The abdominal canister is a model that we have used in rehab for a number of years, especially when it comes to discussing the (often controversial) topic of core stability. Traditionally regarded as encompassing the pelvic floor, diaphragm, deep abdominal muscles (particularly Transversus Abdominus), our definitions of ‘the canister’ or ‘core’ have of late expanded to include psoas, obturator internus, quadratus lumborum and the osseous components of the pelvic girdle (Chaitow 2012).
 Often, we in pelvic rehab bemoan the fact that the pelvic floor is not given the attention it deserves (when we know it really is the answer to everything…) but I do believe that we, as pelvic health specialists are just as guilty of not paying enough attention to the ‘roof’ of the canister, the diaphragm.
Often, we in pelvic rehab bemoan the fact that the pelvic floor is not given the attention it deserves (when we know it really is the answer to everything…) but I do believe that we, as pelvic health specialists are just as guilty of not paying enough attention to the ‘roof’ of the canister, the diaphragm.
The diaphragm and the pelvic floor are bound together structurally and functionally by both fascial and muscular connections (Chaitow 2012). The anatomical link between the diaphragm, psoas and the pelvic floor has been explored by Gibbons in 2001 ‘…The diaphragm’s medial arcuate ligament is a tendinous arch in the fascia of psoas major. Distally, the psoas fascia is continuous with the pelvic floor fascia, especially the pubococcygeus’. Newell in 2005 discussed the relationship between the diaphragm and transversus abdominus and Carriere in 2006 concluded that psoas spasm may influence diaphragmatic mechanics, and conversely that abnormal tensions in the medial arcuate ligament of the diaphragm may irritate psoas.
Paul Hodges has also concluded in his 2007 paper that breathing and continence may be more connected to low back pain than levels of activity or BMI, reinforcing Smith’s 2006 study looking at the link between breathing disorders, pelvic floor dysfunction and back pain in over 38,000 Australian women.
Of course, breathing, like pelvic floor functioning, can also be linked to psychological factors: when we are stressed, our breathing tends to become more apical (and our pelvic floors may hold excess tension). When that becomes habitual rather than a temporary stress response, a sub-optimal breathing pattern may develop, which disrupts the abdominal muscle balance and makes both back and pelvic pain more likely, with the added risk of pelvic venous congestion (Chaitow 2012). Myofascial trigger points may also develop because of restricted breathing patterns. We also know the opposite is true – such as using controlled breathing to calm down, to let go of tension and even to modify pain and autonomic responses (Busch 2012). Athletes may be at a particular risk of dysfunction, competing at high levels of intensity, both physically (in competition?) and psychologically (fear of losing a college scholarship?) Although more research is needed to confirm or disprove these connections, theoretically normalizing breathing patterns may improve outcomes in cases of low back or pelvic pain.
In my specialist course ‘The Athlete & the Pelvic Floor’ in Denver next month, we will look at specific manual therapy interventions for the diaphragm and its allies, the psoas and quadratus lumborum. As with any manual therapy techniques, we must always follow up with a clinical and home exercise program, or the effects will be only temporarily beneficial (Coronado 2011, Hegedus 2012) and so we will look at breath re-patterning, integration with the pelvic floor and how this is an often overlooked step when it comes to managing athletes with pelvic floor dysfunction. Hope to see you there!
References:
1. Chaitow, L & Jones, R (Eds) ‘Chronic Pelvic Pain and Dysfunction 2012 Elsevier Churchill Livingstone
2. Gibbons, S.G.T. 2001 The model of Psoas Major stability function. In: Proceedings of 1st International Conference on Movement Dysfunction, Sept 21-23 Edinburgh, Scotland
3. Newell, R. 2005 Anatomy of the post-laryngeal airways, lungs and diaphragm. Surgery 23 (11) 393-397
4. Carriere, B 2006 Interdependence of Posture and the Pelvic Floor. In: Carriere, B The Pelvic Floor, Thieme New York
5. Hodges, P, Sapsford, R, Pengel, L 2007 Postural and respiratory functions of the PFMs. Neorourol. Urodyn. 26 (3), 362-371
6. Smith, M, Russell, A, Hodges, P., 2006 Disorders of breathing and continence have a stronger association with back pain than obesity and physical activity. Aust. J. Physiother. 21(52) 11-16
7. Coronado, R, Bialosky, J & Cook, C. 2010 The temporal effects of a single session of high-velocity, low-amplitude thrust manipulation on subjects with spinal pain Physical Therapy Reviews Volume 15, Issue 1 (01 February 2010), pp. 29-35
This week we get to feature Katie Tredo, DPT, PRPC, one of the first people to earn her Pelvic Rehabilitation Practitioner Certification! Katie co-owned a private practice in Maryland, and has recently relocated to the Milwaukee area to practice her trade. She was kind of enough to offer her insights with the Pelvic Rehab Report today.
![]() Hi Katie! Tell us a little bit about your clinical practice
Hi Katie! Tell us a little bit about your clinical practice
I recently joined the staff at Health In Balance Physical Therapy in Mequon, WI. Our team is made up of experienced physical therapists with a variety of interests and specialties. Along with two of my coworkers, my practice is focused on treating men, women, and children with pelvic dysfunctions. I think a practice with such a skilled and diverse set of physical therapists allows us to better serve our patients.
What patient population do you find most rewarding in treating and why?
I find treating patients with pelvic dysfunctions, especially pelvic pain, to be extremely rewarding. Pain, incontinence, and other pelvic dysfunctions can leave patients feeling very isolated and hopeless. Watching my patients open up about their issues then progress toward their goals, returning to their previous activities and relationships without pain or dysfunction is amazing. There are so many quality of life issues that go along with pelvic dysfunctions and I am honored to be a part of each of my patient’s journey to recovery.
If you could get a message out to physical therapists about pelvic rehabilitation what would it be?
I would encourage physical therapists to get comfortable asking about bowel, bladder, and sexual dysfunction on their initial intake forms. Many people will not think to report these issues without being asked and a pelvic dysfunction can be a major component of a hip or back issue. If your patient reports a pelvic dysfunction, be comfortable acknowledging it and make an appropriate referral for them. I enjoy working closely with and sharing patients with other physical therapists so that we can maximize our patients’ recovery.
What role do you see pelvic health playing in general well being?
In the past discussing pelvic dysfunctions was considered embarrassing or taboo. In the past few years, I have seen more and more of my patients educating themselves, discussing their issues with other men or women, and finding themselves the help they need. Many patients are going into their referring physicians and requesting to receive help instead of waiting for their doctor’s suggestion. Patients are becoming more empowered over their own care. I see pelvic health becoming more and more of a focus in people’s lives and that fewer patients will be content living with their dysfunction.
Within 1 week, I examined 2 women with the diagnosis of lumbar pain who each happened to mention having a hip labral tear. Of course, neither woman volunteered information about the pelvic floor dysfunction she has lived with since having children. When I took the extra step and openly asked if they had any “issues” in the pelvic floor region, both women initially looked surprised and then relieved as they shared (perhaps for the first time) the problems they’ve had. I started to wonder about the contribution of pelvic floor dysfunction to acetabular labral tears, or vice versa, and I knew each problem had to be addressed for the referring diagnoses to be treated completely and effectively.
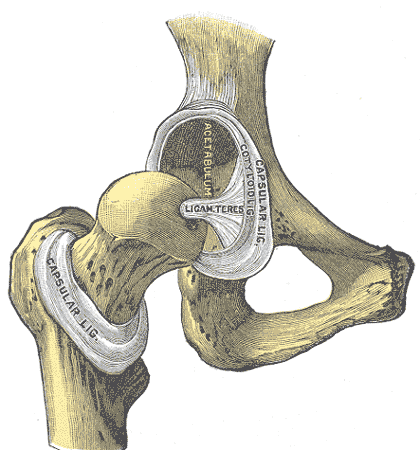
Considering the anatomy of the acetabular labrum in relation to the pelvic floor structures, there is undeniably a connection. A thorough review of pelvic anatomy is given in the Functional Applications in Pelvic Rehabilitation course by Kathe Wallace. Just briefly, the acetabulum is the depression in the pelvis (os coxae) where the femoral head articulates. The labrum sits in the acetabulum, which faces anteriorly along with the femoral head, requiring the anterior aspect of the labrum to stabilize this portion of the hip that lacks bony contact. The obturator internus muscle, which is a deep hip external rotator and abductor, attaches to the posterior aspect of the obturator foramen and inserts on the medial surface of the greater trochanter. When this muscle is in spasm or inhibited, the pelvic floor and the hip can suffer.
 In 2009, Groh and Herrera published a review of hip labral tears, and the general consensus was that labral tears “occur more frequently in women than in men.” The fact that women have more hip dysplasia than men has been suggested as a cause for this finding; however, many of the women with labral tears do not have concomitant hip dysplasia. Alas, Hunt et al (2007) pointed out that women have a generally higher incidence of pelvic-floor pain, which could contribute to the higher incidence of labral tears.
In 2009, Groh and Herrera published a review of hip labral tears, and the general consensus was that labral tears “occur more frequently in women than in men.” The fact that women have more hip dysplasia than men has been suggested as a cause for this finding; however, many of the women with labral tears do not have concomitant hip dysplasia. Alas, Hunt et al (2007) pointed out that women have a generally higher incidence of pelvic-floor pain, which could contribute to the higher incidence of labral tears.
Interestingly, in a study by Brooks and Domb (2012), 10 women over 2 years presented post-partum with anterior hip pain and required labral surgery. The excessive hip external rotation needed for natural delivery was implicated in the pathology, and the authors encouraged obstetricians to have women evaluated prior to delivery and mobilized properly so they could prevent the tears. Hormonal changes in the ligaments as well as the posture assumed by pregnant women with increased lordosis placing more shearing on the anterior aspect of the hip are also factors to consider. Not to mention, the pelvic floor connection to the acetabular labrum certainly seems a reasonable culprit for making the labrum more susceptible to injury during pregnancy and/or delivery.
With the improved technology to diagnose acetabular labral tears, more are being found and treated surgically. The higher incidence of labral pathology in women makes the contribution of pelvic floor dysfunction a serious possibility to consider. If the labrum gets fixed but the pelvic floor is still an issue, becoming completely asymptomatic is less likely. Seeing 2 patients in 1 week who each presented with low back pain, labral tear, and pelvic floor dysfunction when I only work part time makes me think we cannot deny the importance of our subjective examination in uncovering all the possible causes of any suspected tissue in lesion.
Herman & Wallace faculty member Ginger Garner teaches an excellent course called "Extra-Articular Pelvic and Hip Labrum Injury: Differential Diagnosis and Integrative Management" which explores acetabular labral tears in depth. Join Ginger next May in Rochester, NY to learn some great evaluation and treatment techniques!
References:
Groh, M. M., & Herrera, J. (2009). A comprehensive review of hip labral tears.Current Reviews in Musculoskeletal Medicine, 2(2), 105–117. doi:10.1007/s12178-009-9052-9.
Hunt D, Clohisy J, Prather H. (2007). Acetabular tears of the hip in women. Phys Med Rehabil Clin N Am.,18(3):497–520.
Brooks AG, Domb BG. (2012). Acetabular labral tear and postpartum hip pain. Obstet Gynecol. 120(5):1093-8.
Cognition in later years may be affected by premature menopause, according to an article published online in the British Journal of Obstetrics and Gynaecology. In the study 4,868 women at least 65 years old were assessed on a cognitive test battery and were evaluated for clinical dementia. Associations between the subject’s age at menopause, surgical versus natural menopause, use of menopausal hormone therapy, and cognitive function later in life were studied. According to introductory concepts described in the article, estrogen level changes postmenopause are associated with brain atrophy and memory complaints.
Tests were administered at baseline, and again at 2, 4 and 7 years from baseline. Tools included the Mini-Mental State Examination (MMSE) for global cognitive function, Benton’s Visual Retention Test (BVRT) for visual memory assessment, Isaacs Set Test for verbal fluency or semantic access, and the Trail Making Tests A and B for timed visual motor tasks of psychomotor speed and attention and executive function. Unrelated to cognitive function, The Rosow and Breslau mobility and Instrumental Activities of Daily Living scales, the Centre for Epidemiology Studies Depression Scale (CES-D), and other instruments were used to assess socioeconomic, demographic, lifestyle and health information. Dementia was also evaluated by a trained psychologist (or neurologist if subject was suspected to have dementia) and cases were assessed by a panel of dementia experts as a third step in the process.
Natural menopause was noted in 79% of the subjects, surgical menopause in 10%, and 11% due to other causes including radiation, chemotherapy, or unknown. Less than 1 in 7 women was currently using hormone therapy, and over 1/5 used hormone therapy at menopause (most commonly reported treatment was transdermal estradiol- median time of use was 10 years).
The authors concluded that variables such as verbal fluency, visual memory, psychomotor speed and global cognitive function can be negatively impacted by premature menopause. Specifically, premature menopause including premature ovarian failure or surgical menopause at 40 years of age or less was independently associated with increased risk of poor verbal fluency and visual memory later in life. Premature menopause was also associated with increased risk of psychomotor speed and global cognitive decline. The primary conclusion of the article is that when an ovariectomy is being considering in younger women, the potential negative impact on cognitive function should make up part of the risk/benefit discussion. Hormonal influence during various stages of a woman’s life can have a dramatic impact on many variables impacting quality of life and rehabilitation efforts. To learn more about menopause, the Institute offers several courses that contain information about rehabilitation for women throughout the lifespan.
Herman & Wallace offers an excellent course called "Menopause Rehabilitation and Symptom Management ", where you can learn about evaluating and treating menopause patients. Forward thinking therapists can provide an integrative, safe and effective/evidence based approach, such as menopausal weight loss, cardiovascular health promotion and mind body awareness, and Menopause: A Rehabilitation Approach - Atlanta, GA on March 19-20, 2016 is a great opportunity to learn such skills.
You’ve done a thorough evaluation of the lumbar spine. You’ve done all the special tests for hip pathology, but something is missing. Of course it could be a pelvic floor issue, but what else? Think about the middle child who gets ignored even if making a commotion or goes unnoticed unless being tripped over when standing still. Perhaps the missing link to your patient’s dysfunction is the sacroiliac joint, that “in between” area. If you are unsure how to assess and deal with the “middle child,” learning more about Sacroiliac Joint and Evaluation is something to add to your professional bucket list.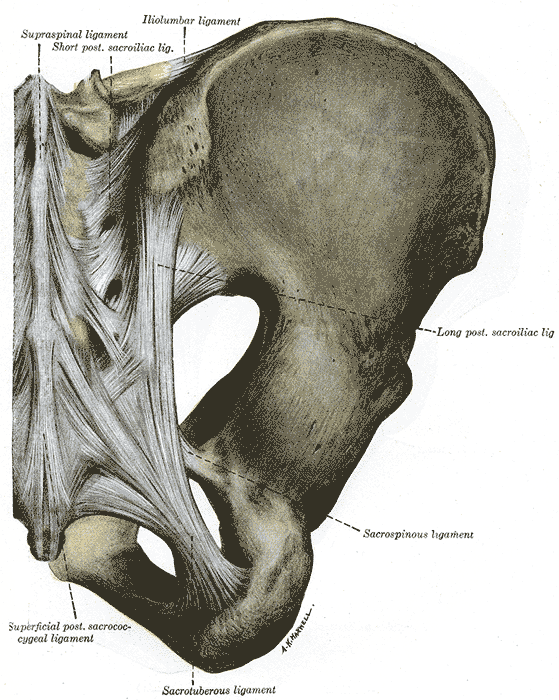
According to the special tests book by Chad Cook, a pain mapping test suggests a referral pattern of SI dysfunction as pain in the buttock unilaterally, below the level of L5, without symptoms in the midline. Often we are on a mission to make the lumbar spine the source of symptoms, but this provides some guideline as to where the pain would be located if the SI joint were the guilty party. If pain is found above L5, the SI joint is likely not the primary tissue in lesion. If the pain is bilateral, the issue is more than just SI joint.(Cook, 2013)
The special tests to diagnose SI joint dysfunction have been considered in a cluster. According to Laslett, distraction, compression, thigh thrust, Gaenslens, and Patricks are the primary tests used to assess SI dysfunction. Three or more of these tests being positive can help a clinician rule in SI joint as a diagnosis, with SI joint blocks being just as predictive. When pain cannot be centralized, and three of the tests are positive, there is a 77% probability the SI joint is the source of pain; and, in the pregnant population, there is an 89% chance the SI joint is the culprit of pain.(Laslett, 2008)
While parents keep up with the oldest and youngest, the middle child can be hard at work causing dysfunction that disrupts the whole family. Likewise, the sacroiliac joint can be hypermobile, hypomobile or have ligamentous strain, yet we therapists may ignore any signs until the lumbar spine or hip or pelvic floor are suddenly provocative. The longer an SI joint dysfunction goes undiagnosed and untreated, the greater the likelihood of pelvic floor dysfunction, secondary to its intimate relationship to the area. A catawampus ilium position on the sacrum can cause hip pain, and the ilium’s relationship to the sacrum can aggravate the lumbar spine. We just need to use all our diagnostic tools to discern what is making our patients symptomatic and then prioritize the treatment.
Taking the upcoming sacroiliac course through Herman Wallace (Sep. 12-13 in New Orleans) will make the “middle child” become respected, understood, and never left wanting again. Review the anatomy, explore and proficiently perform the special tests, and effectively implement treatment and stabilization of the SI joint during this course. You owe your patients the ability to understand the lumbar region and pelvic ring in their entirety and leave no source of pain a mystery.
References:
Cook, C., & Hegedus, E. (2013). Orthopedic physical examination tests: An evidence-based approach. Upper Saddle River, N.J.: PearsonPrentice Hall.
Laslett, M. (2008). Evidence-Based Diagnosis and Treatment of the Painful Sacroiliac Joint. The Journal of Manual & Manipulative Therapy, 16(3), 142–152.
A recent systematic review published in The Lancet online describes the benefits of using music as a postoperative aid in recovery. Seventy-three randomized, controlled trials were included in the review, and the articles covered the use of music before, during, and after surgery. A wide variety of surgical procedures were represented in the research articles, and included cardiac procedures, mastectomy, urogynecologic and abdominal surgeries, and gastrointestinal surgeries and procedures. Interventions included listening to music with headphones, listening to relaxation training or “therapeutic suggestion.” Many of the studies included a control group with routine care or white noise, headphones without music.
The main results of the research is that use of music reduces postoperative pain, anxiety, and analgesia use, and improves patient satisfaction. The timing of or choice of music listened to in the studies did not significantly affect outcomes. Interestingly, even when patients were given general anesthesia, music was effective. And when patients chose their own music, there was a slight increase in reduction of pain and analgesia use.
How can this information be of use to pelvic rehabilitation providers? Perhaps one of your patients will be heading into surgery. A recommendation for listening to favorite music in the postoperative period could be made. Is music available to your patients in your setting? If so, what kind of music? Is the patient allowed to influence the type of music? Maybe the patient could play a favorite song list from their smart phone, or request a certain time period of music on a music subscription service you may use in the clinic. Regardless of how we use this information, it’s great to be reminded of the potentially positive ways that music can influence healing.
National Public Radio (NPR) recently posted a story on their website that you can listen to if you are interested. For more interesting reads about music and healing, check out the links below:
Psychology Today: Does Music Have Healing Powers?
Scientific American: Music Can Heal the Brain
 We know that many of our patients who struggle with severe pelvic pain need rehabilitation efforts directed towards quieting of the nervous system. In general, activation of the parasympathetic system is a goal, with targeted physiologic improvements in heart rate, respiration, and blood pressure, for example. Many providers are teaching patients physiologic quieting techniques such as breathing, mindfulness strategies, visualization, meditation, and encouraging activities like yoga. Does yoga really affect the nervous system? To assess the ability of yoga to increase cardiac parasympathetic nervous system modulation, a study published in Evidence-Based Complementary and Alternative Medicine examined the effects of yoga practice on physiologic variables.
We know that many of our patients who struggle with severe pelvic pain need rehabilitation efforts directed towards quieting of the nervous system. In general, activation of the parasympathetic system is a goal, with targeted physiologic improvements in heart rate, respiration, and blood pressure, for example. Many providers are teaching patients physiologic quieting techniques such as breathing, mindfulness strategies, visualization, meditation, and encouraging activities like yoga. Does yoga really affect the nervous system? To assess the ability of yoga to increase cardiac parasympathetic nervous system modulation, a study published in Evidence-Based Complementary and Alternative Medicine examined the effects of yoga practice on physiologic variables.
Cardiac vagal modulation was the primary variable assessed in this study; ambulatory 24-hour Holter monitoring, with heart rate variability (HRV) identified hourly by a blinded observer, was the method used to collect data. (The authors explain that this is an established tool to measure HRV, and that HRV can be used as a predictor of cardiac mortality and sudden cardiac death.) Eleven healthy yoga practitioners (4 men and 7 women) completed 5 sessions of training. All of the subjects had at least 3 years of experience practicing Iyengar yoga, and some of the subjects were certified Iyengar instructors. During 2 of the sessions, subjects were trained for 90 minutes, once per week, for 5 weeks. During 2 of these sessions, the subjects practiced a yoga session developed by B.K.S. Iyengar for cardiac patients, and during the other 3 sessions, they practiced a placebo relaxation session. The yoga program started with 15 minutes of resting poses, 60 minutes of standing poses, backbends, inverted poses, and ended with 15 minutes of resting poses. (The yoga sequence is listed in the linked article.) The yoga practitioners were matched to a healthy group of volunteers not practicing any relaxation techniques and instead participating in a placebo program. The placebo program included 15 minutes of resting on the floor, 60 minutes walking in a park, followed by another 15 minutes resting on the floor.
Results of the monitoring indicated that heart rate variability was significantly higher during the yoga intervention. The authors conclude that “…relaxation by yoga training is associated with a significant increase of cardiac vagal modulation.” Recommended as an easy-to-apply, no side effects intervention for cardiac rehabilitation programs, it seems that yoga could be beneficial for many patients with different conditions and in various practice settings. The yoga applications can be modified with props and by sequence of yoga postures to account for patient’s level of health. Finding yoga instructors who are capable of adapting yoga to a patient’s specific needs is also important, and if you would like to learn more about yoga applications in rehabilitation, the Institute has several courses that you may find helpful.
Herman & Wallace has several courses available for practitioners who want to start implementing these tools into their practice. Yoga for Pelvic Pain discusses the positive effects of yoga on interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia, and it includes the instruction of many poses/techniques. The next opportunity to take this course is next month, September 12-13 in Boston, MA.
Infertility is often times a very sensitive subject for couples who are struggling to conceive. In the US, there are approximately 6.7 million women who are facing challenges with getting pregnant. (CDC 2006). In 2015, a ten-year retrospective study examined the efficacy of manual physical therapy to treat female infertility and discovered significantly positive outcomes.
The study looked at data collected from 2002-2011, which included approximately 1,392 patients treated for infertility. It specifically included those with single or multiple causes for infertility that involved: 1) elevated FSH (follicle stimulating hormone) of 10 mIU/ml or higher 2) fallopian tube occlusion 3) Endometriosis- when the lining of the uterus grows outside of the uterus causing significant pain, abnormal bleeding, infertility 4) Polycystic Ovarian Syndrome (PCOS)- a condition that affects female hormone regulation at times producing multiple follicles that remain as cysts in and around the ovary 5) Premature Ovarian Failure (POF)-loss of ovarian function before a woman is 40 years old and 6) Unexplained Infertility (Rice, 2015)
Patients were treated using an individualized physical therapy treatment plan that was named the CPA (Clear Passage Approach) protocol. This protocol was tailored to meet the individual needs of the patients and to treat specific sites of restrictions and immobility within each patient’s body. Treatment included integrated manual therapy techniques focused on minimizing adhesions and decreasing mechanical blockages in order to improve mobility of soft tissue structures. Visceral manipulation was also used to help restore normal physiologic motion of organs with decreased motility.
The application of these specific manual therapy modalities are thought to activate the central nervous system by stimulating a local tissue response and thus increasing communication with higher control centers in the brain that have the ability to positively influence the activity of the ovary and uterus, as a result effecting hormone production and regulation.
The study compared manual physical therapy treatment to previously published success rates with standard, conventional treatments for female infertility. The results were astounding. Researchers discovered that with the application of the CPA manual therapy approach, fallopian tube patency of at least one fallopian tube was 60.8% successful. When compared with the reported success rates in the literature, “it was observed that the CPA performed as well as or at higher rates of success than surgery did.” The rate of pregnancy for those patients with at least 1 open fallopian tube was also very successful with an overall pregnancy rate of 56.64% post CPA treatment.
For those women with endometriosis (n=558), the success rates for pregnancy post CPA treatment was 42.8%. For those who underwent IVF (In Vitro Fertilization) after CPA treatment, the pregnancy rates were even higher at 55.4%. These findings were also comparable to or better than standard medical interventions published in current literature.
Manual therapy has even shown to decrease elevated FSH levels and improve pregnancy rates by almost 50%. Researchers acknowledge that, to date, there are no medical treatments that represent standard care for women with elevated FSH levels and require more investigation for comparative results.
Of the 59 women with PCOS, the overall pregnancy success rate was 53.57%. The only significant and direct comparison with standard of care literature was with the use of metformin. Comparably, CPA produced significantly higher rates of pregnancy than with metformin alone. No statistically significant outcomes were reported. Unexplained infertility and POF had the least success rates of pregnancy reported. This is most likely attributable to a lack in subject size and/or no published medical treatment in these specific patient cases, further warranting the need for future investigation.
In conclusion, manual physical therapy has been shown to reverse female infertility in cases such as occluded fallopian tubes, endometriosis, hormone dysregulation, and PCOS. With all of the conventional options available, it is wonderful to know that manual therapists specializing in pelvic health have a clinical significance in helping change the lives of women struggling with infertility.
Center for Disease Control and Prevention (2006-2010). Infertility. Retrieved from http://www.cdc.gov/nchs/fastats/infertility.htm
Rice AD, Patterson K, Wakefield LB, Reed ED, Breder KP, Wurn BF, King CR, Wurn LJ. Ten-year Retrospective Study on the Efficacy of a Manual Physical Therapy to Treat Female Infertility. Alternative Therapies. 2015.(21)3;32-40.
Carolyn McManus, PT, MS, MA is the author and instructor of "Mindfulness Based Pain Treatment: A Biopsychosocial Approach to the Treatment of Chronic Pain". Carolyn is a specialist in managing chronic pain, and has incorporated mindfulness meditation into her practice for more than 2 decades. Today she is sharing her experience by analyzing some of the most foundational research in the field of mindfulness and meditation.
 Mindfulness awareness has been described as the sustained attention to present moment awareness while adopting attitudes of acceptance, friendliness and curiosity. (1,2) In patients with persistent pain, mindfulness has shown to reduce pain intensity, anxiety and depression and in improve quality of life. (3,4) Researchers suggest that mindful awareness may work through 4 mechanisms: attention regulation, increased body awareness, enhanced emotional regulation and changes in perspective on self. (5)
Mindfulness awareness has been described as the sustained attention to present moment awareness while adopting attitudes of acceptance, friendliness and curiosity. (1,2) In patients with persistent pain, mindfulness has shown to reduce pain intensity, anxiety and depression and in improve quality of life. (3,4) Researchers suggest that mindful awareness may work through 4 mechanisms: attention regulation, increased body awareness, enhanced emotional regulation and changes in perspective on self. (5)
1. Attention Regulation: In chronic pan populations, improved attention regulation has been suggested to result in less negative appraisal of pain, greater pain acceptance and reduced pain anticipation. (6)
2. Body Awareness: Improved body awareness has been shown to help patients with chronic pain recognize the difference between muscle tension and relaxation, identify early warning signs that precede a pain flare and reduce maladaptive reactions to pain. (7)
3. Emotional regulation: Training in mindful awareness has been shown to enhance emotional regulation, improve mood and reduce anxiety and depression in patients with chronic pain. (6, 7, 8)
4. Changes in Perspective on Self: In a qualitative study, participants with chronic pain reported becoming less identified with their pain condition or diagnostic label. (7) They felt less “fragmented, experienced a greater integration of mind any body and described the experience of wellness even though they had a persistent pain condition.
I constantly see these changes in my patients who learn to be mindful. Empowered with a skillful way to pay attention, they have greater control over the direction of their mind and thoughts and an increase in body awareness that promotes the ability to relax and the self-regulation of their stress reaction. They avoid escalating distressing emotions and experience a renewed feeling of wholeness and well-being. I am delighted to share my training and experience in mindfulness and years of teaching mindfulness to patients in persistent pain through Herman and Wallace continuing education programs.
1. Kabat Zinn, J., 2013. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness. 2nd ed. New York: Bantam.
2. Bishop, S.R., Lau, M., Shapiro, S., et al., 2004. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), pp. 230–41.
3. Lakhan, S.E., Schofield, K.L., 2013. Mindfulness-based therapies in the treatment of somatization disorders: a systematic review and meta-analysis. PLoS One, 8(8), e71834.
4. Reiner, K., Tibi, L., Lipsitz, J.D., 2013. Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Med, 14(2), pp. 230-42.
5. Holzel, B.K., Lazar, S.W., Guard, T., et al., 2011. How Does Mindfulness Meditation Work? Proposing Mechanisms of Action From a Conceptual and Neural Perspective. Perspect Psychol Science, 6, pp. 537–59.
6. Brown, C.A., Jones, A.K., 2013. Psychobiological correlates of improved mental health in patients with musculoskeletal pain after a mindfulness based pain management program. Clin J Pain, 29(3), pp. 233-44.
7. Doran, N.J., 2014. Experiencing wellness within illness: Exploring a mindfulness-based approach to chronic back pain. Qual Health Res, 24(6), pp. 749-60.
8. Song, Y., Lu H., Chen H., et al. Mindfulness intervention in the management of chronic pain and psychological comorbidity: A meta-analysis. Int J Nurs Sci, 1(2), pp.215-23.
An interesting study aimed to objectively answer the following question: Does applying kinesiotape to promote a posterior pelvic tilt improve an active straight leg raise (ASLR) test in women who have sacroiliac joint pain and who habitually wear high-heeled shoes? To explain some of the rationale for the chosen technique and target population, the authors first describe prior research pointing out that use of high heels can lead to an anterior pelvic tilt position and increased lumbar lordosis. This position can slacken the sacrotuberous ligament and therefore reduce the ability of the ligament to create proper form closure, according to the article.
The research included 16 women with a mean age of 23.63. Inclusion criteria is as follows: having a habit of wearing high-heeled shoes (at least 4 times/week for 4 consecutive hours over at least 1 year), and having pain in both sacroiliac joints with the active straight leg raise test (ASLR). Additionally, having symptoms for at least 3 months, no proximal SIJ pain referral to the lumbar spine, and at least 3 of 5 positive SIJ tests (posterior shear test, pelvic torsion test, sacral thrust test, distraction and compression test) were needed for inclusion in the study.
Anterior pelvic tilt was measured using a palpation meter (PALM) before, immediately after application, 1 day after tape application, and immediately after removal of tape. ASLR was measured at same time points. The ASLR was self-scored on a 6-point scale ranging from “not difficult at all”” to unable to perform”. Kinesiotape was applied for a posterior pelvic tilt taping, and the tape was applied in the target position. I-type strips with ~50% of available tension were applied over the rectus abdominis and external oblique muscles. I-type strips with ~75% tension were placed from ASIS to PSIS aiming for mechanical correction of the anterior tilt.
Results of the study indicated a decrease inanterior pelvic tilt, both during and after tape application, and an improved active straight leg raise test. As this was a preliminary study, the results cannot be extrapolated to SIJ pain and dysfunction with other activities than the ASLR test. The degree of anterior pelvic tilt cannot also directly be correlated to sacroiliac joint pain and dysfunction, yet this research is very interesting, and demonstrates a simple method for affecting in the short term a patient’s mechanics as well as reports of function on the ASLR test, a very clinically simple and useful exam.
If you would like to learn more about evaluating and treating dysfunctions related to the sacroiliac joint, join Peter Philip at Sacroiliac Joint Evaluation and Treatment - New Orleans, LA this Sep 12, 2015 - Sep 13, 2015.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./











































