Vaginal wall thinning associated with menopausal changes can cause vaginal burning and pain, limitations in sexual function, and vaginal redness or even changes in discharge. Because these symptoms can mimic many other conditions such as pelvic floor muscle dysfunction or an infection, it is necessary for the pelvic rehabilitation therapist to be alert to identifying vaginal atrophy as an issue to rule out so that patients can access appropriate medical care when needed.
 Atrophic vaginitis (AV) is a condition of the vaginal walls associated with tissue thinning, discomfort, and inflammation. The tissue changes often extend into the vulvar area as well. Atrophic vaginitis may also be called vaginal atrophy, vulvovaginal atrophy, urogenital atrophy, or genitourinary syndrome of menopause. Although we tend to associate menopause with women who are in their 40’s or 50’s, any woman who has stopped having her menstrual cycles or who has had a significant reduction in her cycles may be at risk for vaginal atrophy. Any woman who has had a hysterectomy may also be at risk of this thinning of the vaginal walls. Common symptoms of vaginal wall thinning include vaginal dryness, tissue irritation, redness, itching, and a “burning” pain. Interruption in sleep, limitations in activities of daily living, and changes in mood and temperament have also been reported.
Atrophic vaginitis (AV) is a condition of the vaginal walls associated with tissue thinning, discomfort, and inflammation. The tissue changes often extend into the vulvar area as well. Atrophic vaginitis may also be called vaginal atrophy, vulvovaginal atrophy, urogenital atrophy, or genitourinary syndrome of menopause. Although we tend to associate menopause with women who are in their 40’s or 50’s, any woman who has stopped having her menstrual cycles or who has had a significant reduction in her cycles may be at risk for vaginal atrophy. Any woman who has had a hysterectomy may also be at risk of this thinning of the vaginal walls. Common symptoms of vaginal wall thinning include vaginal dryness, tissue irritation, redness, itching, and a “burning” pain. Interruption in sleep, limitations in activities of daily living, and changes in mood and temperament have also been reported.
One common pharmacological intervention for vaginal and vulvar atrophy is the topical application of hormone creams such as estrogen. A recent study examined the effects of low dose estrogen therapy on bacteria that populates the vaginal walls.Shen et al., 2016 This bacteria may be causal or correlated to vaginal health, and also appears related to estrogen levels. Sixty women diagnosed with atrophic vaginitis were treated with low dose estrogen therapy and followed for four weeks to assess the vaginal microbiotia via mid-vaginal swabs. Following are highlights from the linked study’s findings,
- Prior to treatment, in symptomatic postmenopausal women the Lactobacilli species were less abundant and made up 11.2% of the community, while in asymptomatic women, the communities were more than 50% lactobacilli
- Gardnerella was more abundant than Lactobacillus in women with atrophic vaginitis
- Overall diversity of bacterial communities between healthy women and those with atrophic vaginitis was not significantly different
- In response to treatment with estrogen, women with AV reported improved symptoms and decreased vaginal pH
- Serum estradiol improved on average from approximately 42 pmol/L to 168 pmol/L by week 2, with little change from week 2 to week 4
- Lactobacillus count was negatively correlated with symptoms (i.e., more Lactobacillis = less symptoms) and Gardnerella and Atopobium counts were positively correlated with symptoms
- There were variations noted in how each woman’s vaginal bacterial communities responded to the estrogen therapy in that some women had a dominance of other bacteria after 4 weeks even though their symptoms decreased
In conclusion, the authors stated that “…a Lactobacillus-dominated vaginal community may be considered as one of the signs of AV treatment success…” along with reduced symptoms and increased serum estradiol levels. Prior studies have recognized barriers to treatment that include lack of patient knowledge of vulvar and vaginal atrophy, failure to discuss associated symptoms with physicians, concerns about safety of treatments or poor symptom relief with prescribed interventions.Kingsburg et al., 2013 This leaves the pelvic rehabilitation provider in a excellent role of educating women in the signs and symptoms of atrophic vaginitis, observing the tissues for changes, and communicating with referring providers and prescribers if a concern is noted. Furthermore, failure to recognize the potential for vaginal atrophy and treating these tissues with manual therapy or exercise may injure or exacerbate the problem.
Interested in learning more? Keep an eye out for a Menopause Rehabilitation and Symptom Management course with Michelle Lyons!
Changes in the Vagina and Vulva. Retrieved June 27, 2016 from http://www.menopause.org/for-women/sexual-health-menopause-online/changes-at-midlife/changes-in-the-vagina-and-vulva
Kingsberg, S. A., Wysocki, S., Magnus, L., & Krychman, M. L. (2013). Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women's VIews of Treatment Options for Menopausal Vaginal ChangEs) survey. The journal of sexual medicine, 10(7), 1790-1799.
Shen, J., Song, N., Williams, C. J., Brown, C. J., Yan, Z., Xu, C., & Forney, L. J. (2016). Effects of low dose estrogen therapy on the vaginal microbiomes of women with atrophic vaginitis. Scientific reports, 6.
Vaginal Atrophy. Retrieved June 27, 2016 from http://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/home/ovc-20200167
Spending the past 5 years watching a lot of Disney Junior and reading Dr. Seuss, professional journal reading is generally reserved for the sanctuary of the bathroom. When patients ask if I’ve heard of certain new procedures or therapies, I try to sound intelligent and make a mental note to run a PubMed search on the topic when I get home. Making the effort to stay on top of research, however, makes you a more confident and competent clinician for the information-hungry patient and encourages physicians to respect you when it comes to discussing their patients.
A 2016 article in Translational Andrology and Urology, Lin et al., explored rehabilitation of men post radical prostatectomy on a deeper level, trying to prove that brain-derived neurotrophic factor (BDNF) promotes nerve regeneration. In many radical prostatectomies, even when the nerve-sparing approach is used, there is injury to the cavernous nerves, which course along the posterolateral portion of the prostate. Cavernous nerve injury can cause erectile dysfunction in 60.8-93% of males postoperatively. The authors discussed Schwann cells as being vital for maintaining integrity and function of peripheral nerves like the cavernous nerve. They hypothesized that BDNF, a member of the neurotrophin family that supports neuron survival and prevents neuronal death, activates the JAK/STAT (Janus kinase /signal transducer and activator of transcription) pathway in Schwann cells, thus facilitating axonal regeneration via secretion of cytokines (IL-6 and OSM-M). Through scientific experiment on a cellular level (please refer to the article for the specific details), the authors were able to confirm their hypothesis. Schwann cells do, in fact, produce cytokines that contribute to the regeneration of cavernous nerves.
From a different cellular perspective, Haahr et al., (2016) performed an open-label clinical trial involving intracavernous injection of “autologous adipose-derived regenerative cells” (ADRCs) in males experiencing erectile dysfunction (ED) after radical prostatectomy. Current treatments with PDE-5 inhibitors do not give satisfactory results, so the authors performed a human phase 1, single-arm trial to further the research behind the use of adipose-derived stem cells for ED. Some limitations included the study was un-blinded and had no control group. Seventeen males who had ED after radical prostatectomy 5-18 months prior to the study were followed for 6 months post intracavernosal transplantation. The primary outcome was safety/tolerance of stem cell treatment, and the secondary was improvement of ED. The single intracavernosal injection of freshly isolated autologous adipose-derived cells resulted in 8 of 17 men regaining erectile function for intercourse; however, the men who were not continent did not regain erectile function. The end results showed the procedure was safe and well-tolerated. There was a significant improvement in scores for the International Index of Erectile Function-5 (IIEF-5), suggesting this therapy may be a promising one for ED after radical prostatectomy.
In the clinic, we need to treat our patients to the best of our ability. Taking the Post-Prostatectomy Patient Rehabilitation course is vital if even just one patient enters your office seeking treatment. Keeping up on research (even that which seems too full of forgotten science) and learning new manual techniques and exercises can help us rise as clinicians prepared to optimize patients’ function.
Lin, G., Zhang, H., Sun, F., Lu, Z., Reed-Maldonado, A., Lee, Y.-C., … Lue, T. F. (2016). Brain-derived neurotrophic factor promotes nerve regeneration by activating the JAK/STAT pathway in Schwann cells. Translational Andrology and Urology, 5(2), 167–175. http://doi.org/10.21037/tau.2016.02.03
Haahr, M. K., Jensen, C. H., Toyserkani, N. M., Andersen, D. C., Damkier, P., Sørensen, J. A., … Sheikh, S. P. (2016). Safety and Potential Effect of a Single Intracavernous Injection of Autologous Adipose-Derived Regenerative Cells in Patients with Erectile Dysfunction Following Radical Prostatectomy: An Open-Label Phase I Clinical Trial. EBioMedicine, 5, 204–210. http://doi.org/10.1016/j.ebiom.2016.01.024
In case you’ve been under a rock (or maybe studying for the Pelvic Rehabilitation Provider Certification (PRPC) exam, the latest Netflix series starring Maria Bamford is out, and it is, as the kids say, amazeballs. We have Maria Bamford and team, and Lady Dynamite, to thank for getting the term vaginismus out in the public as the title of Season 1, Episode 8. The episode is named “A Vaginismus Miracle.” In this episode Maria is answering the question of when she last had sex. She answers that is was a year ago, which reminds her that the annual date of "Vaginismus" must be coming up. Maria further explains that she must have sex once per year because then everything is good "under the hood", and if she doesn't have sex once a year, her "vagina could close up." It's a nail biter of an episode as Maria's assistant has messed up the schedule, and Maria finds out that "Vaginismus" is that very night, and she must find a partner before midnight.
As a pelvic health provider, I knew that neither myself nor my colleagues would be able to sit back and worry about Maria suffering through another year with “Vaginismus” on her calendar, a looming deadline when we all know that with a little bit of rehabilitation, the issue could be much, much better, or maybe resolved altogether. The episode inspired me to write an open letter to Maria. Feel free to share and tag your friends who you think would love to watch a smart, funny show that puts real life issues including mental health in the spotlight.
![]()
Dear Lady Dynamite,
I recently saw your Netflix show and I have to say that it is brilliant. I love how you weave humor, the messiness of life, and important topics into an unpredictable series of events. You are clearly one smart cookie, but I’m not convinced that your new agent, Karen Grisham, is such a great influence on you (or anyone for that matter).
I wanted to reach out and let you know that, as a pelvic rehabilitation therapist and faculty member at the Herman & Wallace Pelvic Rehabilitation Institute, I really appreciate that you brought the term vaginismus into the big time. So many women suffer needlessly because there is so much that pelvic rehab can do for women like you! It does seem that you have figured out a system that works for you, but what if things hadn’t worked out with Scott that night? Hanging out in a bar hoping that you can find someone to hook up with is just so 80’s. Your condition of vaginismus, a tightening of the muscles around your Lady Dynamite parts, does often cause pain with sex, and that’s called dyspareunia. This is a condition that we pelvic rehab specialists treat every day with a heck of a lot of success. Your new boyfriend Scott (he is still your boyfriend after Thanksgiving and all, right?) could even help you overcome some tenderness and tightness by learning to help you release your vaginal muscle tension. Now if that doesn’t sound like great fodder for some stand-up I don’t know what does!
It’s hard to know sometimes why vaginismus starts, maybe it was the years of freezing temperatures in Duluth that led to your tight muscles, or sliding down Chester Bowl on the ice. Maybe it was spending too much time sitting in a wheelchair while medicated, or caused by medication itself (that happens too- even birth control pills can cause pelvic pain!) My point is, there’s no need to put so much pressure on yourself and have this horrible deadline of “vaginismus” hanging over your head when you can see a kind, smart health care provider about the issue. If you, dear Lady Dynamite, need a referral for a great pelvic rehab therapist in your neighborhood, let us know! We train hundreds of therapists every year, and can help you find the perfect fit (pun intended!) Ha! (We know you can handle a little “adult humor.”) Wishing you all the best, and thanks again for talking about your vagina!
Yours in Pelvic Health,
Holly Tanner
P.S. Good luck with the Pussy Noodles representation!
P.P.S Go ‘Toppers!
P.P.P.S Can’t wait for Season 2!
P.P.P.P.S And if you see Mark McGrath around, say “hi” for me!
![]()
So, dear readers, if you would like to enjoy a smart and really funny show, check out Lady Dynamite. And if you want to learn more about vaginismus, Herman & Wallace offers several courses which would be up your alley. Consider joining faculty member Dee Hartmann, PT, DPT at Vulvodynia: Assessment and Treatment - Denver, CO this October 15-16.
Brady, P. & Hurwitz, M. (Creators). (2016). Lady Dynamite: Season 1, Episode 8. Retrieved from http://netflix.com
Yoga offers a compelling mind-body approach to maternal care that is forward thinking and aligns with the World Health Organization and Institute of Medicine’s recommendations for patient-centered care. But let’s take a look at WHY postpartum care MUST change in order to establish need for the entry of yoga into postpartum care.
Maternal Health Track Record
The United States and similarly developed countries have a very poor track record for postpartum care. The record is so poor that the problem in the US has been labeled a “human rights failure.”1
 On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
Patient satisfaction also suffers under the current model of care, with many more mothers experiencing postpartum depression, a significant risk factor for both mother and baby during and after pregnancy.
The increase in mortality and poor outcomes can, in part, be attributed not to underuse, but overuse of medical intervention during pregnancy and birth. 2,3,4 Countries that have “access to woman-centered care have fewer deaths and lower health care costs”; and, hospital system reviews in the US show that reducing medical interventions are both reducing cost and improving outcomes.1,4,5
The notorious lack of accountability (reporting system) in maternal health care also plagues the US and suggests that maternal deaths are even higher than currently reported, leading to Coeytaux’s conclusion that the “United States is backsliding.”1
Improving Postpartum Outcomes with Integrated Physical Therapy Care
In After the Baby’s Birth, maternal health advocate Robin Lim writes,
"All too often, the only postpartum care an American woman can count on is one fifteen minute appointment with her doctor, six weeks after she has given birth. This six-week marker ends an arbitrary period within which she is supposed to have worked out most postpartum questions for herself. This neglect of postpartum women is not just poor healthcare, it is abusive, particularly to women suffering from painful physical and/or psychological disorders following childbirth."
Physical therapists can be instrumental change agents in improving current postpartum care, especially through the integration of contemplative sciences like yoga. Yoga can be the cornerstone of holistically-driven, person-centered care, especially in comorbid conditions such as pelvic pain and depression, where pharmacological side effects, stigma, can severely diminish adherence to biomedical interventions.6 Coeytaux, as well as other authors, clearly correlate the reduction of maternal mortality with improved postpartum care. The World Health Organization recommends that postpartum checkups should include screening for:
- Back pain
- Incontinence (stress)
- Hemorrhoids
- Constipation
- Fatigue
- Breast pain
- Perineal pain
- Depression
- Painful or difficult intercourse
- Headaches
- Bowel problems
- Dizziness or fainting
 A physical therapist is a vital team member in not only screening for many of the
A physical therapist is a vital team member in not only screening for many of the
listed problems above, but in managing them. It is important to note that other countries, like France, deliver high quality postpartum rehab care plus in-home visits, all while spending far less than the US on maternal care.
The World Health Organization, however, clarifies the vital importance of postpartum care delivery by making a significant recommendation for a paradigm shift in biomedical care.7
Yoga as a “Best Care Practice” for Postpartum Care
The WHO recommends the use of a biopsychosocial model of care, which yoga is ideally suited to provide via its ancient, multi-faceted person-centered philosophy. Medical Therapeutic Yoga is a unique method of combining evidence-based rehabilitation with yoga to emerge with a new paradigm of practice. MTY:
- Addresses the mother as a person, not as a condition or diagnosis.
- Empowers mothers with self-care strategies for systems-based, not just musculoskeletal or neuromuscular, change.
- Addresses all domains of biopsychosocial impairment.
- Teaches interdisciplinary partnership-based theory, which is integral to creative collaborative discourse and innovation in postpartum care.
- Equips clinicians with business service, website development, practice paradigm, and social media campaign tools to fully develop the new clinical niche of Professional Yoga Therapy practice.
- Promotes patient advocacy, health promotion, and public health education via mainstreaming yoga into rehabilitative and medical services.
- Provides the gender context for prescription that traditional yoga is lacking.
- Evolves yoga for use in prenatal and postpartum care.
Physical therapy screening and intervention in the postpartum is vital, but the addition of yoga can optimize postpartum care and has enormous potential to be a “Best Care Practice” for postpartum care in rehabilitation.
As a mind-body intervention, yoga during pregnancy can increase birth weight, shorten labor, decrease pre-term birth, decrease instrument-assisted birth, reduce perceived pain, stress, anxiety sleep disturbances, and general pregnancy-related discomfort and quality of life physical domains.8-9
In addition to the typical physical therapy intervention for postpartum physical therapy, the MTY paradigm provides:
- self-care strategies for psychoemotional health and social engagement, increasing self-efficacy, confidence, and self-worth,
- a concise container for clinical-decision through its algorithmic programming,
- psychoemotional and neuroendocrine intervention,
- nutritional counseling and resource utilization,
- energetic adjunct therapies steeped in Ayurvedic science,
- executive functioning and cognitive support,
- epigenetic effect, and
- inter- and intrarelational development.
Postpartum integrated physical therapy care can provide more comprehensive care than rehab alone because of its multi-faceted biopsychosocial structure and systems-based model of care. Ginger’s course, Yoga as Medicine for Labor, Delivery, and Postpartum provides evidence-based methodology for prenatal and postpartum practice that streamlines clinical decision-making and intervention through introduction of a yogic model of assessment.
To learn more about Ginger’s course, visit Yoga as Medicine for Labor, Delivery, and Postpartum
Coeytauz et al., Maternal Mortality in the US: A Human Rights Failure. Contraception Editorial, March 2011. http://www.arhp.org/publications-and-resources/contraception-journal/march-2011
Kuklina E, Meikle S, Jamieson D, et al. Severe obstetric morbidity in the US, 1998–2005. Obstet Gynecol. 2009;113:293–299.
Tita ATN, Landon MB, Spong CY, et al. Timing of elective cesarean delivery at term and neonatal outcomes. NEJM. 2009;360:111–120.
Clark SL, Belfort MA, Byrum SL, Meyers JA, Perlin JB. Improved outcomes, fewer cesarean deliveries, and reduced litigation: results of a new paradigm in patient safety. Am J Obstet Gynecol. 2008;199:e1–105.e7.Abstract | Full Text | Full-Text PDF (100 KB)
Oshiro BT. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113:804–811.
Buttner, M. M., Brock, R. L., O'Hara, M. W., & Stuart, S. (2015). Efficacy of yoga for depressed postpartum women: A randomized controlled trial. Complementary Therapies in Clinical Practice, 21(2), 94-100. doi:10.1016/j.ctcp.2015.03.003 [doi]
WORLD HEALTH ORGANIZATION., 2002. Towards a common language for functioning, disability and health : ICF. Geneva: World Health Organisation.
Curtis, K., Weinrib, A., & Katz, J. (2012). Systematic review of yoga for pregnant women: Current status and future directions. Evidence-Based Complementary and Alternative Medicine : ECAM, 2012, 715942. doi:10.1155/2012/715942 [doi]
Sharma, M., & Branscum, P. (2015). Yoga interventions in pregnancy: A qualitative review. Journal of Alternative and Complementary Medicine (New York, N.Y.), 21(4), 208-216. doi:10.1089/acm.2014.0033 [doi]
Danielle is among the latest class of Certified Pelvic Rehabilitation Practitioners! Her experience treating patients and owning Core 3 Physical Therapy prepared her to pass the exam in flying colors. Read her bio here and check out our interview below. Congratulations, Danielle!
 What/who inspired you to become involved in pelvic rehabilitation?
What/who inspired you to become involved in pelvic rehabilitation?
A patient was the first one to inspire me to improve my knowledge and treatment abilities in pelvic rehabilitation. I was working with a postpartum patient, while carrying my first child, and she felt that my guidance had been so helpful in her care that it made me interested learning more about the pelvic floor. Most of my fellow colleagues could discuss my orthopedic questions but I didn’t have any mentors that could offer advice in more advanced pelvic floor cases so I started attending the Herman and Wallace classes. They have been an invaluable at improving my ability to care for patients with pelvic pain which has even improved my treatment of orthopedic patients with low back pain and sacroiliac dysfunction.
What patient population do you find most rewarding in treating and why?
I enjoy working with chronic pelvic pain patients because it's rewarding to be able to bring relief to someone who has been living with pain, limited quality of life or even social anxiety and has not received any benefit with other treatment options. Being able to help this patient population understand the pelvic floor muscles and function as well as providing justification to why they are in pain and then help them progress through various treatment approaches makes my job rewarding.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
PT's are uniquely trained to provided internal pelvic floor muscle release. This is something that no other health care professional is licensed or has the schedule/time to perform. This technique can provide relief and feedback to your patients that is possible in no other way. If you do not want to address this region or feel comfortable providing this treatment, find a therapist local to you who has experience with pelvic floor and refer when appropriate. Additionally, we as physical therapists are often the first line of defense in recognizing and educating patients about the ability to address a wide variety of symptoms that they believe is "just a normal part of life". Asking the in-depth questions and providing a multimodal approach to their symptoms is not only a boon to the patient but to our profession.
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
"Your most valuable tool is your finger." It is rare to treat an orthopedic patient without incorporating any hands on approach and the same holds true for the pelvic floor. With an internal exam you can make your most accurate assessment while providing valuable feedback to the patient.
What makes you the most proud to have earned PRPC?
I think it has helped me gain respect with my fellow health care professionals for my expertise in the area of pelvic floor treatment. It has broadened my knowledge base and provided me a strong guide for furthering my ability to treat patients with pelvic pain and dysfunction.
What is in store for you in the future?
I would like to become involved in research to further evidence based evaluation and treatment of pelvic conditions. I hope to facilitate the effectiveness and value in pelvic floor rehabilitation via physical therapy.
What role do you see pelvic health playing in general well-being?
It should become a staple for all pelvic floor surgeries just like a physical therapy is the staple post total knee surgery. Currently in my region I find it very underutilized despite the research behind our treatment. This is largely due to the general population not being aware of the treatment benefits physical therapy can play in pelvic dysfunction. European countries make it a standard of care in this area and I hope we progress to adopt a similar view of treatment.
More than a year ago, after working on updating the pelvic floor series courses PF1, 2A and 2B, the Institute turned our attention to the final course in our popular series, PF3. To determine what content our participants wanted to learn about in the last continuing education course of the series, we asked that exact question. From a large survey of therapists who had taken all or most of the courses in the pelvic core series, we collected detailed data from therapists about what was needed to round out their comprehensive training. The results of that survey guided hundreds (and hundreds!) of hours of work completed by a team of instructors. This month, in the beautiful city of Denver, the three instructors who created the Capstone course will share their wisdom, clinical experiences, as well as their thoughtfully-designed lectures and labs. You will have an opportunity to learn in depth about topics covered in the prior courses in the series.
Such topics include lifespan issues and health issues common to different ages, conditions of polycystic ovarian syndrome, endometriosis, infertility, pelvic organ prolapse and surgeries, pelvic fascial anatomy, pharmacology and nutrition. Lab components are detailed and comprehensive for working with specific common implications from conditions in pelvic dysfunction or surgery. This course focuses on the female pelvis, including diving into the complexities of female pelvic health issues. The instructors have all worked in the field for many years, are experienced in working with complex patient presentations, and all excel at manual therapies. I asked each of them to briefly share thoughts about the Capstone course that they each dedicated the last year in developing; following you can read their thoughts.
 "I'm excited for every therapist who will take this course, as it is made to help you approach your practice at a whole new level. We are eager to help your hands work dynamically with more intelligence and how to tackle complex restrictions in the pelvis and abdomen that go far beyond releasing muscles. Additionally, the practitioners will raise their capacity of recognizing and helping the patient manage complex conditions, such as endometriosis, PCOS, fibroids, and IBS."
"I'm excited for every therapist who will take this course, as it is made to help you approach your practice at a whole new level. We are eager to help your hands work dynamically with more intelligence and how to tackle complex restrictions in the pelvis and abdomen that go far beyond releasing muscles. Additionally, the practitioners will raise their capacity of recognizing and helping the patient manage complex conditions, such as endometriosis, PCOS, fibroids, and IBS."
 "One of the best things about the Capstone course is that it provides the participants tools to treat more complicated patients. Topics such as endocrinology, oncology, vulvar dermatology, and surgical procedures are addressed, which will complete the picture for some of those patients that are hard to treat due to the complexity of their case. This knowledge, along with more advanced manual treatment techniques, will add to the skill set of the participants to improve their treatment outcomes. I am excited for the participants to combine their current clinical skills along with some new knowledge and techniques to be able to treat the whole person when working with complex and challenging patients."
"One of the best things about the Capstone course is that it provides the participants tools to treat more complicated patients. Topics such as endocrinology, oncology, vulvar dermatology, and surgical procedures are addressed, which will complete the picture for some of those patients that are hard to treat due to the complexity of their case. This knowledge, along with more advanced manual treatment techniques, will add to the skill set of the participants to improve their treatment outcomes. I am excited for the participants to combine their current clinical skills along with some new knowledge and techniques to be able to treat the whole person when working with complex and challenging patients."
 "Designing and creating Capstone with Nari and Allison was an incredible experience. My own knowledge and clinical expertise grew profoundly while researching and writing this material. Capstone is designed to really take the experienced pelvic health therapist to the next level of understanding and treating more complex patients. I can't wait to see the impact this material has on participants and their patients."
"Designing and creating Capstone with Nari and Allison was an incredible experience. My own knowledge and clinical expertise grew profoundly while researching and writing this material. Capstone is designed to really take the experienced pelvic health therapist to the next level of understanding and treating more complex patients. I can't wait to see the impact this material has on participants and their patients."
There is still time to register for the few remaining seats in Denver this weekend!
Appropriate sun exposure and/or daily supplements provide our bodies with sufficient amounts of Vitamin D. I would venture to guess almost every one of the patients I treated in Seattle had a deficiency of Vitamin D if they were not taking a supplement. Running outside year round has always kept my skin slightly tan and my levels of Vitamin D healthy; however, when I was pregnant in the Pacific Northwest, I had to supplement my diet with Vitamin D, which was a first for this East Coast beach girl. The benefit of Vitamin D has spread beyond just bone health, with studies showing its impact on pelvic floor function.
Parker-Autry et al., (2012) published a study discerning the Vitamin D levels in women who already presented with pelvic floor dysfunction versus “normal” gynecological patients. The retrospective study involved a chart review of 394 women who completed the Colorectal Anal Distress Inventory (CRADI)-8 and the Incontinence Impact Questionnaire (IIQ-7). These women all had a total serum 25-hydroxy Vitamin D [25(OH)D] drawn within one year of their gynecological visit. The authors defined a serum 25(OH)D of <15ng/ml as Vitamin D deficient, between 15-29ng/ml as Vitamin D insufficient, and >30ng/ml as Vitamin D sufficient. In the pelvic floor disorder group comprised of 268 women, 51% were found Vitamin D insufficient, 13% of whom were deficient. The CRADI-8 and IIQ-7 scores were noted as higher among the Vitamin D insufficient women. Overall, the mean 25(OH)D levels in the women without pelvic floor issues were higher than those who presented with pelvic floor disorder symptoms.
Another case-control study in 2014 by Parker-Autry et al., focused on the association between Vitamin D deficiency and fecal incontinence. They considered 31 women with fecal incontinence versus a control group of 81 women without any pelvic floor symptoms, looking at serum Vitamin D levels. The women with fecal incontinence had a mean serum Vitamin D level of 29.2±12.3 ng/ml (insufficient/deficient), while the control group had a higher mean level of 35±14.1 ng/ml (sufficient). The women completed the Modified Manchester Health Questionnaire and the Fecal Incontinence Severity Index, and women with deficient Vitamin D scored higher on the questionnaire, indicating fecal incontinence as a burden on quality of life. The severity scores were higher for Vitamin D deficient women, but there was not a statistically significant difference between the groups. Once again, the pelvic floor disorder and Vitamin D deficiency correlation prevailed in this study.
An even more recent study looked at postmenopausal women and Vitamin D deficiency (Navaneethan et al., 2015). This prospective case control study involved 120 postmenopausal women, 51 of whom had pelvic floor disorders. The serum 25-hydroxy Vitamin D levels were obtained, and the results revealed a deficiency in those women with pelvic floor dysfunction. Vitamin D levels were found to be significantly lower in women who were 5 years or more into menopause. Overall, Vitamin D was deemed a worthy factor to consider in the pelvic floor disorder population as well as in postmenopausal women.
Taking time to talk to patients about their lifestyle, daily supplements, and diet can often shed light on their ability to benefit from our treatments. If a Vitamin D deficiency sounds possible, discuss current research with them and suggest they get their serum Vitamin D levels checked. Don’t underestimate the power of a little sunshine – it just might have a positive impact on pelvic floor health.
Parker-Autry, C. Y., Markland, A. D., Ballard, A. C., Downs-Gunn, D., & Richter, H. E. (2012). Vitamin D Status in Women with Pelvic Floor Disorder Symptoms. International Urogynecology Journal, 23(12), 1699–1705. http://doi.org/10.1007/s00192-012-1700-8
Parker-Autry, C. Y., Gleason, J. L., Griffin, R. L., Markland, A., & Richter, H. E. (2014). VITAMIN D DEFICIENCY IS ASSOCIATED WITH INCREASED FECAL INCONTINENCE SYMPTOMS. International Urogynecology Journal, 25(11), 1483–1489. http://doi.org/10.1007/s00192-014-2389-7
Navaneethan, P. R., Kekre, A., Jacob, K. S., & Varghese, L. (2015). Vitamin D deficiency in postmenopausal women with pelvic floor disorders. Journal of Mid-Life Health, 6(2), 66–69. http://doi.org/10.4103/0976-7800.158948
The American Society of Clinical Oncology convened their 2016 annual meeting over the weekend, and several of the presentations suggest new methods of preventing breast cancer recurrence.
Extended Hormone Therapy Reduces Recurrence of Breast Cancer
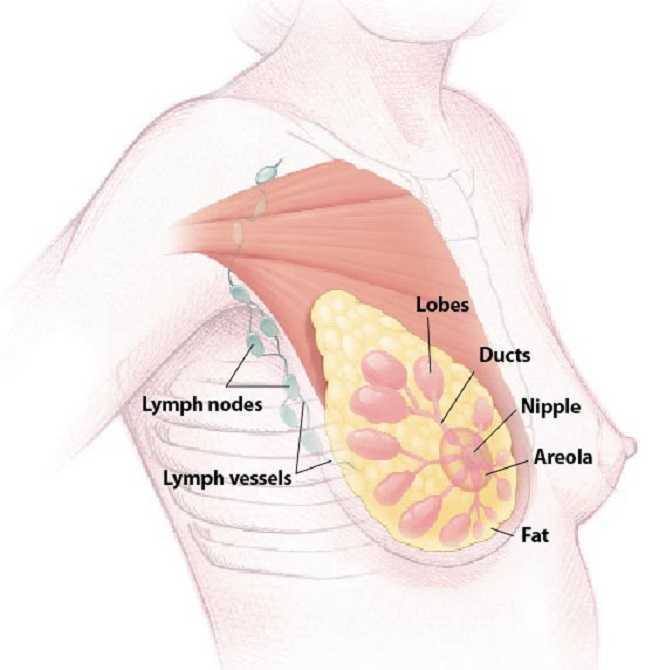 Breast cancer patients who are treated with aromatase inhibitor therapy are generally prescribed the the estrogen drugs for a five year course. A new study has suggested that by doubling the length of hormone therapy, the recurrence rate for breast cancer survivors drops by 34%. The study included 1,918 women who underwent five years of hormone therapy with the drug letrozole. After five years, half of the group switched to a placebo while the other half were given an additional five year treatment.
Breast cancer patients who are treated with aromatase inhibitor therapy are generally prescribed the the estrogen drugs for a five year course. A new study has suggested that by doubling the length of hormone therapy, the recurrence rate for breast cancer survivors drops by 34%. The study included 1,918 women who underwent five years of hormone therapy with the drug letrozole. After five years, half of the group switched to a placebo while the other half were given an additional five year treatment.
Drug Used to Treat Type 2 Diabetes May Increase Breast Cancer Survivability
The Univerisity of Pennsylvania School of Medicine has published results from two recent studies which document the effects of Metformin, a drug commonly used to treat type 2 diabetes, on breast cancer and endometrial hyperplasia. The study tracked outcomes for 1,215 patients who were diagnosed and surgically treated for breast cancer. Patients who began to use metformin after their diagnosis were found to have a 50% higher survivability rate than those who did not use metformin.
The timing of metformin use is extremely important when it comes to breast cancer survivability rates. The study also found that patients who used metformin prior to their diagnosis were more than twice as likely to die than those who never used the drug.
Research Suggests a "Mediterranian Diet" May Reduce Breast Cancer Recurrence
A study has indicated that a diet rich in vegetables, fish, and olive oil may decrease the odds of a breast cancer survivor experiencing a relapse or recurrence of their cancer. The study tracked 300 women with early-stage cancer and found that those who ate a normal diet were more likely to experience a breast cancer recurrence. The findings build upon previous research which indicated that a Mediterranean diet, and especially extra virgin olive oil, could reduce breast cancer risk by 68%.
Want to Learn More?
Susannah Haarmann, PT, CLT, WCS is the author and instructor of Physical Therapy Treatment for the Breast Oncology Patient, a course offered through the Herman & Wallace Institute. This continuing education course for medical practitioners offers a rehabilitation perspective for providers who work with oncology rehabilitation patients. Join Dr. Haarmann this in Stockton, CA on September 24-25 to learn evaluation and treatment techniques necessary to make an outpatient therapist an essential member of any oncology team.
1) Paul E. Goss, et al. J Clin Oncol 34, 2016 (suppl; abstr LBA1)
https://www.asco.org/about-asco/press-center/news-releases/ten-years-hormone-therapy-reduces-breast-cancer-recurrence
2) Yun Rose Li. University of Pennsylvania, American Society of Clinical Oncology Annual Meeting 2016
http://www.eurekalert.org/pub_releases/2016-06/uops-ddm060316.php
3) http://www.scienceworldreport.com/articles/41404/20160606/mediterranean-diet-prevent-breast-cancer-recurring.htm
When a 472 pound gentleman recently arrived for an evaluation for low back pain, he came to the clinic for me to help him, not deride him about his weight (which he complained all his doctors have already done). He claimed he had lost 120 pounds but gained back 50, and his low back was extremely painful with transitional movements and daily function. Undoubtedly, this man’s body was a battlefield for inflammation, and no matter how much manual therapy or exercise I implemented, nutrition education seemed vital. Instead of just chatting about baseball or the weather, competently sharing what we’ve studied and learned in continuing education courses is warranted in our practice.
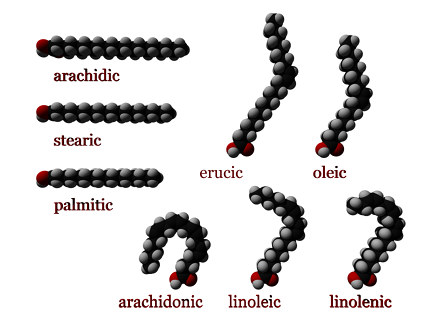 In a 2016 review Klek reveals the most current evidence regarding Omega-3 Fatty Acids in nutrition delivered intravenously. Although physical therapists do not decide the ingredients for patients’ parenteral nutrition, the article thoroughly explains the essential benefits of fatty acids. Aside from being important structural components of cell membranes and precursors of prostaglandins and cholesterol, fatty acids regulate gene expression and adjust pathways of cells regarding inflammation and cell-mediated immune responses. Ultimately, fatty acids modulate metabolic processes in the body, whether locally, in a particular region, or at remote sites. Omega-3 fatty acids have been shown to inhibit synthesis of triglycerides by the liver, prevent cardiovascular disease, reduce cancerous cell growth, and even affect the development of rheumatoid arthritis and Chrohn’s disease. This article not only sheds light on parenteral nutrition for post-surgical, oncology, critically ill, and even pediatric patients but also educates the healthcare professional on the impact fatty acids have on the patients we treat.
In a 2016 review Klek reveals the most current evidence regarding Omega-3 Fatty Acids in nutrition delivered intravenously. Although physical therapists do not decide the ingredients for patients’ parenteral nutrition, the article thoroughly explains the essential benefits of fatty acids. Aside from being important structural components of cell membranes and precursors of prostaglandins and cholesterol, fatty acids regulate gene expression and adjust pathways of cells regarding inflammation and cell-mediated immune responses. Ultimately, fatty acids modulate metabolic processes in the body, whether locally, in a particular region, or at remote sites. Omega-3 fatty acids have been shown to inhibit synthesis of triglycerides by the liver, prevent cardiovascular disease, reduce cancerous cell growth, and even affect the development of rheumatoid arthritis and Chrohn’s disease. This article not only sheds light on parenteral nutrition for post-surgical, oncology, critically ill, and even pediatric patients but also educates the healthcare professional on the impact fatty acids have on the patients we treat.
In 2015, Haghiac et al. performed a randomized double-blind controlled clinical trial to determine if Omega-3 fatty acid supplementation could reduce inflammation in pregnant woman who are obese. Although the study began with 36 subjects in each group, only 24 women in the experimental group receiving 4 capsules a day of Omega-3 fatty acid (total of 2000mg) and 25 of the women taking 4 placebo capsules a day completed the supplementation over the 25 weeks up until delivery. The authors referenced the findings that low grade inflammation becomes exacerbated in obese pregnant women. While an excess of Omega-6 fatty acids practically promotes inflammation via eicosanoid (hormone) production, a healthy balance of Omega-3 fatty acids lessens inflammatory and immunosuppressive eicosanoid production. This study demonstrated an improvement in inflammation in the women who took the Omega-3 fatty acid as evidenced by a decrease in the expression of inflammatory genes in adipose tissue and placenta as well as reduced plasma C-reactive protein (CRP) at delivery.
Being able to control or reduce inflammation on a cellular level through nutrition could promote an exciting cycle of positive events for obese patients. Decreased inflammation in the body could decrease pain, which could allow and even promote increased activity and likely boost metabolism to equip them to battle obesity. The “Nutrition Perspectives for the Pelvic Rehab Therapist” course should spark the interest of any therapist wanting to guide patients not only on movement and function but also on the appropriate nutrition that best facilitates the body’s ability to heal and perform.
To learn more about nutrition and it's effects on pelvic rehabilitation, check out Nutrition Perspectives for the Pelvic Rehab Therapist this month in Lodi, CA.
Klek, S. (2016). Omega-3 Fatty Acids in Modern Parenteral Nutrition: A Review of the Current Evidence. Journal of Clinical Medicine, 5(3), 34. http://doi.org/10.3390/jcm5030034
Haghiac, M., Yang, X., Presley, L., Smith, S., Dettelback, S., Minium, J., … Hauguel-de Mouzon, S. (2015). Dietary Omega-3 Fatty Acid Supplementation Reduces Inflammation in Obese Pregnant Women: A Randomized Double-Blind Controlled Clinical Trial. PLoS ONE, 10(9), e0137309. http://doi.org/10.1371/journal.pone.0137309
Congratulations to Jane Blair Johe, PT, PRPC on becoming one of the newest Certified Pelvic Rehabilitation Practitioners! Read our interview with Blair below.
 Tell us about your clinical practice
Tell us about your clinical practice
I work in a free standing outpatient PT center of a large 4 hospital affiliation. 70% lymphedema 30% pelvic floor rehab.
How did you get involved in the pelvic rehabilitation field?
I was already the lymphedema PT (LANA cert.) when I moved to WV. The women's health PT was moving to another state and asked me to please pick up her bladder incontinence patients.
What patient population do you find most rewarding in treating and why?
I do like pelvic pain clients as I can work with other PT’s on staff to problem solve . Both patients and their doctors are so grateful.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
That you cannot ignore a very important group of muscles (PF) whether you are treating backs, hips etc. or pain and weakness or balance issues…. it plays such a vital role in wellbeing. Any of these clients should be questioned about bowel and bladder issues.
What has been your favorite Herman & Wallace Course and why?
I took my first course from them in September and was so impressed (compared to other courses)
What lesson have you learned from a Herman & Wallace instructor that has stayed with you?
the PT pelvic floor assessment. Correct postures , breathing and “safe” effort of bowel movements.
What do you find is the most useful resource for your practice?
MedBridge Courses
What motivated you to earn PRPC?
If I only had one pelvic floor referral, I would like to give the best service possible to that client. My referring MD’s are very happy too.
What makes you the most proud to have earned PRPC?
I thought it was a many faceted subject and combined many aspects of my 45 years of physical therapy practice. It made me feel that I do know my profession that I love.
What advice would you give to physical therapists interested in earning PRPC?
Have a broad back ground in multiple areas of PT then I highly recommend Herman and Wallace courses as the best path.
What is in store for you in the future?
A urologist in town contacted me today to set up referring for pre surgery PT (prostate surgery).
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./










































