Isa Herrera, MSPT, CSCS teaches the "Low-Level Laser Therapy for Female Pelvic Pain Conditions" course for Herman & Wallace. Join her on October 3-4 in New York, NY to learn about this new modality!
Physical therapists deal with chronic pain that can be problematic to treat and manage on a daily basis. There is an arsenal of tools, exercises and techniques at their disposal, but many times using a modality can help accelerate the pain-relieving process.
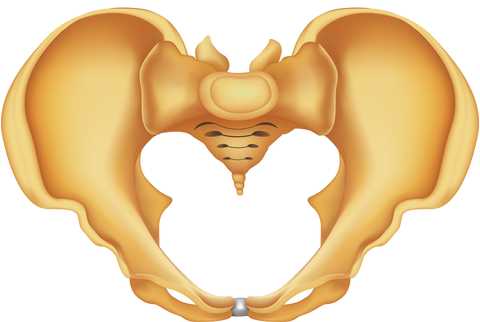
 At my healing center in New York City, we treat an extremely difficult type of chronic pain loosely classified under the umbrella term "pelvic pain". Pelvic pain can express itself as sacroiliac pain, hip bursitis, symphysis pubic dysfunction, and vulvodynia. Chronic pelvic pain is sometimes perceived as a "woman's issue", but we treat both men and women who have suffered for years with their conditions. We are challenged to think outside the box to provide relief for these patients.
At my healing center in New York City, we treat an extremely difficult type of chronic pain loosely classified under the umbrella term "pelvic pain". Pelvic pain can express itself as sacroiliac pain, hip bursitis, symphysis pubic dysfunction, and vulvodynia. Chronic pelvic pain is sometimes perceived as a "woman's issue", but we treat both men and women who have suffered for years with their conditions. We are challenged to think outside the box to provide relief for these patients.
'Secret Weapon' for Pain
Chronic pelvic pain is very different from other types of pain because it's intimately connected to our emotional, spiritual and psychological states, and can involve many symptoms in the nervous, endocrine, visceral, gynecological, urological and muscular systems. It can be very difficult to treat, and can require from six months to one year of physical therapy, depending on patient presentation and history.
This lengthy course of treatment requires a fresh approach to therapy and modalities. When I started treating this population I had many difficulties when it came to controlling their pain and I had to think differently. Electrical stimulation and ultrasound were not working as well as I'd hoped, and were providing insufficient pain relief to these patients.
I needed a modality that, when incorporated with my pelvic pain treatment protocols, could help produce immediate and long-lasting pain-relieving effects. I needed a modality that could significantly decrease pain within one session, and that my patients could believe in because of the results.
Low-level laser therapy (LLLT) proved to be my secret weapon when treating women with chronic pelvic pain. (I frequently call it "light therapy", because many patients are put off by the term "laser.")
I have been successfully using light therapy for nearly ten years. It helps my patients keep their pain at bay, and many request that I use it as part of their therapy. Of course, light therapy is only as good as the therapist using it. You have to apply this modality correctly, and use the science properly to maximize results.
LLLT was approved by the FDA in 2002. At that time, the modality was hailed by the New England Patriots and the U.S. Olympic Committee, among others, for its ability to help top athletes quickly return from injury. Endorsements from these organizations piqued my interest and I decided to research its principles.
I realized that LLLT could be used on many levels. LLLT is unique: it is a cellular bio-stimulator and is used to increase vitality of cells as well as processes that occur within the cell. Not all lasers are "created equal," and you have to be careful with the type you purchase.
Principles that must be taken into consideration include wavelength in nanometers, power in milliwatts, and total energy delivered in joules. In my pelvic pain protocols, I use LLLT on sensitive and painful tissues that are unable to tolerate any heat production.
Many lasers claim to be great therapeutic lasers, but actually produce heat within the tissue and cells. Any heat production has the potential to harm cells and destroy them. Heat production indicates the delivery of too many joules of energy per cycle. The goal with LLLT is to stimulate health and vitality within the cell to produce effects such as pain relief, collagen synthesis, resetting nerve potential, anti-inflammatory effects, and endorphin production.
New Look at Modalities
LLLT has changed the way I treat all pain syndromes. It's had such a positive impact that I've created laser protocols for vulvodynia, scar and bladder pain. I also created a special class for the Herman and Wallace Institute class for physical therapists who treat chronic pelvic pain. I encourage any colleagues specializing in this population to investigate this remarkable modality and to attend the class in October. If you are looking for something different and a modality that will change the way you treat come and learn how to use if effectively.
Reema Thakkar, PT, DPT has been a practicing Physical Therapist in Manhattan since 2011, specializing in orthopedics and vestibular rehabilitation. Reema has offered to share insights about her journey into pelvic rehabilitation.
Working as a physical therapist for 4+ years in Manhattan, I soon realized the need for pelvic floor rehabilitation within the pre- and post- natal community, as well as the geriatric community. Much of our population did not even know that this type of rehabilitation was effective or even available. Others, were simply embarrassed by the topic altogether. I decided - a complete novice in this field - to attend a Herman & Wallace PF course and see what was available as a resource for me, and my patients.
"I can happily report that as more and more patients catch wind of what I’m working on, their interest spurs."
My first course was definitely overwhelming. I had studied beforehand, like any eager student would, but I still felt as though it was my first day of PT school and I was scared I would “break” the patient. The candor and wit, in which each topic was presented to us that weekend, completely eased my mind. The pelvic floor, like any other daunting body part we had studied through our careers as PTs, was equally as influenced by the pulls and strains of our daily lives…and the muscles and joints needed our help.
I returned from my course full steam ahead. I felt equipped to at least begin this journey with my patients, and decided to further pursue my pelvic floor education, already registering for a follow up course in a few months. One thing that was imperative to my pelvic floor pursuit, was understanding the confines of an outpatient clinic. Even with having curtains around, patients were far less inclined to open up about their dysfunctions despite this assumed level of privacy. I had to ensure to schedule in times where one on one care with a closed door was possible. Another imperative factor was studying ahead of time. Being new to this care, I had to have a prescription from the MD or an intake form from the patient beforehand in order to research the night before.
I am still in the process of mastering this flow of practice. However I can happily report that as more and more patients catch wind of what I’m working on, their interest spurs. I can’t say they have all come in for a pelvic floor evaluation, especially the older generation, but they are certainly opening up a dialogue and asking some questions – which is all I can hope for.
That being said, I am even more confident in my ability to help the patients in question. Since returning from my first class, my greatest successes have been working with an elderly woman with severe uterine prolapse and a middle aged gentleman suffering from urinary incontinence s/p inguinal hernia repair. I can gladly report that their quality of life has greatly improved since beginning this care and I can only hope to guide them further in this process, with further success.
Reema has been a practicing Physical Therapist in Manhattan since 2011, specializing in orthopedics and vestibular rehabilitation. Reema is currently pursuing further training in order to become a certified Pelvic Rehabilitation Practitioner.
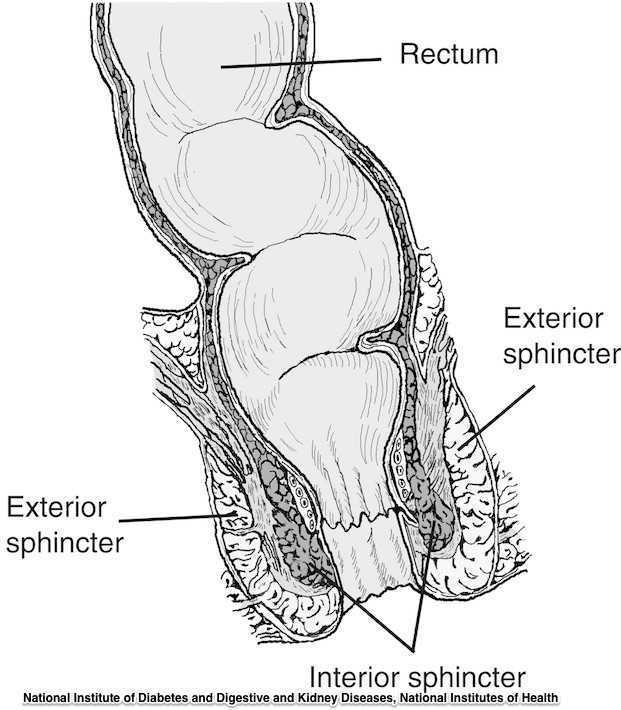
The phrase “rectal prolapse” may be easily confused with the term “rectocele” yet they may be very distinct clinical presentations. A rectocele refers to a prolapse of the posterior wall of the vagina that allows the rectum to bulge forward towards the posterior vaginal wall. This condition occurs most often in women rather than men. A rectal prolapse is a protruding of the rectum itself outside of the anal verge or opening. An overview article published in 2013 in the Journal of Gastrointestinal Surgery provides information about the condition that may assist the pelvic rehabilitation provider with valuable clinical concepts. Prior to becoming a full external prolapse, an internal intussusception may occur (and observed on defecography) and progress to include an external mucosal prolapse. Rectal prolapse may occur with or without other conditions of pelvic organ descent such as a cystocele or uterine prolapse. Although the prevalence of complete rectal prolapse is low, and occurs more often in women or in elderly patients, interference with quality of life may be significant.
Symptoms can include pain, difficulty emptying the bowels, bloody and or mucous discharge, urinary incontinence, and fecal incontinence or constipation. Patients may also complain of a lump or a bulge in the rectum that may or may not improve following a bowel movement. A complete rectal prolapse can be described as a full-thickness protrusion of the rectum through the anus. A more serious consequence of this condition is strangulation of the bowel. Features of a rectal prolapse often include a redundant sigmoid colon, levator ani muscle diastasis, and loss of the vertical position of the rectum, according to the article.
Treatment of a rectal prolapse may include surgery. Prior to surgery, a physical exam, colonoscopy, anoscopy, and possibly manometry and defecography may be completed. The surgical goals are to correct the prolapse, improve any complaints of discomfort, and to resolve bowel dysfunction. Surgical approaches may include abdominal or perineal approaches, minimally invasive versus open surgery, and techniques can include posterior versus ventral and rectopexy with or without sigmoidectomy. For more details about the specific approaches for rectal prolapse repair, see the linked article. The authors of this overview article point out that because “…there is a paucity of data evaluating the effectiveness and appropriateness of the various surgical techniques…”, there is not one single management strategy for each patient.
Nonsurgical recommendations for management of a rectal prolapse include appropriate daily fluid and fiber, suppositories or enemas if needed, biofeedback training, and pelvic floor muscle exercises. A patient may benefit from education in all of these concepts, before and/or following surgery. Pelvic rehabilitation providers are well poised to offer conservative management in these conditions prior to and following any needed surgery.
To learn more about rectal prolapse and related dysfunctions, join Dr. Lila Abbate, PT, DPT, MS, OCS at Bowel Pathology, Function, Dysfunction and the Pelvic Floor this November in New York, NY!
Herman & Wallace faculty member Lila Abbate instructs several courses in pelvic rehabilitation, including "Coccyx Pain, Evaluation and Treatment". Join Lila this October in Bay Shore, NY in order to learn evaluation and treatment skills for patients with coccyx conditions.
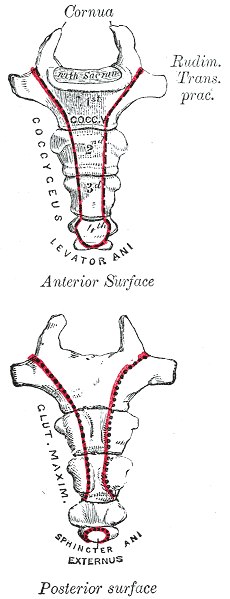
Case studies are relevant reading for physical therapists. Reviewing case studies puts you into the writer’s brain allowing you to synthesize your current knowledge of a particular diagnosis taking you through some atypical twists and turns in treating this particular patient type. In JOSPT, August 2014, Marinko & Pecci presented a very well-written case study of two patients with coccyx pain. By then, I had already written my Coccyx course and couldn’t wait to see what the authors had written. I eagerly downloaded the article to see another’s perspective of coccyx pain and their treatment algorithms, if any, were presented in the article. How were the author’s patients different than mine? What exciting relevant information can I add to my Coccyx course?
I believe that coccyx pain patients have more long-standing pain conditions than other patient types. For the most part, the medical community does not know what to do with this tiny bone that causes all types of havoc in patients’ pain levels. Sometimes treating a traumatic coccydynia patient seems so simple and I am bewildered as to why patients are suffering so long - and other times, their story is so complex that I wonder if I can truly help.
The longer I am a physical therapist, the more important has the initial evaluation become. Our first visit with the patient is time together that really helps me to create a treatment hypothesis. This examination helps me to put together an algorithm for treatment. I now hear their story, repeat back their sequence of events in paraphrase and then I ask: do you think there is any other relevant information, no matter how small or simple, that you think you need to tell me? Some will say, I know it sounds weird, but it all started after I twisted my ankle or hurt my shoulder or something like that. I assure them that we have the whole rest of the visit together and they can chime in with any relevant details. Determining the onset of coccyx pain will help you gauge the level of improvement you can expect to achieve. Coccyx literature states that patients who have coccyx pain for 6 months or greater will have less chance for resolution of their symptoms. However, none of the literature includes true osteopathic physical therapy treatment, so I am very bias and feel that this statement is untrue.
The coccyx course is a very orthopedically-based which takes my love of manual, osteopathic treatment and combines it with the women’s health internal treatment aspects so that we are able to move more quickly to get patient’s back on the path to improved function and recovery. The course looks at patients from a holistic approach from the top of their head down to their feet. In taking on this topic, I couldn’t do it without honing into our basic observation skills, using some of my favorite tools in my toolbox: Hesch Method, Integrated Systems Model, and traditional osteopathic and mobilization approaches mixing it with our internal vaginal and rectal muscle treatment skill set.
Marinko LN, Pecci M. Clinical decision making for the evaluation and management of coccydynia: 2 case reports. J Orthop Sports Phys Ther. 2014 Aug; 44(8): 615-21.
Varicoceles are enlarged veins that occur in the scrotum. They can be common in adolescent boys and men, with an incidence rate of approximately 15%. Because up to 1/3 of men dealing with infertility have a varicocele, a repair of this venous herniation may be a first line treatment for male fertility. Varicoceles are sometimes referred to as feeling like a "bag of worms" due to the distended veins that coil through the area (the U.S. National Library of Medicine provides a useful illustration). Although varicoceles may be painless, they are thought to be symptomatic in up to 10% of men. Symptoms can be dull, aching, throbbing, and can worsen with physical activity. Conservative care includes scrotal support, limiting physical activity, and using anti-inflammatory medications.

Pelvic rehabilitation providers may work with a male patient who complains of scrotal pain, and who has a known diagnosis of a varicocele. If the patient is unsure of such a diagnosis, questioning the patient about prior discussions with his medical providers may reveal that he was told about “enlarged veins in the scrotum” or similar description. Visual inspection may reveal the tell-tale appearance of distended veins inside the scrotum, and palpation may reveal a significant difference among sides (unless both sides are involved of course.) Physical examination for a varicocele is usually completed in supine and standing positions and may be palpable with or without Valsalva maneuver. Keeping in mind that the differential diagnosis for pain in the scrotum can include medical conditions such as testicular torsion, epididymitis, inguinal hernia, testicular tumor, hydrocele, epididymal cyst, or sperm granuloma, patients who have complaints must see an appropriate medical provider to rule out such conditions. It is also possible for a patient’s condition to change or worsen if a period of time has passed, with communication with the referring provider recommended. Post-surgical complications that should also be considered are inguinal hernia repair for nerve entrapment or vasectomy.
Because of the nerves traveling in the same pathway as the involved veins, we can also consider the neural tension potentially created from the increased venous distension creating either (or both) compression and drag. Surgical options may be discussed by the medical provider, and these might include a microsurgical ligation or a varicolectomy. According to Park & Lee (2013) “A varicocelectomy should be considered in patients with no alleviation of their pain after conservative management, including resting, scrotal elevation, and nonsteroidal anti-inflammatory analgesics.” Conservative management is exactly where we can fit in as providers of pelvic rehabilitation. Including a condition such as a varicocele in our differential diagnosis and treating planning can further our success with patients.
Herman & Wallace offers it's popular Male Pelvic Floor Function, Dysfunction and Treatment course next month in Denver, CO. See you there!
References
Park, Y. W., & Lee, J. H. (2013). Preoperative predictors of varicocelectomy success in the treatment of testicular pain. The world journal of men's health, 31(1), 58-63.
Shridharani, A., Lockwood, G., & Sandlow, J. (2012). Varicocelectomy in the treatment of testicular pain: a review. Current Opinion in Urology, 22(6), 499-506.
Guidelines for the management of 3rd and 4th degree tears were updated and published last month by The Royal College of Obstetricians & Gynaecologists. The purpose of the guidelines are to provide evidence-based guidelines on diagnosis, management and treatment of 3rd and 4th degree perineal tears. These types of tears are also referred to as obstetric anal sphincter injuries, or OASIS. The authors acknowledge an increased rate of reported anal sphincter injuries in England that may in part be due to increased awareness and detection of the issue. In terms of classification of anal sphincter injuries, the following is recommended (note the different levels at grade 3:
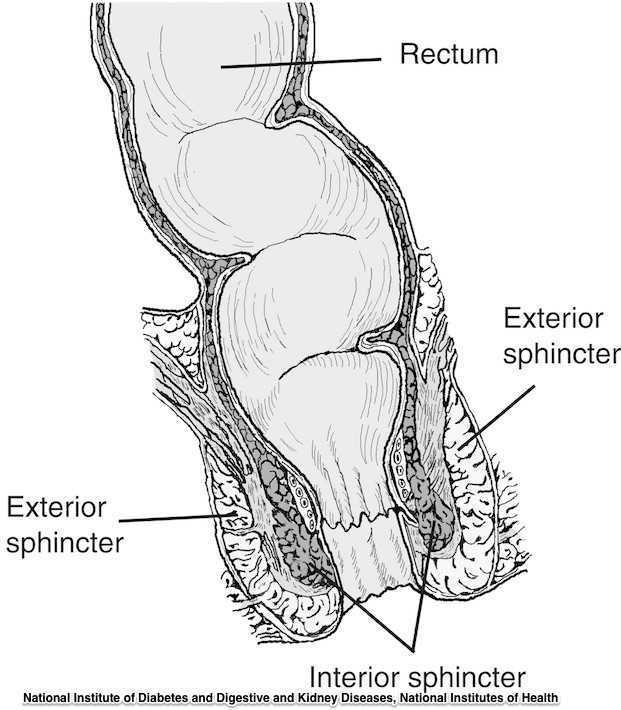
- 1st degree tear: injury to the perineal skin and/or the vaginal mucosa
- 2nd degree tear: injury to the perineum involving the perineal muscles but not involving the anal sphincter.
- 3rd degree tear: injury to the perineum involving the the anal sphincter complex
- Grade 3a tear: Less than 50% of the external anal sphincter (EAS) thickness is torn.
- Grade 3b tear: More than 50% of the EAS thickness is torn.
- Grade 3c tear: Both the EAS and the internal anal sphincter (OAS) are torn.
- 4th degree tear: Injury to the perineum involving the anal sphincter complex (EAS and IAS) and the anorectal mucosa.
Risk factors for anal injury are also outlined in the guidelines, although the authors point out that accurate prediction based on the risk factors is not reliable. The noted risk factors are as below:
- Asian ethnicity
- Nulliparity
- Birthweight greater than 4 kg (8.8 lb)
- Shoulder distocia
- Occipito-posterior position
- Prolonged 2nd stage labor
- Instrumented delivery
Recommendations worth noting include Level A evidence that warm compression during the 2nd stage of labor reduces the risk of OASIS. A noted best practice recommendation is that “Women should be advised that physiotherapy following repair of OASIS could be beneficial.” Guidelines such as these from The Royal College of Obstetricians & Gynaecologists can help in creating common language and in making recommendations that improve communication and expectations between patients and providers.
If you are interested in learning more about anal tears, Herman & Wallace offers several courses which cover the topic. For postpartum care specifically, check out Care of the Postpartum Patient.
The research on pelvic pain and specifically on sexual dysfunction has focused on heterosexual women, leaving a large gap in the clinically-based evidence. A study published last year in the Journal of Sex & Marital Therapy aimed to narrow this gap by studying the characteristics of vulvar pain in women in a variety of relationships. The associations between qualities such as love and communication were evaluated in relation to the participants' perceptions of how pain influenced their relationships. Within the research report, the authors establish that pelvic pain commonly causes pain and limitation with sexual function, and that queer women (defined in their work as women who identify as something other than heterosexual) also experience pain with sexual function.
"Of the 839 women, 31% reported genital pain, with 12% of the women with genital pain in a same-sex relationship, 67% in a mixed-sex relationship, and 21% being single"
The women in the study provided information about demographics, experiences of genital pain and pain characteristics. They completed surveys including the Dyadic Trust Scale (measures trust in a close relationship), the Rubin Love Scale (assesses level of romantic love), and the Communication Subscale of Evaluation and Nurturing Relationship Issues, Communication and Happiness Marital Satisfaction Scale (measures level of communication). Participants' average age was 25, and of the 77% who were in a relationship, most (60%) were in a mixed-sex relationship. Average length of relationships was 3 years, with nearly 84% of the women being white with some level of higher education.
Of the 839 women, 31% reported genital pain, with 12% of the women with genital pain in a same-sex relationship, 67% in a mixed-sex relationship, and 21% being single. Of the 260 women reporting genital pain, 39% identified as heterosexual, 15% identified as lesbian, and 46% identified as bisexual. The most common pain locations reported were inside the vagina (48%), in the pelvis or abdomen (45%), at the vaginal opening (39%), and 21% of the women reported global vulvar pain. From the data, the authors also report that women in same-sex relationships were likely to report that tampon insertion was painful.
The authors point out that challenges to healing for women who identify outside of heterosexual are many, and can include:
- homonegativity and heterosexism at a medical provider's office
- failure to disclose sexual identity due to fear of negative interaction
- fear that a symptom is linked to a sexual practice
- being in an unsupportive relationship or having poor adjustment within relationship
The limited research on sexual pain in women in same sex relationships has highlighted strengths within the relationships as well. Women in same sex relationships have been noted to have more effective communications skills, which may in turn foster better understanding of conditions such as pelvic pain. The authors concluded that while the characteristics of vulvar pain were similar across groups, there was a difference in the perception of pain impact on relationships. Better communication for same-sex couples and more love for mixed-sex couples was positively associated with impact on relationship. Of the women reporting pain, nearly half of the participants indicated that the pain negatively impacted their relationship in general, and 64% reported that the pain interfered with sexual health.
This type of research provides insight for pelvic rehabilitation clinicians and adds to our data base of considerations when working with women. The truth is that most of us were not provided adequate training in how to evaluate and manage issues of sexual health, nor were we provided with the means to value our own sexuality as a normal and healthy part of being. This lack requires education to fill in our own gaps, so that we can be of best service to our patients. If we are able to be present and nonjudgmental, our patients can in turn share openly and provide information that can direct best care. Holly Herman, co-founder of the Pelvic Rehabilitation Institute, offers a 2-day course in Sexual Medicine, so that providers can learn more about healthy sexuality as well as how to dialog with our patients.
Michelle Lyons is instructor of "Oncology and the Female Pelvic Floor: Female Reproductive and Gynecologic Cancers", among other Herman & Wallace courses. We thought you might like to hear her expert analysis of current research going on in the field of gynecologic oncology, and the benefits therapeutic yoga can have on patient rehabilitation. Take it away, Michelle!

More than 65,000 women are diagnosed with gynecologic cancers (vulvar, vaginal, cervical, ovarian, endometrial) in the United States each year (Sohl et al 2012). Treatment options for these women include surgery, chemotherapy, radiation and hormone therapy – all of which have the potential to have local, regional and global effects on a woman’s body. The pelvic rehab specialist is in a unique position to hugely improve quality of life issues for these women – dealing with issues directly associated with pelvic health (urinary, sexual and bowel function and dysfunction) as well as more global issues such as bone health, peripheral neuropathies and musculoskeletal dysfunctions.
Yoga has enormous potential as a therapeutic tool for gynecologic cancer survivors and as exercise prescription experts, we can add yoga as a multi-purpose tool to our skill-set.
Empirical research on therapeutic yoga has been ongoing for several decades, including several recent studies conducted with cancer patients and survivors. Although most of the research looking at the benefits of yoga for cancer survivors has been done in the context of breast and prostate cancers, we can safely extrapolate many of the benefits associated with oncology rehab yoga, including its immediately obvious ability to improve flexibility, strength, balance, but also the impact yoga can have on decreasing inflammation, improving sleep and raising quality of life scores in pelvic cancer survivors.
Recent papers by Dewhirst et al showed how moderate exercise can improve the efficacy of chemotherapy and radiation by decreasing tumour hypoxia – they also discovered that this may limit metastatic aggression.
We also know that exercise can be potent medicine when it comes to dealing with the effects of cancer treatments, especially fatigue, bone health and cardiovascular function, which may disrupt return to exercise (Kerry et al 2005). But pelvic cancer patients may face extra barriers when it comes to returning to exercise, such as pelvic pain and concerns about continence, as well as diminished flexibility, balance and strength. But as Blaney et al concluded in their 2013 paper ‘…however, the main barriers reported were those that had the potential to be alleviated by exercise.’ And in my opinion, this can be achieved by integrating yoga into our pelvic oncology rehab programs.
These recent and exciting research findings have encouraged me to add a therapeutic yoga lab session to my Oncology & the Pelvic Floor course, which I will be teaching in NY next month. This is the last chance to catch this course stateside this year so I hope you will join me in White Plains to explore the many ways we can make a serious impact on pelvic cancer survivorship (Bring your yoga mat!)
References:
Psychooncology. 2013 Jan;22(1):186-94.
Cancer survivors' exercise barriers, facilitators and preferences in the context of fatigue, quality of life and physical activity participation: a questionnaire-survey. Blaney JM1, Lowe-Strong A, Rankin-Watt J, Campbell A, Gracey JH.
Annals of Behavioral Medicine
April 2005, Volume 29, Issue 2, pp 147-153
A Longitudinal Study of Exercise Barriers in Colorectal Cancer Survivors Participating in a Randomized Controlled Trial
Kerry S. Courneya Ph.D., Christine M. Friedenreich Ph.D., H. Arthur Quinney Ph.D., Anthony L. A. Fields M.D., Lee W. Jones Ph.D., Jeffrey K. H. Vallance M.A., Adrian S. Fairey M.Sc.
JNCI J Natl Canc
Allison S. Betof, Christopher D. Lascola, Douglas H. Weitzel, Chelsea D. Landon, Peter M. Scarbrough, Gayathri R. Devi, Gregory M. Palmer, Lee W. Jones, and Mark W. Dewhirst
Modulation of Murine Breast Tumor Vascularity, Hypoxia, and Chemotherapeutic Response by Exercise
Pelvic rehabilitation providers commonly treat a variety of conditions associated with peripartum pelvic girdle dysfunction. This list of conditions includes coccyx pain, and a recent study aimed to identify risk factors which may lead to coccyx pain in the postpartum period. Dr. Jean-Yves Maigne, who is well known for providing foundational research on the topic of coccyx pain, and colleagues completed a case series of 57 postpartum women presenting to a specialty coccydynia clinic. Dynamic x-rays were taken to assess mobility of the coccyx, and data about delivery methods were collected. (A control group of 192 women were comprised of women who also presented to the clinic but who had coccyx pain from other causes.)
The authors found that the women reported immediate postpartum pain in the coccyx with sitting. Instrumentation was a common finding in regards to the patients’ deliveries. 50.8% of the deliveries utilized forceps while 7% were vacuum-assisted. An additional 12.3% of the deliveries were spontaneous and were described as “difficult.” A subluxation of the coccyx was observed in 44% of the women who developed coccyx pain after childbirth as compared to 17% of the controls. A fractured coccyx occurred in 5.3 % of the women. Body mass index (BMI) of more than 27 and having 2 or more vaginal deliveries was also associated with a higher prevalence of a subluxation of the coccyx.
Being unable to sit comfortably following childbirth could make a new parent’s life very difficult with limitations in activities such as sitting to feed the baby. Socially, being unable to sit comfortably can also limit many activities. The women in this study reported immediate tailbone pain with sitting, which can alert providers to a condition requiring both immediate and follow-up attention. Risk factors such as having a difficult delivery or use of forceps may also signal a patient history that may lead to coccyx pain.
If you are interested in learning more about managing coccyx pain, join Lila Abbate at Coccyx Pain Evaluation and Treatment in Bay Shore, NY on October 25-26! You may also be interested to learn more about treating patients during the postpartum period, in which case Care of the Postpartum Patient is right up your alley!
Today we are fortunate to hear from Barbara S. Rabin MSPT ATC PYTc, owner and practitioner at Holistic Physical Therapy in Gates Mills, OH. Barbara has more than 20 years of experience in orthopedic rehabilitation. Her perspective as an athletic trainer and orthopedic therapist highlights the many approaches practitioners can take when working with pelvic rehabilitation patients.
"We were reminded how all the muscles of the hip are intricately integrated into the pelvic floor and one can’t ignore the influence and interaction they have on each other."
My physical therapy career has been in the world of outpatient orthopedics and sports medicine. While in physical therapy graduate school I became a nationally certified athletic trainer, and most of my post graduate CEU’s have been in the orthopedic and sports medicine arena.
Stepping Outside the Comfort Zone
As an orthopedic PT, it was “safe” to study the pelvic girdle when I took Richard Jackson’s continuing education course in 1994 because it focused on muscles, ligaments, bones and nerves. However, I was leaving “safe territory” when I took Janet Hulme’s course, “Beyond Kegels: Evaluation and Treatment of Pelvic Muscle Dysfunction and Incontinence” in 1998. Long ago, back in gross anatomy lab in physical therapy school, we barely looked at the pelvic floor contents. Yes, we identified the digestive system but basically ignored all of the rest. Our mission was mostly to learn the muscles, ligaments, bones and nerves. After Janet Hulme’s course, I tried to offer incontinence rehabilitation at my place of employment at the time, but the idea was quickly dismissed. However, I am very glad to say that pelvic floor rehab is now commonly offered at most major hospitals and many clinics.
I continued my education of the pelvis and hip in several other courses and especially enjoyed one I attended last year called, "Extra-Articular Pelvic and Hip Labrum Injury: Differential Diagnosis and Integrative Management" by the Herman & Wallace Pelvic Rehabilitation Institute and taught by Ginger Garner PT ATC PYT. We were reminded how all the muscles of the hip are intricately integrated into the pelvic floor and one can’t ignore the influence and interaction they have on each other.
I was intrigued and wanted to learn more about the pelvic floor. I got another opportunity when I most recently attended an intimidating course for an “orthopedic sports medicine physical therapist” called, “Mobilization of Visceral Fascia for the Treatment of Pelvic Dysfunction - Level 1: The Urinary System” taught by Ramona Horton, MPT. I learned that externally mobilizing the bladder can often increase hip extension. Here was a combining of the fascial, pelvic floor, and orthopedic worlds!
Myofascial Release and Other Manual Therapy
I learned several manual therapy techniques in courses, and I took the best out of many but never specialized. As of late, I have been gladly drawn into the world of John F Barnes myofasical release. Studying and working with the fascia coincides with my holistic approach of rehabilitation, since the fascia is intricately woven throughout our body. The fascia was another thing we ignored in gross anatomy lab in physical therapy school. It was cut to move it out of the way so we could “get to the important stuff.” Even in that dead and embalmed state, the fascia was fascinating. It was strong and flexible at the same time. Now, with the advent of micro discography of the fascia by Dr. Jean-Claude Guimberteau (http://www.guimberteau-jc-md.com/en/biographie.php) we can view fascia in its live state and we can really see the phenomenal structure that it truly is.
Incorporating Yoga into Rehabilitation Practices
About eight years ago I took my first yoga class. I thought I was a conditioned athlete as a lifelong runner but I was humbled as I could not even balance on one leg for a minute. I noticed the physical and emotional benefits in myself and wanted to include yoga in the treatment of my patients. I had a patient who had physical issues from an eating disorder and needed supervision to exercise. I thought to myself that what she needed was not physical therapy but possibly meditation and relaxation. Even though I didn’t learn those techniques in PT school, I felt that I should be able to offer them to my patients. With one yoga class under my belt, in 2007, I entered into a 200 hour teacher training with Marni Task studying her combination of Jivamukti and Anusara yoga. I further continued my yoga training in 2011 with Ginger Garner PT, ATC, PYT of Professional Yoga Therapy Studies (http://proyogatherapy.org). Her school of medical yoga training, was just what I was looking for to merge my worlds of physical therapy and yoga.
Instead of looking at our patients as “pieces and parts,” referring to them as “the knee or the shoulder patient,” it is so important to see them as a whole. As an orthopedic PT I need to recognize that patients have not only a physical side of muscles, ligaments, bones and nerves, but other parts too that make them a whole person. Most likely I won’t specialize in pelvic pain or woman’s health but it is so important for me to be knowledgeable about this field to be the most effective therapist. In addition, it’s important to also go beyond the physical aspect and recognize patient’s psycho-emotional-social, spiritual, energetic, and intellectual aspects of their beings. Optimal health is achieved by recognizing and addressing all aspects of a patient.
And on that note, I’m going to continue merging all of my worlds of fascia, pelvic floor, orthopedics, and yoga, to address all the components of well-being, as I attend an upcoming course offered by Herman and Wallace called, Yoga for Pelvic Pain this month in Cleveland, Ohio.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./










































