Milk duct blockage is a common condition in breast feeding mother’s that can cause a multitude of problems including painful breasts, mastitis, breast abscess, decreased milk supply, breast feeding cessation, and poor confidence with decreased quality of life. A recent study in 2015 in The Journal of Women’s Health Physical Therapy1, showed that physical therapy (PT) maybe a helpful treatment for the lactating mother experiencing milk duct blockage when conservative measures have failed. Common conservative measures typically recommended are self-massage, heat, and regular feedings. The World Health Association, the American Academy of Pediatrics, and Academy of Breast Feeding Medicine, all recommend breast feeding as the primary source for nutrition for infants. There are many benefits to both the mother, and the infant, when breast feeding is used as the primary source for nutrition in infants. Having blocked milk ducts make it difficult and painful to breast feed and can lead to poor confidence for the mother and a frustrated baby as the milk supply could be reduced or inadequate. The primary health concern for blocked milk ducts is mastitis. Mastitis is defined as an infection of breast tissue leading to pain, redness, swelling, and warmth, possibly fever and chills and can lead to early cessation of breast feeding.
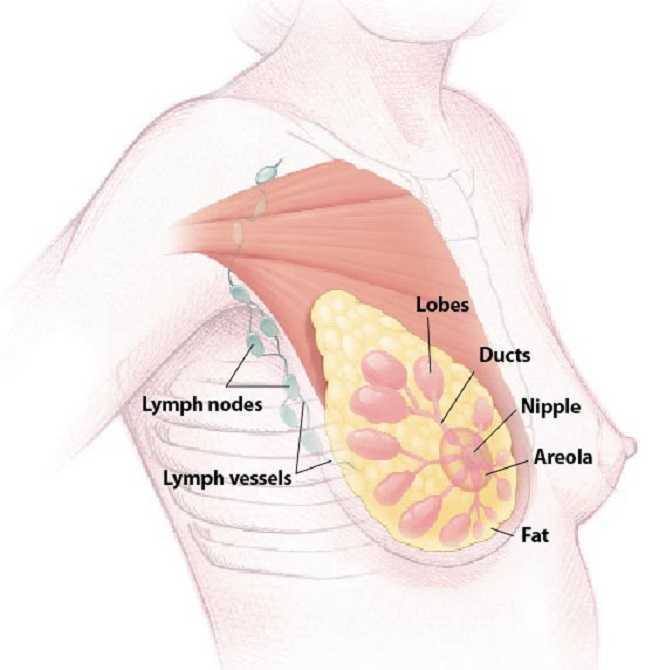 A blocked milk duct is not a typical referral to PT, however, this study outlined a protocol used for 30 patients with one or more blocked milk ducts that were referred to PT by a qualified lactation consultant. This study was a prospective pre/posttest cohort study. As an outcome measure, this study utilized a Visual Analog Scale (VAS) for 3 descriptive areas: pain, difficulty breast feeding, and confidence in independently nursing before and after treatment. The treatment protocol included moist heat, thermal ultrasound, specific manual therapy techniques, and patient education for treatment and prevention of the blockage(s). The thermal ultrasound and moist heating provided the recommend amount of heat to relax tissue around the blockage. Ultrasound also provided a mechanical effect that assists in the breaking up of the clog and increased pain threshold for the patient to improve tolerance to the manual clearing techniques. Next, the specific manual therapy was provided to directly unclog the blockage(s), and lastly the education provided was to help the patient identify and clear future blockages to prevent recurrence. 22 of the 30 patients were seen for 1-2 visits, 6 were seen for 3-4 visits, and none of the mother’s condition progressed to infective mastitis or developed breast abscess’s.
A blocked milk duct is not a typical referral to PT, however, this study outlined a protocol used for 30 patients with one or more blocked milk ducts that were referred to PT by a qualified lactation consultant. This study was a prospective pre/posttest cohort study. As an outcome measure, this study utilized a Visual Analog Scale (VAS) for 3 descriptive areas: pain, difficulty breast feeding, and confidence in independently nursing before and after treatment. The treatment protocol included moist heat, thermal ultrasound, specific manual therapy techniques, and patient education for treatment and prevention of the blockage(s). The thermal ultrasound and moist heating provided the recommend amount of heat to relax tissue around the blockage. Ultrasound also provided a mechanical effect that assists in the breaking up of the clog and increased pain threshold for the patient to improve tolerance to the manual clearing techniques. Next, the specific manual therapy was provided to directly unclog the blockage(s), and lastly the education provided was to help the patient identify and clear future blockages to prevent recurrence. 22 of the 30 patients were seen for 1-2 visits, 6 were seen for 3-4 visits, and none of the mother’s condition progressed to infective mastitis or developed breast abscess’s.
The results of the study showed the protocol used was helpful to ease pain, reduce difficulty with breast feeding, and improve confidence with independent breast feeding for lactating women that participated in the study. Although treatment of blocked milk ducts in lactating mothers is not a common PT referral, this study shows that PT may be one more helpful treatment for a patient experiencing this problem that is not responding to traditional conservative treatment. Since breast feeding is important to both mother and infant and is the primary recommended source for infant nutrition, it is important that a lactating mother receives quick, effective treatment for blocked milk ducts to prevent onset of mastitis and breast abscess that lead to early cessation of breast feeding. The cited study recommends that women who suspect a blocked milk duct or are having problems with breast feeding always seek care from a certified lactation consultant first, and that PT may be a referral that is made.
Cooper, B. B., & Kowalsky, D. S. (2015). Physical Therapy Intervention for Treatment of Blocked Milk Ducts in Lactating Women. Journal of Women’s Health Physical Therapy, 39(3), 115-126.
The day my son was born, my daughter had not defecated for 5 days, and her pain was getting pretty intense. My husband and his mom took her to Seattle Children’s Hospital for help, and they suggested using Miralax and sent them away. When they got back to my hospital room, my daughter was straining so hard it looked like she was about to give birth! Being physical therapists, my husband and I massaged her little muscles and told her to take deep breaths, and eventually she did the deed, yet not without a heart-breaking struggle. Little did I know then there is actually research to back up our emergency, instinctual technique.
 Zivkovic et al (2012) performed a study regarding the use of diaphragmatic breathing exercises and retraining of the pelvic floor in children with dysfunctional voiding. They defined dysfunctional voiding as urinary incontinence, straining, weakened stream, feeling the bladder has not emptied, and increased EMG activity during the discharge of urine. Although this study focuses primarily on urinary issues, it also includes constipation in the treatment and outcomes. Forty-three patients between the ages of 5 and 13 with no neurological disorders were included in the study. The subjects underwent standard urotherapy (education on normal voiding habits, appropriate fluid intake, keeping a voiding chart, and posture while voiding) in addition to pelvic floor muscle retraining and diaphragmatic breathing exercises. The results showed 100% of patients were cured of their constipation, 83% were cured of urinary incontinence, and 66% were cured of nocturnal enuresis.
Zivkovic et al (2012) performed a study regarding the use of diaphragmatic breathing exercises and retraining of the pelvic floor in children with dysfunctional voiding. They defined dysfunctional voiding as urinary incontinence, straining, weakened stream, feeling the bladder has not emptied, and increased EMG activity during the discharge of urine. Although this study focuses primarily on urinary issues, it also includes constipation in the treatment and outcomes. Forty-three patients between the ages of 5 and 13 with no neurological disorders were included in the study. The subjects underwent standard urotherapy (education on normal voiding habits, appropriate fluid intake, keeping a voiding chart, and posture while voiding) in addition to pelvic floor muscle retraining and diaphragmatic breathing exercises. The results showed 100% of patients were cured of their constipation, 83% were cured of urinary incontinence, and 66% were cured of nocturnal enuresis.
More recently, Farahmand et al (2015) researched the effect of pelvic floor muscle exercise for functional constipation in the pediatric population. Stool withholding and delayed colonic transit are most often the causes for children having difficulty with bowel movements. Behavioral modifications combined with laxatives still left 30% of children symptomatic. Forty children between the ages of 4 and 18 performed pelvic floor muscle exercise sessions at home, two times per day for 8 weeks. The children walked for 5 minutes in a semi-sitting (squatting) position while being supervised by parents. The patients increased the exercise duration 5 minutes per week for the first two weeks and stayed the same over the next six weeks. The results showed 90% of patients reported overall improvement of symptoms. Defecation frequency, fecal consistency and decrease in fecal diameter were all found to be significantly improved. Although not statistically significant, the number of patients with stool withholding, fecal impaction, fecal incontinence, and painful defecation decreased as well.
Parents may not be as aware of their children’s voiding habits once they are cleared from diaper duty after successful potty training occurs. To help prevent issues, keep the basics covered, such as making sure children are exercising regularly or being active, drinking plenty of fluids, and eating a diet that includes plenty of fiber. My daughter was only 26 months old when her constipation became a problem, so the stool softener was ultimately the way to go at that time, and everything worked out naturally over the next year. If she were still experiencing functional constipation, I would be delighted to know teaching her pelvic floor exercises (relaxation being the key aspect) and diaphragmatic breathing could be effective for keeping my crazy little girl regular in at least that area of her life!
Zivkovic V, Lazovic M, Vlajkovic M, Slavkovic A, Dimitrijevic L, Stankovic I, Vacic N. (2012). Diaphragmatic breathing exercises and pelvic floor retraining in children with dysfunctional voiding. European J ournal of Physical Rehabilitation Medicine. 48(3):413-21. Epub 2012 Jun 5.
Farahmand, F., Abedi, A., Esmaeili-dooki, M. R., Jalilian, R., & Tabari, S. M. (2015). Pelvic Floor Muscle Exercise for Paediatric Functional Constipation.Journal of Clinical and Diagnostic Research : JCDR, 9(6), SC16–SC17. http://doi.org/10.7860/JCDR/2015/12726.6036
The 2012 guidelines for the treatment of overactive bladder in adults (updated in 2014) recommends as first line treatment behavioral therapies. These therapies include bladder training, bladder control strategies, pelvic floor muscle training, fluid management- all tools that can be learned in the Institute’s Pelvic Floor Level 1 course. These behavioral therapies may also be combined with medication prescription, according to the guideline.
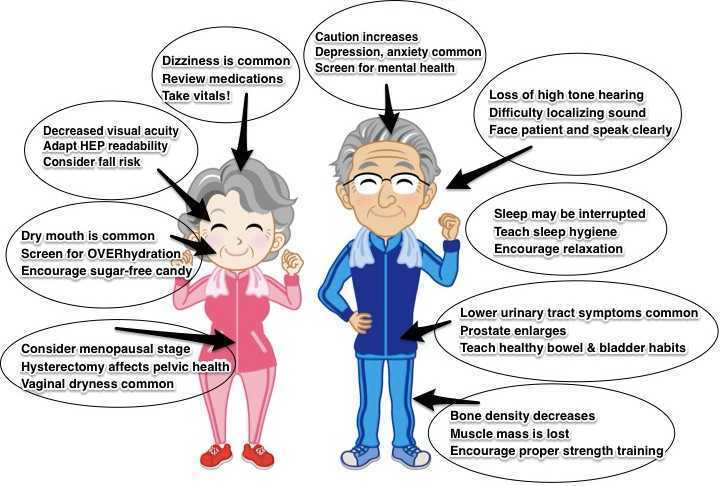 When medications are prescribed for overactive bladder, oral anti-muscarinics or oral B3-adrenergic agonists may be prescribed. Although these drugs may help to relax smooth muscles in the bladder wall, the side effects are often strong enough to make the medication difficult to tolerate. Side effects of constipation and dry mouth can occur, and when they do, patients should communicate that to their physician so that the medication dosage or class can be evaluated and modified if possible. We know that patients who have constipation tend to have more bladder dysfunction, so patients can get stuck in a vicious cycle.
When medications are prescribed for overactive bladder, oral anti-muscarinics or oral B3-adrenergic agonists may be prescribed. Although these drugs may help to relax smooth muscles in the bladder wall, the side effects are often strong enough to make the medication difficult to tolerate. Side effects of constipation and dry mouth can occur, and when they do, patients should communicate that to their physician so that the medication dosage or class can be evaluated and modified if possible. We know that patients who have constipation tend to have more bladder dysfunction, so patients can get stuck in a vicious cycle.
Although patients and their medications are screened at their prescriber’s office and often at the pharmacy, it is important to remember that therapists are an important part of this safety mechanism. Patients may not be candidates for anti-muscarinics if they have narrow angle glaucoma, impaired gastric emptying, or a history of urinary retention. When patients are taking other medications with anticholinergic properties, or are considered frail, adverse drug reactions can also occur. Our geriatric patients may have some additional considerations, not just in medication screening, but also in evaluation and intervention. If you are interested in learning more about pelvic rehabilitation for those in the geriatric population, check out our new continuing education course, Geriatric Pelvic Floor Rehabilitation with Heather S. Rader, PT, DPT, BCB-PMD. The next opportunity to take the class is January 16-17, 2016 in Tampa.
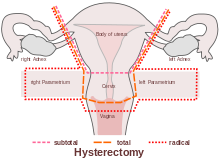
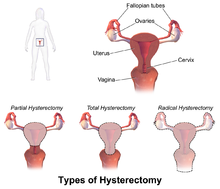 ACOG (American College of Obstetrics and Gynecology) describes hysterectomy as a treatment of last resort, but studies show that anywhere from 10 to 90% of hysterectomies performed in the United States are not medically necessary, evidenced by the fact that today, approximately 90 percent of hysterectomies are performed electively. Corona et al stated: ‘…that alternatives to hysterectomy are underutilized in women undergoing hysterectomy for AUB, uterine fibroids, endometriosis, or pelvic pain. The rate of unsupportive pathology when hysterectomies were done for these indications was 18%.’
ACOG (American College of Obstetrics and Gynecology) describes hysterectomy as a treatment of last resort, but studies show that anywhere from 10 to 90% of hysterectomies performed in the United States are not medically necessary, evidenced by the fact that today, approximately 90 percent of hysterectomies are performed electively. Corona et al stated: ‘…that alternatives to hysterectomy are underutilized in women undergoing hysterectomy for AUB, uterine fibroids, endometriosis, or pelvic pain. The rate of unsupportive pathology when hysterectomies were done for these indications was 18%.’
The US has the highest rate of hysterectomy in the industrialized world; it is the second most common surgical procedure carried out on women. 1 in 3 American women have their uterus removed by the age of 60, with the highest rates in women aged 30-54 (according to Corona et al in 2014, one in five women may not need it).
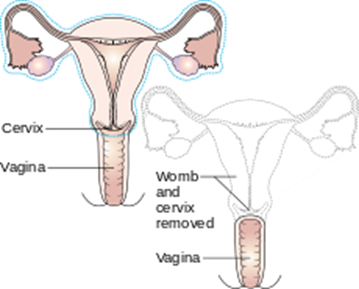 Reasons for hysterectomy include cancer, bleeding with childbirth and severe infection with uterine damage, all of which make up about 10% of cases. The other 90% are made up of medical, non-surgical and other surgical reasons, such as for menstrual cramps, heavy bleeding and fibroids. Unfortunately, too many women are also having hysterectomies as a treatment option for endometriosis (instead of laparoscopic excision, histological confirmation and pelvic rehab follow up)
Reasons for hysterectomy include cancer, bleeding with childbirth and severe infection with uterine damage, all of which make up about 10% of cases. The other 90% are made up of medical, non-surgical and other surgical reasons, such as for menstrual cramps, heavy bleeding and fibroids. Unfortunately, too many women are also having hysterectomies as a treatment option for endometriosis (instead of laparoscopic excision, histological confirmation and pelvic rehab follow up)
Numerous women who undergo hysterectomy remain unclear about the details of their surgical procedures or indeed the implication for short and long term recovery. Clinically, I have seen many women who assume that as they have had a ‘Total’ Hysterectomy, that includes removal of their ovaries (Total vs Partial Hysterectomy generally refers to cervical preservation). I have also see many women confused as to why their recovery from what has been a laparoscopic surgery, with small incisions, is taking so long. A surgical colleague described it well in my opinion: ‘A laparoscopic hysterectomy is major abdominal/pelvic surgery with tiny incisions’.
 In Part Two of this blog, I will discuss the sequelae of hysterectomy and the key role of pelvic rehab. Interested in learning more about Endometriosis, Fertility and Hysterectomy? Join me in Denver in January!
In Part Two of this blog, I will discuss the sequelae of hysterectomy and the key role of pelvic rehab. Interested in learning more about Endometriosis, Fertility and Hysterectomy? Join me in Denver in January!
The Boston Women's Health Book Collective. Our Bodies, Ourselves: A New Edition For A New Era. New York: Touchstone, 2005., Centers for Disease Control and Prevention Online. "Hysterectomy Surveillance" --- United States, 1994,1999, 2002. http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5105a1.htm
‘Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative’ Corona et al (Presented in oral and poster format at the 4oth Annual Scientific Meeting of the Society of Gynecologic Surgeons, Scottsdale March 24-26 2014)
The eve of my daughter’s 5th birthday has me reminiscing about my first pregnancy. I had recently surrendered my ACL on a ski slope and was contemplating surgery when I got confirmation I was pregnant. A seasoned surgeon had told me if I just wanted to return to running and not ski or do cutting sports (without a brace, anyway), I would probably be fine; so, I chose to forego the surgery and was running again 7 weeks later. Being my first pregnancy, I was not sure how hormones would affect my knee stability without an ACL or if the impact was safe for me and the baby or if my doctor would approve of my exercise choice of running. After all, pending ligamentous laxity from hormonal changes made running without an ACL seem risky while pregnant; but, runners tend to be, well, stubborn, when it comes to being able to run.
 Deghan et al (2014) discuss the hormone relaxin and its effect on bone, muscle, tendon, ligaments, and cartilage. Interestingly, relaxin actually plays a role in the healing and remodeling of certain tissues in the body such as muscle and bone. However, the article also emphasizes how relaxin has been shown to reduce the integrity of the ACL and put female athletes at risk for injury. Lucky for me, that hormone couldn’t have its way with my knee since the ACL was already gone!
Deghan et al (2014) discuss the hormone relaxin and its effect on bone, muscle, tendon, ligaments, and cartilage. Interestingly, relaxin actually plays a role in the healing and remodeling of certain tissues in the body such as muscle and bone. However, the article also emphasizes how relaxin has been shown to reduce the integrity of the ACL and put female athletes at risk for injury. Lucky for me, that hormone couldn’t have its way with my knee since the ACL was already gone!
A study in the British Journal of Sports Medicine just published online October 4, 2015, encourages running and other high-impact sports before pregnancy to decrease the risk of pelvic girdle pain. The patients engaging in such exercises prior to being pregnant showed a 14% lower risk of having pelvic girdle pain during pregnancy. Out of 4069 women, 12.5% of the 10.4% of women who experienced pelvic pain were non-exercisers pre-pregnancy. The women who exercised 3-5 days per week and participated in high-impact aerobic exercise prior to being pregnant had less pelvic pain while pregnant.
Tenforde et al (2015) investigated the habits of competitive runners during pregnancy as well as breastfeeding. Out of 110 female runners, 70% continued to run during their pregnancy; however, only 31% continued into their 3rd trimester. Only 3.9% of the women got injured while running pregnant. In general, the competitive runners reduced their intensity and volume and ran primarily for fitness and health. The 84.1% of the women who ran during breastfeeding reported less postpartum depression and no negative impact on breastfeeding.
Looking back at my running log, I ran 3 miles under 10-minute pace two days before going into labor, and my daughter was even 9 days late. I continued to run because I love it and, quite simply, because I could. Personally, my blood pressure, weight, and glucose levels stayed healthy throughout the pregnancy. Even without an important stabilizing ligament in my knee and some extra pounds, I never experienced joint pain while running. On the trail where I ran, I got mixed responses from people coming the other way - mostly encouragement, but also some looks of disappointment or disgust (I didn’t say it was pretty) and an occasional know-it-all “warning.” Ultimately, any woman who has been running prior to pregnancy should be able to continue some level of running through the trimesters until her own body, the obstetrician, or a hard-kicking baby gives a reason to stop.
Dehghan, F., Haerian, B. S., Muniandy, S., Yusof, A., Dragoo, J. L., & Salleh, N. (2014). The effect of relaxin on the musculoskeletal system. Scandinavian Journal of Medicine & Science in Sports, 24(4), e220–e229. http://doi.org/10.1111/sms.12149
Owe KM, Bjelland EK, Stuge B, Orsini N, Eberhard-Gran M, Vangen S. (4 October 2015). Exercise level before pregnancy and engaging in high-impact sports reduce the risk of pelvic girdle pain: a population-based cohort study of 39,184 women. British Journal of Sports Medicine. pii: bjsports-2015-094921. doi: 10.1136/bjsports-2015-094921. [Epub ahead of print]
Tenforde AS, Toth KE, Langen E, Fredericson M, Sainani KL. (2015 Mar). Running habits of competitive runners during pregnancy and breastfeeding. Sports Health.;7(2):172-6. doi: 10.1177/1941738114549542.
Although awareness of pelvic rehabilitation is growing, patients who are referred for pelvic rehabilitation usually have more questions than the average patient about attending therapy. This can mean that you as a provider are burdened with a lot of phone calls or emails that go something like this: can I come to the clinic if I’m on my period? what are you going to do? are you familiar with my condition? how long will it take to get better? Consider how often these questions occur with patients who have knee pain, or headaches, and you may find that pelvic rehab is perceived by patients as quite unique from other types of rehab. How can you avoid trying to find time in your busy clinical schedule to tackle these additional communications? You can start by educating your front desk to handle patient care questions related to pelvic rehab, such as the following frequently asked questions:

- Do I need a referral from a doctor?
- What will we do on my first visit?
- What is biofeedback?
- What is ____________ (proctalgia fugax, interstitial cystitis), etc?
- I have my period, should I reschedule?
- Do you do internal work?
- Will my insurance cover this?
It is likely that the patient will ask to speak directly with the therapist, so you can first encourage your support personnel to politely inquire if there is something he or she could help in answering. Create a list of conditions along with a brief description of its definition, and a few examples of skills that a pelvic rehab provider has to offer. Your support staff can also offer to mail a brochure or flyer that you create which answers some of the frequently asked questions. Providing an “FAQ” section on your website that can be referred to may also decrease some of the stress of trying to play phone tag. Make no mistake that if you DO have the time to follow-up with a patient who has a question, you may create a connection that is really important for that patient in regards to scheduling an appointment. On the other hand, if you don’t have time set aside in your day for such calls or emails, you risk having the patient not get her questions answered. A form (on your site or as a written resource) might have some of the commonly asked questions written out, and you could use the ones below as an example to get you started.
Do I need a referral from a doctor?
Most patients can attend a physical therapy visit without having a prescription or written referral from a doctor or other referring provider. Insurance companies, however, may insist that you have a referral in order for you or your therapist to receive payment. Even if you do not need a referral from a medical provider, your therapist may require that you have seen a medical provider for your condition. Many conditions involving the pelvis can be medical in nature and require checking for more serious conditions before coming to the clinic. It is also helpful to have a medical provider with whom your therapist can coordinate care and discuss your health as a team.
What will we do on my first visit?
First, we will talk about what concerns or symptoms you have. Your therapist will also look over any forms you filled out to learn more about your history. The exam will be discussed with you so that you can have any questions answered. Your therapy exam may include general movement like bending forward and backward, seeing how you move your body, and specific tests of your joints, muscles, and nerves. For pelvic rehabilitation, an assessment of your pelvic muscles internally (through the rectum or vaginal canal) may be valuable.
Will we use biofeedback? (What is biofeedback?)
Your therapist may use surface EMG (electromyography), a form of biofeedback. This may involve placing some sticky sensors on your body so you and your therapist can get a better idea of how you are coordinating muscle activity in the abdomen or pelvis. Biofeedback means that you will be able to get information about how your muscles are working, and in therapy this is often displayed as graphs or bars on a screen. An internal sensor for the vaginal or rectal canal may also be used.
(For those menstruating) Should I reschedule if I have my period?
It is usually not necessary to reschedule if you are on your cycle, so you are welcome to keep your appointment.
Commonly in physical therapy we treat patients with osteopenia or osteoporosis, however, they are usually in our office for another diagnosis such as back, hip, or pelvic pain as the primary complaint and we learn about the osteoporosis from health history review. Physical therapy is an opportunity to provide them with not just relief from their primary complaint, but a chance to learn from a professional how to move in a more healthy way and learn the right ways to exercises to make a regular routine that can help them to protect their body and even slow or stop bone mineral density loss. This is important as the primary concern for a patient with the diagnosis of osteoporosis is risk of fracture (especially of the hip or spine) due to minimal trauma because of low bone mineral density. So let’s make sure we are giving patients comprehensive exercise programs that address their primary complaint, however be comprehensive and include exercise modes that may reduce fractures and may improve bone mineral density.
 An interesting article by Palombaro et al1 in 2013 from Physical Therapy discusses a Cochrane review by Howe et al2 and applies the findings from this review to an example patient similar to the participants reviewed in the study. The goal of the article is to link evidence in the literature with how we practice as PT’s. The topic explored in the systematic review by Howe et al was exercise for the management of osteoporosis in women postmenopause and which exercise approaches reduce the loss of bone mineral density or reduce chance of fractures in women who are healthy postmenopause. The systematic review2 included 43 randomized controlled studies of postmenopausal women age 45-70 where the intervention groups included exercises that improved aerobic capacity or improved aerobic capacity and muscle strength and had a comparison group completing “usual activity: or placebo intervention. The duration of exercise lasted from 6 months to 2 years in the various studies. The results of the review demonstrated decreased bone loss (of the spine or hips) in groups who performed any type of exercise compared to the control groups. The review also performed additional sub group analysis to take into account the various types of exercise programs in the studies and found favorable effect for all types of exercises completed (dynamic, low force, high force, weight bearing, or non-weight bearing) all had favorable effect on bone density. The take home message from this systematic review is that exercise programs combining various forms of exercises lasting 6 months to 2 years resulted in reduced risk for fracture, and a slightly beneficial effect on bone mineral density of the spine, trochanter, and neck of the femur in postmenopausal women with osteoporosis.
An interesting article by Palombaro et al1 in 2013 from Physical Therapy discusses a Cochrane review by Howe et al2 and applies the findings from this review to an example patient similar to the participants reviewed in the study. The goal of the article is to link evidence in the literature with how we practice as PT’s. The topic explored in the systematic review by Howe et al was exercise for the management of osteoporosis in women postmenopause and which exercise approaches reduce the loss of bone mineral density or reduce chance of fractures in women who are healthy postmenopause. The systematic review2 included 43 randomized controlled studies of postmenopausal women age 45-70 where the intervention groups included exercises that improved aerobic capacity or improved aerobic capacity and muscle strength and had a comparison group completing “usual activity: or placebo intervention. The duration of exercise lasted from 6 months to 2 years in the various studies. The results of the review demonstrated decreased bone loss (of the spine or hips) in groups who performed any type of exercise compared to the control groups. The review also performed additional sub group analysis to take into account the various types of exercise programs in the studies and found favorable effect for all types of exercises completed (dynamic, low force, high force, weight bearing, or non-weight bearing) all had favorable effect on bone density. The take home message from this systematic review is that exercise programs combining various forms of exercises lasting 6 months to 2 years resulted in reduced risk for fracture, and a slightly beneficial effect on bone mineral density of the spine, trochanter, and neck of the femur in postmenopausal women with osteoporosis.
At the end of this article1 the authors give a case of an active, postmenopausal female patient with history of osteopenia without a fracture seeking PT for an unrelated complaint. The authors took the findings from this review and showed the relevance of the findings, applying it to the patient and the outcome of care for this patient when giving her an exercise program. We can implement findings from this review simply to the common question posed by our patients… “what exercises should I be doing to help with my osteoporosis?”
Exercises for a patient with osteoporosis should be forms of exercises that may improve bone density by loading bones (weight bearing exercise) and by increasing muscle mass (strengthening resistive exercise) to produce mechanical load and stress to the bone. Also as we age we tend to experience changes with not just a reduction of bone mineral density, but also a reduction of muscle mass. Additionally complicating the natural progression of aging are balance and gait changes leading to impaired physical performance. We should be giving our patients a comprehensive exercise program including safe weight bearing exercises and a strengthening program. Common examples of weight bearing exercises include regular walking, jogging, jumping, dancing, and racquet sports. Common examples of strengthening activities would include use of resistive exercises for upper and lower body with bands, free weights or resistive equipment. All of these classifications of exercise were considered as beneficial in the review.
To learn more about helping postmenopausal patients, consider joining Michelle Lyons, PT, MISCP for "Menopause Rehabilitation and Symptom Management". This course will be taking place March 19, 2016 - March 20, 2016 in Atlanta, GA. Another great resource to consider is "Geriatric Pelvic Floor Rehab: Modifying Treatments for Seniors and Older Patients" with Heather S. Rader, PT, DPT, BCB-PMD, taking place January 16-17, 2016 in Tampa, FL.
1 Palombaro, K. M., Black, J. D., Buchbinder, R., & Jette, D. U. (2013). Effectiveness of exercise for managing osteoporosis in women postmenopause. Physical Therapy, 93(8), 1021-1025.
2 Howe, T. E., Shea, B., Dawson, L. J., Downie, F., Murray, A., Ross, C., ... & Creed, G. (2011). Exercise for preventing and treating osteoporosis in postmenopausal women (Review).
Earlier this year, 3 prominent societies representing pelvic health met to discuss and update terminology for vulvar pain. The result is the “2015 Consensus Terminology and Classification of Persistent Vulvar Pain.” A complete list of the updated terminology can be accessed on the website of the International Pelvic Pain Society. The updated document takes into account the additions of the terms Primary versus Secondary Vulvodynia, intermittent versus persistent pain, and considers research-based interventions for the suspected etiologies of pain. Some of the other updates are highlighted below.
- Replace the term “unprovoked” with “spontaneous”
- Use the term “vulvar” rather than “vulvodynia” in the title of the terminology
- Vulvar pain definition removes the word “burning” from description
Vulvar pain can have a known cause, and the categories within vulvar pain caused by a specific disorder are: infectious, inflammatory, neoplastic, neurologic, trauma, iatrogenic, and hormonal deficiencies. Vulvodynia, defined as vulvar pain at least 3 months in duration, and without a clear identifiable cause, is described as having “potential associated factors.” There are also descriptor terms such as localized, provoked, or mixed, and terms such as intermittent, persistent, constant, immediate or delayed.
The terminology document recognizes that a patient may have a specific condition or diagnosis, and also be diagnosed with vulvodynia. As this consensus document is designed to replace the ISSVD terminology from the 2003 publication, becoming familiar with the updates is valuable for pelvic rehabilitation providers. The evaluation and treatment of vulvar pain is introduced in the Insitute’s Pelvic Floor Level 1 continuing education course, and further developed in the Level 2B course. For an immersion in the topic of vulvar pain, check out the Institute’s course on Vulvodynia: Assessment and Treatment instructed by Dee Hartmann. Your next opportunity to take the course is this March in Houston.
Can patients benefit from a non-face-to-face treatment program for stress urinary incontinence? A recent study addressing this question was published in the British Journal of Urology International. This randomized, controlled trial utilized online recruitment of 250 community-dwelling women ages 18-70 years. Criteria was stress urinary incontinence (SUI) at least 1x/week, diagnosis based on self-assessment questionnaires, 2 days of bladder diaries, as well as a telephone interview with a urotherapist. The Outcomes tools included the International Consultation on Incontinence Questionnaire Short Form (ISIC-UI SF), the Lower Urinary Tract Symptoms Quality of Life (ICIQ-LUTSqol), the Patient Global Impression of Improvement, health-specific quality of life (EQ-VAS), use if incontinence aids, and satisfaction with treatment.
 The participants were randomized into 2 pelvic floor muscle training groups: an “internet-based” group (n=124) and a group who were sent information in the mail (n=126). The internet-based program contained information about pelvic muscle contractions (8 escalating levels of training), behavioral training related to lifestyle changes. The internet group received email support from the urotherapist, and the postal group did not. Pelvic floor muscle training was instructed at at least 8 contractions 3 times/day. After the 3 month training period, the internet-based treatment group was advised to continue pelvic floor muscle training 2-3 times/week, whereas the mail training group were not given any advice about continued training frequency. Follow-up data was collected at 4 months post-intervention, at 1 year and 2 years. At 2 years follow-up, 38% of the participants were lost from the study.
The participants were randomized into 2 pelvic floor muscle training groups: an “internet-based” group (n=124) and a group who were sent information in the mail (n=126). The internet-based program contained information about pelvic muscle contractions (8 escalating levels of training), behavioral training related to lifestyle changes. The internet group received email support from the urotherapist, and the postal group did not. Pelvic floor muscle training was instructed at at least 8 contractions 3 times/day. After the 3 month training period, the internet-based treatment group was advised to continue pelvic floor muscle training 2-3 times/week, whereas the mail training group were not given any advice about continued training frequency. Follow-up data was collected at 4 months post-intervention, at 1 year and 2 years. At 2 years follow-up, 38% of the participants were lost from the study.
Within both groups, the authors report that the International Consultation on Incontinence Questionnaire Short Form (ISIC-UI SF) and the Lower Urinary Tract Symptoms Quality of Life (ICIQ-LUTSqol) showed “highly significant improvements” after 1 and 2 years compared to baseline data. Much of the improvement occurred within the first 4 months of the study “…and then persisted throughout the follow-up period.” When comparing the internet group to the mail-only group, the perception of improvement following treatment was higher. Approximately 2/3 of the women in both groups reported satisfaction with the treatment even at the 2 year follow-up. The authors conclude that the internet or mail-based exercise programs may “…have the potential to increase access to care and the quality of care given to women with SUI [stress urinary incontinence] in a sustainable way.” Additionally, not all patients will improve significantly unless they have one-on-one intervention, leaving plenty of patients who do need our direct care.
If you would like to learn more about exercise prescription for urinary incontinence, consider attending one of Herman & Wallace's many continuing education courses.
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./










































