The following comes to us from faculty member Allison Ariail. Allison teaches several courses for the Institute, her next one being Rehabilitative Ultrasound Imaging in Baltimore, MD on June 12-14. There is still room, so sign up today!

Living in Colorado, I come across a lot of individuals who are avid runners, cyclists, or triathletes. Even with a higher level of fitness, these individuals will at times have back pain. What is going on in these physically fit, strong individuals? This is what Rostami et al.[1] set out to determine in their recent study. Using ultrasound imaging, they measured the thickness of the transversus abdominis, internal oblique, external oblique, and the cross sectional area of the multifidus while laying down as well as while mounted on a bicycle. They also measured the back strength, endurance, and flexibility of off-road cyclists with and without back pain. Fourteen professional competitive off-road cyclists with low back pain were compared to 24 control. Results showed a significantly thinner transversus abdominis, and cross sectional area of the multifidus muscle in the cyclists with back pain. There was no significant difference found in flexibility or isometric back strength between the two groups. However the cyclists with low back pain demonstrated decreased endurance in back dynamometry with 50% of their maximum isometric back strength.
The results of this study are consistent with other studies that examined less athletic individuals; thinner transverseus abdominis, and smaller multifidus muscles. This further reinforces the training of the local stabilizing muscles. What does this training method consist of? Learning to isolate each of the local stabilizing muscles; the transversus abdominis, the multifidus, and the pelvic floor muscles. Once a patient is able to isolate a contraction, challenge the muscles by holding a contraction while breathing normally, or holding the contraction while performing motor tasks such as Sahrmann’s exercises. Progress the patient so they are able to perform contractions in weight bearing positions and co-contractions of the muscles. Finally, progress the patient to maintaining co-contractions during functional activities and exercise activities. This will improve stability of the back and pelvis as well as decrease the pain experienced by the patient.
Even patients with higher levels of activity and physical fitness can benefit from a program such as this one. I have used this treatment protocol using ultrasound imaging to confirm and train the local stabilizing muscles on individuals who are both active as well as with individuals not able to participate in as much physical activity. Each and every patient has made gains, even patients who already had a higher level of activity and sports participation such as cyclists, runners, and triathletes. It is rewarding to see all patients make gains and improvements!
[1]Rostami M, Ansari M, Noormohammadpour P et al. Ultrasound assessment of trunk muscles and back flexibility, strength and endurance in off-road cyclists with and without back pain. J Back Musculoskelet Rehabil. 2014; Nov.
According to the online resource www.celiac.org celiac disease (also called celiac sprue or gluten sensitive enteropathy) is an autoimmune disorder in which the ingestion of gluten can damage the small intestine. It is further described as an autoimmune disorder affecting 1 in 100 people worldwide and a disorder that can occur among "genetically predisposed people." Common signs and symptoms include abdominal bloating and pain, chronic diarrhea, vomiting, constipation, weight loss, fatigue, irritability and behavioral issues, dental enamel defects, delayed growth, failure to thrive, and ADHD. If not treated, long-term consequences may include developing other disorders such as Type I diabetes, multiple sclerosis, dermatitis herpetiformis (itchy rash), anemia, osteoporosis, infertility, epilepsy, migraines, and intestinal cancers.
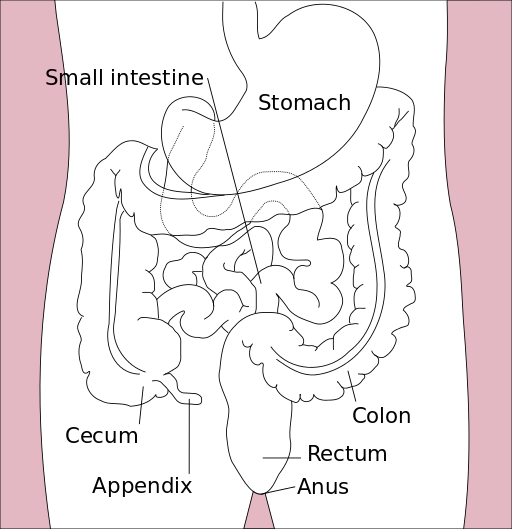
Last year, in the Journal of Family Practice, an article was published describing "Why celiac disease is so easy to miss" the authors point out that less than half of patients present with GI symptoms. An unexplained symptom, iron deficient anemia, may be a clue that a patient needs to be tested for celiac disease. Other conditions, such If a patient has a 1st degree relative with celiac disease, presents with autoimmune thyroid disease, peripheral neuropathy, recurrent migraine, chronic fatigue, osteopenia/osteoporosis, or elevated liver enzymes. (See the linked article for further considerations for testing.) Blood serum tests can help determine the presence of celiac disease, and other tests such as an intestinal biopsy or response to a gluten-free diet can be used to confirm the condition. Adherence to a gluten free diet is critical for a patient with celiac disease, and if you are currently (or have tried) eating a gluten free diet, you know how challenging that may be because gluten is in so many products including sources such as vitamins, medications, and lipsticks! If your patient has been diagnosed recently with celiac disease, referral to a nutritionist may be an excellent part of the patient's plan.
While we might imagine that a patient who has a genetic susceptibility for celiac disease would be diagnosed long before we first see them in the clinic, patients can have a "triggering event" such as a trauma, infection, or severe stress that triggers an onset of the disease. And because of the common gastrointestinal symptoms that are present, a patient with undiagnosed celiac disease may be found in our clinical practice. If you would like to learn more about how celiac disease can affect our patients, those diagnosed or undiagnosed, check out the Institute's new course on Nutrition Perspectives for the Pelvic Rehab Therapist, instructed by Megan Pribyl who earned degrees in both nutrition and exercise science. The course taking place in Seattle this weekend has a few last-minute spots for you to attend, and if you'd like to host this course, contact us at the Institute!
Patients and practitioners alike can benefit from meditation and mindfulness training for the rehabilitation setting. Nari Clemons joined us today to discuss her upcoming Meditation for Patients and Practitioners course taking place in New York.

We all live in a fast paced world. Our smart phones are letting us know to get back to people with email or texts, we have busy practices with full days, and many of us also have care-giving to do when we get home. Many practitioners see chronic pain patients, sometimes with abuse history or a history of many years of failed medical care. Our patients come to us stressed out and ready to unload, and this happens all day long.
We know our pelvic patients would do better to calm their system. We go home at night so drained sometimes. We would do better to regulate our system. But how? We are all so busy. In Meditation for Patients and Practitioners, we focus on the therapist as well as the patient.
Perhaps you have tried meditation for yourself or your patient. Perhaps you didn’t respond to imagining a waterfall or counting your breath, and you gave up. Perhaps your patient didn’t really take to it, or you can’t figure out how to fit it into your sessions. So many of us know that we are tired of our own low level anxiety, or that our patients would do better if we could get them to re-frame mentally. However, when it comes to implementing those changes, we often come up at a loss.
A randomized control study[1] of nurse leaders who work in understaffed environments were tested with a workplace meditation program. Stress scores were tested at baseline and one week after completing a 4 week program. What do you know? The participants had a decrease in distress scores and an increase in positive symptoms.
“But my day is too busy,” you think? In this course, we work on strategies to center yourself at the beginning of your day, the end of your day, or during your day with 1, 2, or 5 minute strategies. This way, even on your busiest days, you have a way to reel in your stress level and find your calm. For your patients, we offer around 10 different techniques.
When teaching PF1, PF2A and PF2B, we talk about the need to downtrain the nervous system to be effective with pelvic pain, constipation, and history of trauma. Yet, the question always arises about which technique to use with a patient. In the Meditation for Patients and Providers course we give you a working model of how to choose a technique for your patient depending on the time you have, the patient personality, and the situation you are working on resolving.
As one participant said after the last course, “Excellent course. No other course has so beautifully described such practical techniques that are just as important for the therapist’s mental health as they are for the patient’s”. Sound exciting? Join us at the Meditation for Patients and Practitioners course being offered July 19-20 in New York City.
[1]Bazarko, Dawn et al. “The Impact of an Innovative Mindfulness-Based Stress Reduction Program on the Health and Well-Being of Nurses Employed in a Corporate Setting." Journal of Workplace Behavioral Health 28.2 (2013): 107–133. PMC. Web. 2 June 2015.

The following is contributed by faculty member Ginger Garner, who teaches the Hib Labrum Injury course. You can read more about that course on the Herman & Wallace course page.
Hip labral injury (HLI) is a relatively new diagnosis in the last 10 years of orthopaedic and rehabilitative care. However, just because HLI is a new diagnosis doesn’t mean the injury is new. In fact, HLI is posited to be responsible for the premature aging and osteoarthritis of the hip joint and pelvis that leads to hip replacements. HLI is also a major source of hip pain, with groin pain being the most common subjective complaint.However, groin pain is not the only complaint that is associated with HLI. Pelvic pain commonly goes hand-in-hand with hip pain.
What does this mean for patients? If you have hip or pelvic pain you should be evaluated by an HLI specialist, which can be a PT, surgeon, or osteopath who has received additional training on managing HLI. It is critical that you see someone who specializes in HLI. If HLI or other hip or pelvic injury is suspected, it is important that you follow up with a physical therapist who has had advanced training in HLI rehab for the best chance of recovery.
I find the premenstrual cycle pain (usually 1-5 days before the cycle begins) is a common phenomenon with many women with HLI (operative and non-operative), which is an area that needs more attention in research. Some women say it feels like they have retorn their labrum, and as a result, they get fearful – which affects not just their physical functioning but their psychoemotional and social well-being.
They limit activity which can exacerbate faulty neuromuscular patterning and deconditioning and result in increased pain from faulty structural support. Their realm of social activity and self-efficacy can suffer, which is also not good for long-term well-being.
Additionally, sleep can be interrupted with HLI and pelvic pain, which can dysregulate the HPA (hypothalamic pituitary adrenal) Axis and cause further problems with issues like pain centralization, cortisol dysregulation, and digestion. A recent study correlated vulvodynia and FAI (femoracetabular impingement), a type of hip impingement commonly found with HLI. The study found that those women who received early surgical intervention received the most relief from vulvodynia, while those who had a longer duration of pain did not experience the same level of improvement.
The take-home message is that early intervention for HLI is absolutely critical for the best long-term prognosis, and that pelvic pain, which can include anything from vulvodynia, dyspareunia, interstitial cystitis, non-relaxing pelvic floor/myalgia, pudendal neuralgia or entrapment, athletic pubalgia, and/or continence issues, although a common occurrence with HLI, is not normal and should be addressed by a trained pelvic rehab professional.
Want more? Read my post about Hip Labrum Tear Risk: Why Early Care is Critical, is absolutely necessary for the best long-term prognosis.
Physical therapist, educator, researcher, and clinical instructor Daniel Kirages, who was mentioned in Do Male Therapists Belong in Pelvic Rehab: Part I, shares his viewpoint from the perspective of his various roles.

“As a male, how did you get involved in pelvic rehab?” This is a question I have been asked countless times and the answer can be pretty simple, I usually say “It’s really not much different than any other musculoskeletal related issue. I’m just not afraid of working below the belt.” Working within the domain of neuro-musculo-skeletal physical therapy offers an endless supply of opportunities. Pelvic rehab is just one subcategory amongst many and this can be further subdivided into several categorizations as well – incontinence, voiding dysfunction, pain, etc. Despite a heavy dose of specialized knowledge necessary for these topics, ultimately we view the patient/client using a similar lens as any neuro-musculo-skeletal condition. This would include the need to examine and intervene for identified deficits in motor coordination, mobility, flexibility, strength, awareness and knowledge. Therefore, all PTs are primed to enter the world of pelvic rehab and they should consider “uploading the mental software” of pelvic specific knowledge by taking courses and finding a mentor to get started.
Being a male within what is typically considered a female related health domain never really bothered me. It just made me witness what a great opportunity it is and how I can be somewhat unique with my practice because there was and still is a need for more male PTs to be involved in pelvic rehab. Early on in my career I would see more females than I do now because our clinic needed the coverage and I wanted to use all aspects of the pelvic related knowledge I acquired. There was never an issue because the patients were willing to work with me; it was not a big deal to them because most of the time a male physician referred them to me in the first place. I would protect myself from any concerns by having a female aide or student be my chaperone in the room. This way a witness was present. It was not a burden on the clinic in any way, and actually the chaperones reported feeling very enlightened about what I do and I believe having a chaperone comforted the patient as well. The male patients I treat are so grateful and many express how they would be uncomfortable with a female therapist although they would go "if they had to". Of course, we as the practitioners know that the care offered by a PT of any gender will be therapeutic and professional, but the patient would not know until they had a positive experience. Some of my patients have avoided going to PT for their pelvic dysfunction until they discovered they can see a male PT. Unfortunate, but true.
The sheer number of people experiencing pelvic health related disorders speaks to the need for competent PTs to help them, but we have competition from urologic nurses, occupational therapists, Pilates instructors, personal trainers amongst others. However, we as PTs are most equipped to serve this population because of our educational backgrounds in manual therapy, exercise physiology, systems physiology and the priceless ability to take time to educate our patients. So the door is open for all of us to get involved and join the world of pelvic rehab which is why I try to make a push to incorporate pelvic rehab topics within entry-level DPT programs. We are making some gains in select programs, but without the PT board exam or the school credentialing agencies seeing value in pelvic rehab it will not change rapidly. The last several years there has been at least one male student applying each semester for a 16-week clinical affiliation with me for a hybrid ortho/male pelvic health experience. As long as there are more PTs offering this exposure to male students we will soon be populating the pelvic rehab world with a bit more testosterone, which can only be a good thing.
Today’s contribution to the Pelvic Rehab Report comes from Allison Ariail, the instructor for Herman & Wallace’s Rehabilitative Ultrasound Imaging courses. Join Allison and others this June 12-14 at Rehabilitative Ultra Sound Imaging: Women's Health and Orthopedic Topics - Baltimore, MD!
Is an Ultrasound that provides images of the pelvic floor and other deep musculature a cool gadget to have in the office or something that is truly essential? That depends on who you are asking! If you know how to use Ultrasound imaging properly and market yourself and your practice accordingly, it can become a tool that is not only fun to have and handy to use clinically, but also essential to providing your most efficient and thorough care!
Using an ultrasound (US) machine allows you to view the deeper musculature to assess how the muscles are functioning. The most common muscles assessed with US imaging are the transverse abdominis, the multifidus, and the pelvic floor. The patient then can use what is seen on the US screen as biofeedback to retrain their strategy and timing of recruitment. The therapist can also assess the patient’s ability to activate and maintain a contraction in various positions and even during motor tasks as well. This type of biofeedback is not only useful for pelvic floor patients, but is also important for patients with back and sacroiliac joint pain. Research is showing that using this type of stabilization program is making a difference in athletes. Julie Hides has published two articles recently showing that this type of stabilization program has helped with low back pain in professional cricket players, as well as to decrease the rate of lower extremity injury in Australian professional football players. (1,2) (see my post on The Local Stabilizing Muscles and Lower Extremity Injury.
You may be saying to yourself that you can save a lot of money and just palpate the transverse abdominis (TA), and the multifidus. However I would ask you… are you really feeling a transverse abdominis contraction, or some of the internal obliques? I have had 2 patients referred to me from very capable therapists that I respect and look up to. They were referred to me due to a lack of progress in their treatment. The therapist was addressing a local stabilization program, but their back pain was not getting better. To their credit, the therapist was able to train both patients to perform a proper TA contraction in supine, however one patient was unable to hold a contraction beyond 1 second, and another one was not able to activate it in sitting, or standing. This would explain why they were not progressing with respect to their pain. After treating each patient for 1 or 2 visits using US imaging, and sending them back to their referring therapist, they made rapid progress. Both therapists were so convinced on the usefulness of US imaging that they both went out and bought a machine to use in their clinic. Additionally, you would be surprised how many physical therapists (I can’t count the number on two hands anymore) I have seen that think they are properly performing a TA contraction and want to see how they are doing on the US. However, once we used the US imaging to assess their TA contraction, they realized they were overcompensating with their internal obliques. This is with physical therapists who have more knowledge than the general public regarding the importance of these muscles and how to activate them!
If you are knowledgeable in using ultrasound imaging, you open your doors to a number of possible patients you may not be currently accessing as referrals. There are numerous women and men who would like to receive treatment for pelvic floor weakness issues, but do not want to have to disrobe each treatment. Using ultrasound imaging is a wonderful option for these patients. It also is a way to treat younger patients that you have not been able to treat in the past as well (I would recommend taking the Pediatric Incontinence and Pelvic Floor Dysfunction course prior to treating pediatric patients). By using ultrasound imaging you not only gain an edge over your competing clinics that specialize in pelvic floor therapy, but you can gain an edge for back patients and sacroiliac joint patients as well. For the reasons I stated above when discussing a stabilization program centered on the use of US imaging, you could become very busy with referrals from spine surgeons, and ortho docs. In my office we have six therapists trained in using ultrasound imaging and two ultrasound machines. One of our most limiting factors is not the lack of patients to use ultrasound on, but that we only have two US units available to use! We have several spine physicians that send all of their patients to us because they have seen the difference using ultrasound imaging and the stabilization program can make in patients’ lives. We are eagerly awaiting a third machine and know it will be immediately used and allow us to further grow our clinic.
Now you may be saying, “Yes this would be handy but the pricing makes it impossible!” I would say think outside of the box! Some machines are going down in price making them more affordable. Plus, the settings we as therapists use are pretty basic, so we do not need to purchase a unit with a lot of bells and whistles that makes it more expensive. However there are other ways to acquire a unit other than purchasing one brand new. You could look into the price of refurbished units or look to your referring physician groups that you have a good relationship with. You may be surprised to find out how much physician’s offices get for machines when they are upgrading; hardly anything! If you work for a hospital system you may be able get the old machine transferred to your department for no cost to you! Or if you work in a private practice, you could offer to match the little amount the office would get from the vendor when upgrading. I guarantee you it would not be as much as a new unit. You also might be able to share a unit with another department, office, or clinic. In the past, I have shared ultrasound units with a surgical department, and a gynecology office. I would use the ultrasound some days of the week, and they would other days of the week. It worked out well! There are a lot of possibilities of ways to acquire an ultrasound unit if you think outside of the box! It may take a little effort coordinating things in order to get an US unit, but with proper knowledge, proper marketing, and word of mouth your business will grow and you will not regret the decision to invest in your practice!
Join me to discuss more ideas of how to use US imaging to grow your practice in both clinical skill as well as business growth this June in Baltimore!
1. Hides, Stanton, Wilson et al. Retraining motor control of abdominal muscles among elite cricketers with low back pain. Scand J Med Sci Sports. 2010; 20: 834-842.
2. Hides JA, Stanton WR. Can motor control training lower the risk of injury for professional football players? Med Sci Sports Exec. 2014; 46(4): 762-8.
The following post was contributed by Herman & Wallace faculty member Ramona Horton. Ramona teaches three courses for the Institute; "Myofascial Release for Pelvic Dysfunction", "Mobilization of Visceral Fascia for the Treatment of Pelvic Dysfunction - Level 1: The Urologic System", and "Mobilization of Visceral Fascia for the Treatment of Pelvic Dysfunction - Level 2: The Reproductive System". Join her at Visceral Mobilization of the Urologic System - Madison, WI on June 5-7!
My physical therapy training and initial experience were in the US Army, so I had a strong bias toward utilization of manual therapy techniques based on a structural evaluation. When the birth of my 10 pound baby boy threw me head-long into the desire to become a pelvic dysfunction practitioner, I became plagued by the question: how do you treat the bowel and bladder, without treating the bowel and bladder? That, along with a mild obsession for the study of anatomy was the genesis of my desire to explore the technique of visceral mobilization.
The field of pelvic physical therapy has moved far beyond the rehabilitation of the pelvic floor muscles for the purpose of gaining continence, which was its origin. Now pelvic rehabilitation is a comprehensive specialty within the PT profession, treating a variety of populations and conditions (Haslam & Laycock 2015). Research has provided a greater understanding of the abdomino-pelvic canister as a functional and anatomical construct based on the somatic structures of the abdominal cavity and pelvic basin that work synergistically to support the midline of the body. The canister is bounded by the respiratory diaphragm and crura, along with the psoas muscle whose fascia intimately blends with the pelvic floor and the obturator internus and lastly the transversus abdominis muscle (Lee et al. 2008). The walls of this canister are occupied by and intimately connected to the visceral structures found within. These midline contents carry a significant mass within the body. In order for the canister to move, the viscera must be able to move as well, not only in relationship to one another, but with respect to their surrounding container. There are three primary mechanisms by which disruption of these sliding surfaces could contribute to pain and dysfunction: visceral referred pain, central sensitization and changes in local tissue dynamics.
Since the inception of physical therapy, manual manipulation of tissues has been a foundational practice within the profession. Manual therapy is a generic therapeutic category for hands-on treatment of a structural anomaly; it encompasses a variety of techniques which can be subdivided into either soft tissue based or joint based. Although the majority of manual therapy research has been on the musculoskeletal system, its effects are not exclusive to any particular region of the anatomy. The Orthopaedic Section of the American Physical Therapy Association (APTA) defines the technique of mobilization as "the act of imparting movement, actively or passively, to a joint or soft tissue" (Farrell & Jensen 1992). Visceral mobilization is a treatment approach focusing on mobilizing the fascial layer of the visceral system with respect to the somatic frame; it therefore falls under the classification of soft tissue based manual therapies. Soft tissue and or fascial based manual therapies have higher-levels of evidence to support their use for treating musculoskeletal pain and dysfunction (Ajimsha & Al-Mudahka 2014; Gay et al. 2013). Although many models have been proposed, the specific mechanisms behind the response of the musculoskeletal system to manual interventions are still not fully understood (Bialosky et al. 2009; Clark & Thomas 2012).
The previous model of manual therapy directly relieving local tissue provocation has given way to a recognition that the observed clinical improvement is not simply a result of the practitioner directly altering the structure beneath their hands through mechanical means. Rather this improvement is a combination of afferent input influencing the neurophysiologic output, changes in the endogenous cannabinoid system, and even a placebo responses simply because of touch (Bialosky et al. 2009; McParland 2008; Gay et al. 2014).
There is significant clinical evidence that issues of somatic pelvic pain, bowel, bladder and reproductive system dysfunction may be the result of visceral referred pain, central sensitization and restrictions in visceral tissue mobility which may further contribute to dysfunction within the canister of core muscles. The musculoskeletal framework is a mysterious, perplexing and complicated system. It is unique in that it offers us a variety of tissues and techniques from which to choose in order to help our patients from a manual therapy perspective. Science has acknowledged that the visceral structures and their connective tissue attachments indeed have an influence on the function of the somatic frame, the question is can we manually manipulate these structures and bring about an effect with a reasonable degree of specificity while producing a therapeutic outcome.
Part 2 of this report will discuss the evidence to support visceral mobilization.
Ajimsha M.S., Al-Mudahka N.R. & Al-Madzhar J.A. (2015) Effectiveness of myofascial release: Systematic review of randomized controlled trials. Journal of Bodywork and Movement Therapies 19, 102-112.
Clark B.C., Thomas, J.S., Walkowski S., Howell J.N. (2012) The biology of manual therapies. The Journal of the American Osteopathic Association 112 (9), 617-29.
Bialosky J., Bishop M. & Price D. (2009) The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Manual Therapy 14 (5), 531-538.
Gay C.W., Robinson M.E., George S.Z., Perlstein W.M. & Bishop M.D. (2014) Immediate changes after manual therapy in resting-state functional connectivity as measured by functional magnetic resonance imaging in participants with induced low back pain. Journal of Manipulative and Physiologic Therapeutics 37 (6), 614-627.
Haslam J. & Laycock J. (2015) How did we get here? The development of women’s health physiotherapy special interest groups in the UK. Journal of Pelvic Obstetric and Gynecological Physiotherapy 116 (Spring), 15-24.
Farrell J.P. & Jensen G.M. (1992) Manual therapy: a critical assessment of role in the profession of physical therapy. Physical Therapy 72, 843-852.
Lee D.G., Lee L.J. & McLaughlin L. (2008) Stability, continence and breathing: The role of fascia following pregnancy and delivery. Journal of Bodywork and Movement Therapies 12 (4), 333-348.
McPartland J M (2008) Expression of the endocannabinoid system in fibroblasts and myofascial tissues. Journal of Bodywork and Movement Therapies 12(2), 169-182.
A few weeks ago, a pelvic course participant shared some sensitive and intimate thoughts about being at a course and being "the biggest girl in class." This week, we will address specific strategies for communicating with your patients and for adapting your exam techniques when appropriate. The following quote is from an educational book for Nurse Practitioners, and echoes a very healthy and realistic sentiment about our role when working with patients in pelvic rehabilitation.
"If the exam is limited by obesity, the patient should be told in a clear, non-judgmental manner. Patients have a right and responsibility to understand the findings of the health care visit."

Unfortunately, according to the authors, women who are obese are less likely to receive routine gynecologic care due to bias and fear of judgement, or even practical issues like exam tables, gowns, and equipment not being adequate. Another issue is that of mobility: is the exam table too narrow for safety and comfortable positioning? In my own clinical practice, I have had patients ask me: "Is that massage table going to hold me?" In order to answer that question, you need to know what the safe weight limits are for your chairs, walkers, exam tables, and any other equipment your patients may use. You might imagine that if a patient is concerned about falling off of a table, completing an appropriate exam could be difficult due to muscle guarding. Other techniques recommended include the following:
- ask an assistant to gently hold back skin folds if vagina or vulva is obscured
- ask the patient to flex her hips upward if able
- ask patient to help hold back excess skin in lower abdomen if helpful
- ultrasound may be used rather than palpation as needed (this is in reference to a medical gynecologic exam, but how might rehab US contribute to our toolkit?)
- document any difficulty with the examination - placing a small towel or pillow under the patient's hips may also help in viewing the cervix
This "Bias Tool Kit" offers further suggestions to avoid causing harm when evaluating a woman who is obese:
- if you would like to weigh the patient, ask for consent first, using sensitive language, i.e. "would you like to be weighed today?" and maintain privacy
- in addition to considering equipment like tables, think about having a stepstool with a handle, properly sized blood pressure cuffs, sturdy, armless chairs, and a long exam speculum
- use words that patients find more acceptable, such as excess weight or BMI
Advice to the nurse practitioners include the following to counter the fact that obese women are often discriminated against:
"If the exam is limited by obesity, the patient should be told in a clear, non-judgmental manner. Patients have a right and responsibility to understand the findings of the health care visit." For example, for a medical exam: "Due to the shape and size of your body, I wasn't able to feel your uterus and ovaries." Any similarly needed communications can be shared in a professional and warm tone.
While sensitive topics can require patience, practice, and an abundance of professionalism, everyone wins when difficult subjects are approached with honesty. Thanks again to Erin B. for shining her light on this sensitive and valuable topic.

Earlier this week a blog post asked the question "Do male therapists belong in pelvic rehab?" With increased frequency, male therapists are participating in pelvic rehab coursework and practices. Some of the male therapists are even attending coursework as students. I asked Justin Stambaugh, a student from Duke University (who very much impressed me with his command of the material, and his calm, curious, and competent demeanor), a few questions about his path into pelvic rehab. Below are his responses.
Holly: How did your path lead towards pelvic rehab in general?
Justin: Pelvic rehab really necessitates an openness and sense of comfort regarding issues that can be seen as very personal, private, and even taboo. I was drawn to pelvic rehab because I am the type of person who doesn’t believe that individuals should have to suffer in silence because of fear or embarrassment of addressing their issues. I want people to know that they can and should seek treatment for their pelvic health issues, and that physical therapy can be a valuable resource in this regard.
I also value the complexity of pelvic rehab. In addition to the clinical aspect of care there is also the psychosocial element that adds to the scope and depth of treatment. I appreciate that pelvic rehab requires the clinician to continuously evaluate and adapt their approach in order to be proficient.
Additionally I find that often times many physicians, patients, and other physical therapists don’t realize the extent of what we are capable of treating, and how great of an impact we can have on someone’s life. I get excited about educating and promoting this side of the profession.
Holly: What is your viewpoint on how you will be perceived as a male therapist in treating pelvic rehab with a female patient?
Justin: As a male therapist in the pelvic rehab setting I understand that there are some female patients who will be hesitant to work with me solely because of my gender. I think this is an unfortunate fact, however it simply requires me to be a bit more industrious as a practitioner. Patients who may initially be uncomfortable with me due to my gender are really just asking me to prove to them that I know what I’m doing and that I am trustworthy. It is completely understandable that I need to win their trust before moving forward with any type of treatment. I respect my patients and ultimately just want what’s best for them. We can work together on achieving this goal, and find the correct path that suits each patient’s needs based on their comfort level. Often times I think of the phrase “to a man with a hammer, everything looks like a nail”. Although I am capable of performing an internal pelvic floor exam and subsequent treatment, there are also external approaches that may work just as well for an apprehensive patient depending on their presentation. This may also help gain their trust in order to implement more effective care in future sessions.
Holly: How do you think your generation differs from those before you in addressing the entire issue of gender?
Justin: I would like to think that my generation is more open regarding issues of sex and gender. However I think there are still many hurdles left to climb in this regard. I feel that socially my generation is part of an evolution in tolerance and empathy towards diversity with respect to issues such as gender, gender identity, sexual orientation etc. All of these qualities define some part of all of us and are constantly being communicated and evaluated. If we look back through history we see the dynamics of social inequality based on gender. Today we continue to see broad discussions regarding sex and gender. I feel that each generation continues to grow from these conversations and socially we persist in advancing our understanding and comfort regarding this topic.
Holly: Where do you see us (on the continuum) as a profession in normalizing the experience of having treatment directed to the pelvis by any gendered therapist to any gendered patient?
Justin: It would be my hope that in the future more institutions will instruct pelvic health with patient models that allow students to interact and conduct treatment based therapies in a clinical manner. I feel that in order to alleviate some of the gender based fears and apprehension regarding pelvic rehab from a professional perspective, all students should get to experience this aspect of physical therapy before deciding if its for them. I do feel it’s unfortunate that there are not more males who are interested in pelvic rehab. Oftentimes people are afraid of what they don’t know. It seems that perhaps pelvic rehab has remained somewhat enigmatic in that many individuals don’t get to experience this type of patient care, and therefore never approach it. It is such a great benefit to be able to work with this population of patients. I feel that the more exposure and normalization pelvic rehab gets to the patient population as well as to the professionals in the field of physical therapy the more we will see an increase in gender representation within the profession.
If the work of pelvic rehab is in the hands of students like Justin, we have so much to look forward to in our field. Thank you to Justin for being willing to articulate his thoughts and experience so that we can continue to explore issues of gender in pelvic rehabilitation.
Today's post on the Pelvic Rehab Report comes from faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC. Allison instructs the ultrasound imaging courses, the next of which will be Rehabilitative Ultra Sound Imaging: Women's Health and Orthopedic Topics in Baltimore, MD on Jun 12, 2015 - Jun 14, 2015.

In the past several decades there has been quite a bit of research regarding stabilization of the low back and pelvic ring. We as therapists have changed our focus from working more of the global stabilization muscles to the local stabilizing muscles; the transverse abdominis, the lumbar multifidus, and the pelvic floor. Both research studies and clinical experience has shown us what a positive difference working on these muscles can makes for back pain and pelvic ring pain, as well as for the risk of injury in the back and pelvic ring. However, what does it do for risk of injury for the lower limb? In 2014, Hides and Stanton published a study looking at the effects of motor control training on lower extremity injury in Australian professional football players. A pre- and post-intervention trial was used during the playing season of the Australian football league as a panel design. Assessment included magnetic resonance imaging and measurements of the cross-sectional area of the multifidus, psoas, and quadratus lumborum, as well as the change in trunk cross-sectional area due to voluntary contraction of the transverse abdominis muscle. A motor control program included training of the multifidus, transversus abdominis, and the pelvic floor muscles using ultrasound imaging for feedback that then progressed into a functional rehabilitation program was used with some of the players. Injury data was collected throughout the study. Results showed that a smaller multifidus or quadratus lumborum was predictive of lower limb injury during the playing season. Additionally, the risk of sustaining a severe injury was lower for players who received the motor control intervention.
This is interesting and intriguing information. Yes, there are many factors that are involved in sustaining an injury during a sport. However, it would be a good idea to do a quick screen of the local stabilizing muscles before a playing season, whether it is a professional player or an adolescent player. Do adolescents really have issues with weakness in their local stabilizing muscles? Yes! Clinically I have seen adolescent players who display back pain and other issues related to weakness in their core muscles. Usually this occurs after they have gone through a growth spurt, but some of these adolescent athletes did not recover, even several years after the large growth spurt.
What a nice community service it would be to screen a local sports team for strength of the local stabilizing muscles in order to decrease injuries! It would also be nice to see additional research regarding this topic! To learn more about recent research and how to use ultrasound imaging to accurately assess and treat the local stabilizing muscles, join me at Johns Hopkins in Baltimore this June for the Rehabilitative Ultrasound Imaging for the Pelvic Girdle and Pelvic Floor course.
Hides JA, Stanton WR. Can motor control training lower the risk of injury for professional football players? Med Sci Sports Exec. 2014; 46(4): 762-8.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./











































