In a 2018 article by Holly Tanner, she explains how managing a medical crisis such as a cancer diagnosis can be overwhelming for an individual. ‘Faced with choices about medical options, dealing with disruptions in work, home, and family life often leaves little energy left to consider sexual health and intimacy. Maintaining closeness, however, is often a goal within a partnership and can aid in sustaining a relationship through such a crisis.” Research shows that cancer treatment is disruptive to sexual health. Intimacy is a larger concept that may be fostered even when sexual activity is impaired or interrupted.
Prostate cancer treatment can change relational roles, finances, work-life, independence, and other factors including hormone levels. (1) Exhaustion (on the part of the patient and the caregiver), role changes, changes in libido, and performance anxiety can create further challenges. (1, 3, 4) Recovery of intimacy is possible, and reframing of sexual health may need to take place. Most importantly, these issues need to be talked about, as a renegotiation of intimacy may need to take place after a diagnosis or treatment of prostate cancer. (2)
If a patient brings up sexual health, or the practitioner encourages the conversation, many research-based suggestions can be provided to encourage recovery of intimacy including:
• Redefining sex to include other sexual practices beyond penetration, such as massage or touching, cuddling, talking, use of vibrators, medication, aids such as pumps (5)
• Participation in couples therapy to understand their partner’s needs, address loss, be educated about sexual function (7)
• Participation in “sensate focus” activities (developed by Masters & Johnson in the 1970s as “touch opportunities”) with appropriate guidance (6)
Holly continues to share that “Within the context of this information, there is an opportunity to refer the patient to a provider who specializes in sexual health and function. While some rehabilitation professionals are taking additional training to be able to provide a level of sexual health education and counseling, most pelvic health providers do not have the breadth and depth of training required to provide counseling techniques related to sexual health - we can, however, get the conversation started, which in the end may be most important.”
Courses of Interest:
- A colorectal or male pelvic cancer diagnosis has multiple systems that are affected by cancer treatment. The rehabilitation professional that works with the pelvic oncology patient needs to competently navigate treatment techniques for all of these systems, as well as be confident in treating a patient in a personal area. This two-day course will address specific cancer types including prostate cancer, penile cancer, and testicular cancer. Additional cancer types covered include colorectal cancer and anal cancer.
Trauma Awareness for the Pelvic Therapist - Remote Course - Apr 9-10, 2022
- Bring their increased awareness of trauma to the successful, holistic treatment of patients with pelvic pain, sexual dysfunction, bowel dysfunction, and bladder dysfunction.
Sexual Medicine in Pelvic Rehab - Remote Course - Apr 9-10, 2022
- This course provides a thorough introduction to pelvic floor sexual function, dysfunction and treatment interventions for males and females of all sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Male Pelvic Floor Function, Dysfunction, and Treatment - Satellite Lab Course - April 23-24 2022
- Discuss sexual anatomy and physiology, prostate issues, and look at the research describing models of intimacy and what worked for couples who did learn to renegotiate intimacy after prostate cancer. Participants will be able to describe the relationships between pelvic muscle function and men’s sexual health, including the evidence that demonstrates pelvic muscle rehabilitation's positive impact on erectile function.
1. Beck, A. M., Robinson, J. W., & Carlson, L. E. (2009, April). Sexual intimacy in heterosexual couples after prostate cancer treatment: What we know and what we still need to learn. In Urologic oncology: seminars and original investigations (Vol. 27, No. 2, pp. 137-143). Elsevier.
2. Gilbert, E., Ussher, J. M., & Perz, J. (2010). Renegotiating sexuality and intimacy in the context of cancer: the experiences of carers. Archives of Sexual Behavior, 39(4), 998-1009.
3. Hawkins, Y., Ussher, J., Gilbert, E., Perz, J., Sandoval, M., & Sundquist, K. (2009). Changes in sexuality and intimacy after the diagnosis and treatment of cancer: the experience of partners in a sexual relationship with a person with cancer. Cancer Nursing, 32(4), 271-280.
4. Higano, C. S. (2012). Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer. Journal of Clinical Oncology, 30(30), 3720-3725.
5. Ussher, J. M., Perz, J., Gilbert, E., Wong, W. T., & Hobbs, K. (2013). Renegotiating sex and intimacy after cancer: resisting the coital imperative. Cancer Nursing, 36(6), 454-462.
6. Weiner, L., Avery-Clark, C. (2017). Sensate Focus in Sex Therapy: The Illustrated Manual. Routledge, New York.
7. Wittmann, D., Carolan, M., Given, B., Skolarus, T. A., An, L., Palapattu, G., & Montie, J. E. (2014). Exploring the role of the partner in couples’ sexual recovery after surgery for prostate cancer. Supportive Care in Cancer, 22(9), 2509-2515.
The female sexual response cycle is more than physical stimulation. As pelvic therapists, we frequently find ourselves treating pelvic pain that has interrupted a woman’s ability to enjoy her sexuality and sensuality. As physical therapists, we focus on the physical limitations and pain generators as a way of helping patients overcome their functional limitations. However, many of us find that once many of the physical symptoms have cleared with pelvic floor and fascial stretching, our patients are still apprehensive to engage physically, or they are not able to derive pleasure. There is clearly a gap that needs to be bridged that goes beyond pain.
 Last year I taught my class, Lumbar Nerve Manual Assessment and Treatment. I was honored and astounded to have Dee Hartmann, PT in my class. For those of you who do not know Dee, she has been a champion of our field for a long time, and she has been instrumental in elevating physical therapy as a first line of treatment in pelvic pain through her work, international leadership, and representation in multiple organizations, including APTA SOWH, ISSVD, IPPS, NVA, ISSWSH, and as an editor for the Journal of Sexual Medicine.
Last year I taught my class, Lumbar Nerve Manual Assessment and Treatment. I was honored and astounded to have Dee Hartmann, PT in my class. For those of you who do not know Dee, she has been a champion of our field for a long time, and she has been instrumental in elevating physical therapy as a first line of treatment in pelvic pain through her work, international leadership, and representation in multiple organizations, including APTA SOWH, ISSVD, IPPS, NVA, ISSWSH, and as an editor for the Journal of Sexual Medicine.
In this manual nerve class, I was teaching how to treat the path of the genitofemoral nerve, which affects the peri-clitoral tissues and sensation. We also covered manual therapy approaches to decrease restriction in the clitoral complex and improve the blood flow response in this region. Dee was fascinated and looped me into what she had been working on for the past several years. She has been working as part of a company called Vulvalove with her partner, sex therapist, Elizabeth Wood on studying and teaching women how to recapture their sensuality. Immediately, we wanted to combine forces in some way to present a way to approach these issues. So, when Dee invited me to present with Elizabeth and her at the Combined Sections Meeting of the American Physical Therapy Association (CSM) this year, I was humbled and excited to jump on board.
With improved tissue mobility in the clitoral and vaginal area, blood flow is able to improve through any previously restricted tissues. With any manual therapy or soft tissue work, it is expected that cutaneous circulation of blood and lymph will alter. In studies, a measure of this blood flow, VPA (Vaginal Pulse Amplitude) is higher in the arousal than the non-arousal state in women.4 “The first measurable sign of sexual arousal is an increase in the blood flow. This creates the engorged condition, elevates the luminal oxygen tension and stimulates the production of surface vaginal fluid by increased plasma”.5 Manual therapy can likely affect this.1,2. During our CSM talk, I will discuss the neurovascular anatomy and will have a brief video of manual techniques to enhance these pathways in my portion of the presentation.
In the 19th century, female orgasm and sensuality was believed to be more vaginal, but as the 20th century unfolded, understanding of the clitoral tissues improved. More recent research reveals the origin of female pleasure is more complex, involving the clitoris, vulva, vagina, and uterus.3 However, female response is more complicated than just anatomy below the waist.
Heart Rate Variability (HRV) is a measure of autonomic nervous system health and the ability to flux between sympathetic and parasympathetic states. Autogenic training and meditation or mindfulness have been shown in multiple studies to improve HRV. A study by Stanton in 2017 demonstrated that even one session of autogenic training can increase HRV and VPA (Vaginal Pulse Amplitude, a measure of arousal). In our talk at CSM, Dee will cover the role of autogenics and how to specifically and practically use our autonomic state to influence our perception and feeling of pleasure. Dee will also cover extensive clitoral anatomy to have a better understanding of how this intricate complex functions and is structured in women.
Elizabeth Wood, a former sex therapist who is now a sex educator, will then present on the arousal cycle and what can be done physiologically to prepare the arousal network for climax. Elizabeth will help us to better define and understand the roles of arousal, calibration, and exploring sensuality, including exercises to help a patient have a more fulfilling experience once the physical pain is resolved. As Elizabeth says, “Knowledge is an antidote to shame and an invitation to pleasure”.
If you will be at CSM, please come join us at the opening session, Thursday February 13 from 8am-10am (PH2540), “Now That The Pain Is Gone, Where’s the Pleasure”.
If you can’t make it to CSM, I hope to see you at one of my nerve classes, “Lumbar Nerve Manual Therapy and Assessment” this year in Madison, WI April 24-26 or Seattle, WA October 16-18 to further explore manual therapies to improve sensation and neural feedback loops and to continue this conversation!
1. Portillo-Soto, A., Eberman, L. E., Demchak, T. J., & Peebles, C. (2014). Comparison of blood flow changes with soft tissue mobilization and massage therapy. The Journal of Alternative and Complementary Medicine, 20(12), 932-936.
2. Ramos-González, E., Moreno-Lorenzo, C., Matarán-Peñarrocha, G. A., Guisado-Barrilao, R., Aguilar-Ferrándiz, M. E., & Castro-Sánchez, A. M. (2012). Comparative study on the effectiveness of myofascial release manual therapy and physical therapy for venous insufficiency in postmenopausal women. Complementary therapies in medicine, 20(5), 291-298.
3. Colson, M. H. (2010). Female orgasm: Myths, facts and controversies. Sexologies, 19(1), 8-14.
4. Rogers, G. S., Van de Castle, R. L., Evans, W. S., & Critelli, J. W. (1985). Vaginal pulse amplitude response patterns during erotic conditions and sleep. Archives of sexual behavior, 14(4), 327-342.
5. Stanton, A., & Meston, C. (2017). A single session of autogenic training increases acute subjective and physiological sexual arousal in sexually functional women. Journal of sex & marital therapy, 43(7), 601-617.
Mia Fine, MS, LMFT, CST joins the Herman & Wallace faculty in 2020 with her new course on Sexual Interviewing for Pelvic Health Therapists! The new course is launching this April 4-5, 2020 in Seattle, WA; Lecture topics include bio-psycho-social-spiritual interviewing skills, maintaining a patient-centered approach to taking a sexual history, and awareness of potential provider biases that could compromise treatment. Labs will take the form of experiential practice with Bio-Psycho-Social-Spiritual-Sexual Interviewing Skills, case studies and role playing. Check out Mia's interview with The Pelvic Rehab Report, then join her for Sexual Interviewing for Pelvic Health Therapists!
 Tell us about yourself, Mia!
Tell us about yourself, Mia!
My name is Mia Fine, MS, LMFT, CST and I’ve been a Licensed Marriage and Family therapist for four years. I am an AASECT Certified Sex Therapist and my private practice is Mia Fine Therapy, PLLC. I see these kinds of patients: folks with Erectile Dysfunction, Pre-mature Ejaculation, Vaginismus, Dyspareunia, Desire Discrepancy, LGBTQ+, Ethical Non-monogamy, Anxiety, Depression, Trauma, Relational Concerns, Improving Communication.
What can you tell us about the new course?
This course will offer a great deal of current and empirically-founded sex therapy and sex education resources for both the provider as well as the patient. This course will add the extensive skills of interviewing for sexual health. It also offers the provider a new awareness and self-knowledge on his/her/their own blind spots and biases.
How will skills learned at this course allow practitioners to see patients differently?
Human beings are hardwired for connection, intimacy, and pleasure. Our society often tells us that there is something wrong with us, or that we are defective, for wanting a healthy sex life and for addressing our human needs/sexual desires. This course will broaden the provider’s scope of competence in working with patients who experience forms of sexual dysfunction and who hope to live their full sexual lives.
What inspired you to create this course?
This course was inspired by the need for providers who work with pelvic floor concerns to be trained in addressing and discussing sexual health with their patients.
What resources were essential in creating your course?
Becoming a Licensed Marriage and Family Therapist and a Certified Medical Family Therapist requires three years of intensive graduate school. Additionally, a minimum of two years of training to become an AASECT Certified Sex Therapist and hundreds of hours of direct client contact hours, supervision, and consultation. I attend numerous sex therapy trainings and continuing education opportunities on a regular and ongoing basis. I also train incoming sex therapists on current modalities and working with vulnerable client populations.
How do you think these skills will benefit a clinician in their practice?
It is vital that providers working with pelvic floor concerns have the necessary education and training to work with patients on issues of sexual dysfunction. It is also important that providers be aware of their own biases and be introduced to the various sexual health resources available to providers and patients.
What is one important technique taught in your course that everybody should learn?
Role playing sexual health interview questions is an important experience in feeling the discomfort that many providers feel when asking sexual health questions. This offers insight not only into the provider experience but also the patient’s experience of uncomfortability. Role playing this dynamic illustrates the very real experiences that show up in the therapeutic context.
Sexuality is core to most human beings’ identity and daily experiences. When there are concerns relating to our sexual identity, sexual health, and capacity to access our full potential, it affects our quality of life as well as our holistic well-being. Working with folks on issues of sexual health and decreasing sexual dysfunction encourages awareness and encourages healing. Imagining a world where human beings don’t walk around holding shame or traumatic pain is imaging a world of health and happiness.
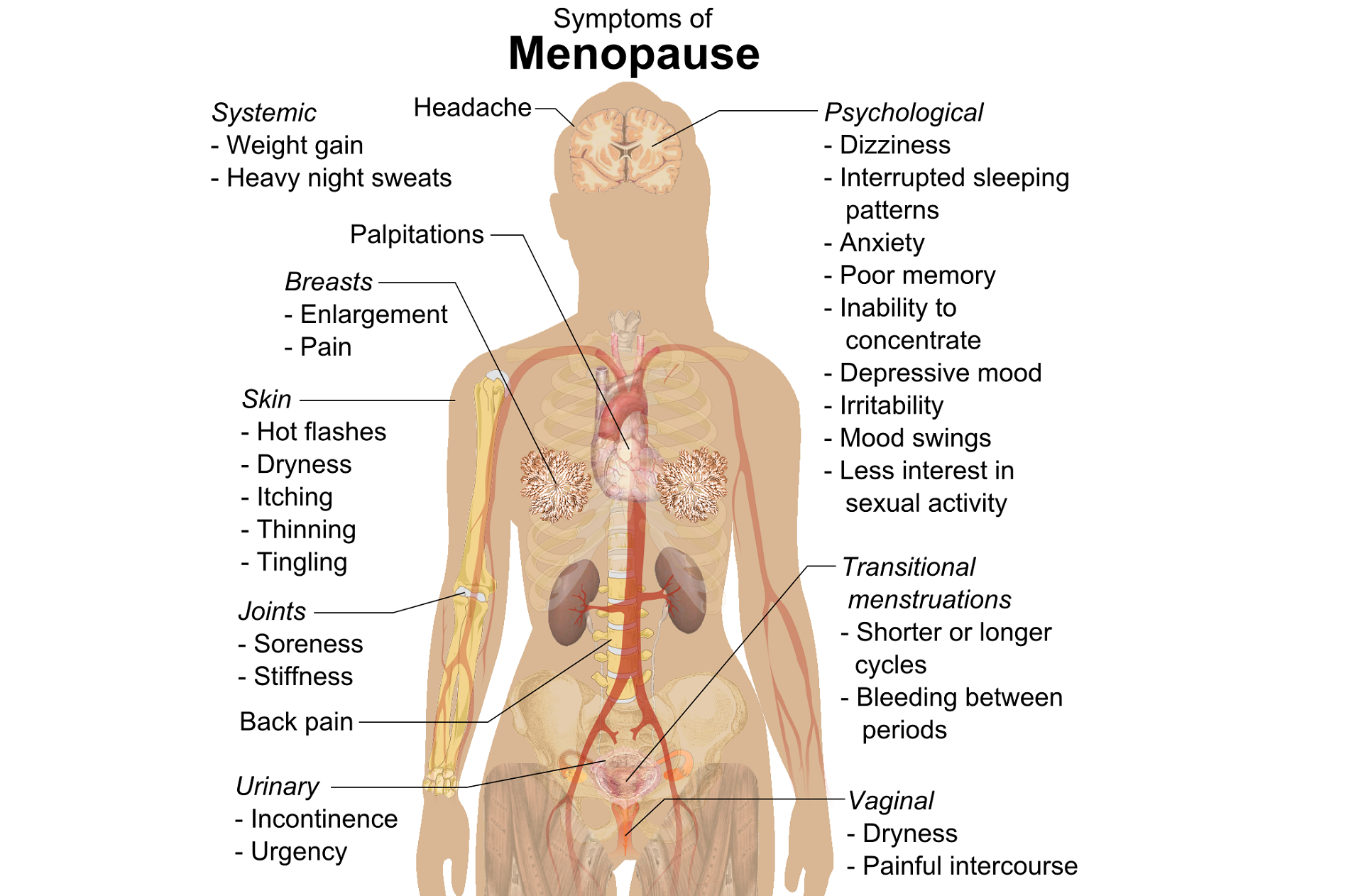
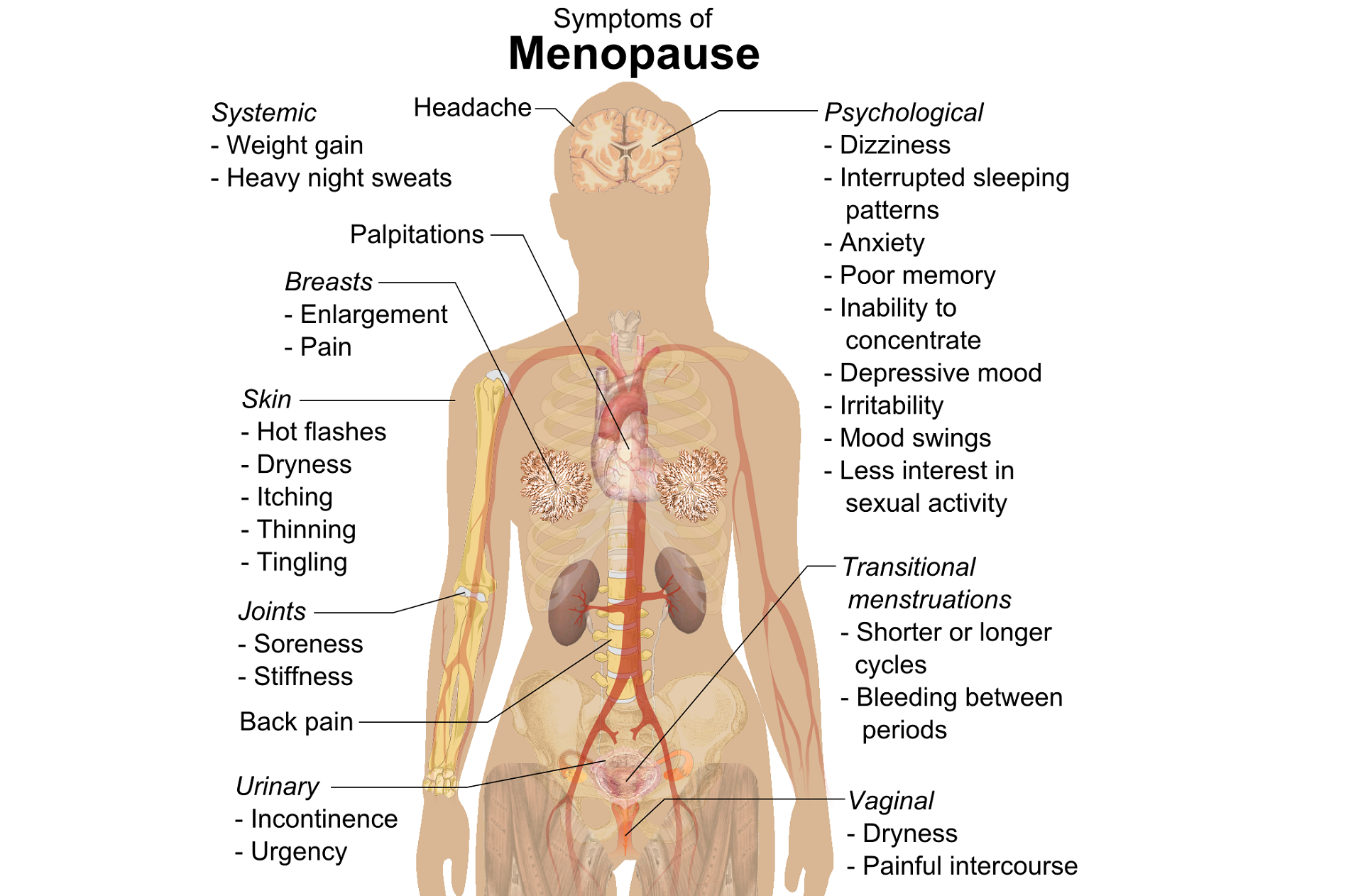
A question that often comes up in conversation around menopause is that of pelvic health – the effects on bladder, bowel or sexual health…what works, what’s safe, what’s not? Is hormone therapy better, worse or the same in terms of efficacy when compared to pelvic rehab? Do we have a role here?
An awareness of pelvic health issues that arise at menopause was explored in Oskay’s 2005 paper ‘A study on urogenital complaints of postmenopausal women aged 50 and over’ stating ‘…Urinary incontinence and sexual problems, particularly decline in sexual desire, are widespread among postmenopausal women. Frequent urinary tract infections, obesity, chronic constipation and other chronic illnesses seem to be the predictors of UI.’
 Moller’s 2006 paper explored the link between LUTS (Lower Urinary Tract Symptoms) and sexual activity at midlife: the paper discussed how lower urinary tract symptoms (LUTS) have a profound impact on women’s physical, social, and sexual well being, and confirmed that LUTS are likely to affect sexual activity. However, they also found that conversely, sexual activity may affect the occurrence of LUTS – in their study a questionnaire was sent to 4,000 unselected women aged 40–60 years, and they found that compared to women having sexual relationship, a statistically significant 3 to 6 fold higher prevalence of LUTS was observed in women with no sexual relationship. They also found that women who ceased sexual relationship an increase in the de novo occurrence of most LUTS was observed, concluding that ‘…sexual inactivity may lead to LUTS and vice versa’.
Moller’s 2006 paper explored the link between LUTS (Lower Urinary Tract Symptoms) and sexual activity at midlife: the paper discussed how lower urinary tract symptoms (LUTS) have a profound impact on women’s physical, social, and sexual well being, and confirmed that LUTS are likely to affect sexual activity. However, they also found that conversely, sexual activity may affect the occurrence of LUTS – in their study a questionnaire was sent to 4,000 unselected women aged 40–60 years, and they found that compared to women having sexual relationship, a statistically significant 3 to 6 fold higher prevalence of LUTS was observed in women with no sexual relationship. They also found that women who ceased sexual relationship an increase in the de novo occurrence of most LUTS was observed, concluding that ‘…sexual inactivity may lead to LUTS and vice versa’.
So, who advises women going through menopause about issues such as sexual ergonomics, the use of lubricants or moisturisers, or provide a discussion about the benefits of local topical estrogen? As well as providing a skillset that includes orthopaedic assessment to rule out any musculo-skeletal influences that could be a driver for sexual dysfunction? That would be the pelvic rehab specialist clinician! Tosun et al asked the question ‘Do stages of menopause affect the outcomes of pelvic floor muscle training?’ and the answer in this and other papers was yes; with the research comparing pelvic rehab vs hormone therapy vs a combination approach of pelvic rehab and topical estrogen providing the best outcomes. Nygaard’s paper looked at the ‘Impact of menopausal status on the outcome of pelvic floor physiotherapy in women with urinary incontinence’ and concluded that : ‘…(both pre and postmenopausal women) benefit from motor learning strategies and adopt functional training to improve their urinary symptoms in similar ways, irrespective of hormonal status or HRT and BMI category’.
We must also factor in some of the other health concerns that pelvic health can impact at midlife for women – Brown et al asked the question ‘Urinary incontinence: does it increase risk for falls and fractures?’ They answered their question by concluding that ‘‘… urge incontinence was associated independently with an increased risk of falls and non-spine, nontraumatic fractures in older women. Urinary frequency, nocturia, and rushing to the bathroom to avoid urge incontinent episodes most likely increase the risk of falling, which then results in fractures. Early diagnosis and appropriate treatment of urge incontinence may decrease the risk of fracture.’
If you are interested in learning more about pelvic health, sexual function and bone health at Menopause, consider attending Menopause Rehabilitation and Symptom Management.
Sexual activity and lower urinary tract symptoms’ Møller LA1, Lose G. Int Urogynecol J Pelvic Floor Dysfunct. 2006 Jan;17(1):18-21. Epub 2005 Jul 29.
A study on urogenital complaints of postmenopausal women aged 50 and over. Oskay UY1, Beji NK, Yalcin O. Acta Obstet Gynecol Scand. 2005 Jan;84(1):72-8.
Do stages of menopause affect the outcomes of pelvic floor muscle training? Tosun ÖÇ1, Mutlu EK, Tosun G, Ergenoğlu AM, Yeniel AÖ, Malkoç M, Aşkar N, İtil İM. Menopause. 2015 Feb;22(2):175-84. doi: 10.1097/GME.0000000000000278.
‘Impact of menopausal status on the outcome of pelvic floor physiotherapy in women with urinary incontinence.’ Nygaard CC1, Betschart C, Hafez AA, Lewis E, Chasiotis I, Doumouchtsis SK. Int Urogynecol J. 2013 Dec;24(12):2071-6. doi: 10.1007/s00192-013-2179-7. Epub 2013 Jul 17
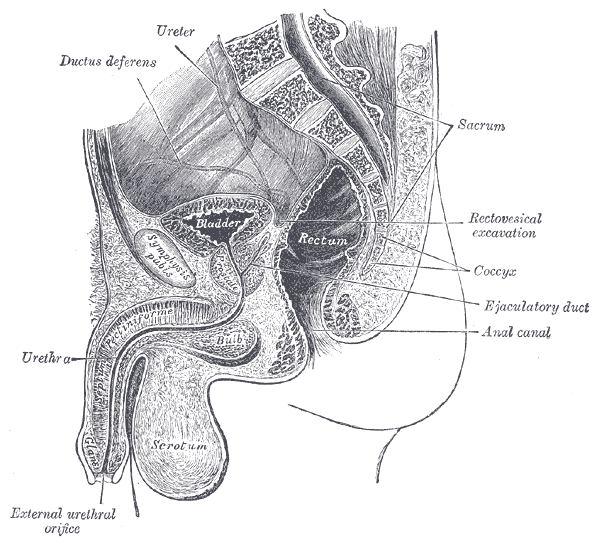
Erectile dysfunction (ED) is a debilitation complication of radical prostatectomy, which is a treatment for prostate cancer. ED is caused by a variety of causes, diabetic vasculopathy, smoking, high blood pressure, high cholesterol, psychological issues, peripheral vascular disease and medication; we will focus on post-prostatectomy ED and the role of penile rehabilitation in its management.
Post-prostatectomy-related Erectile dysfunction
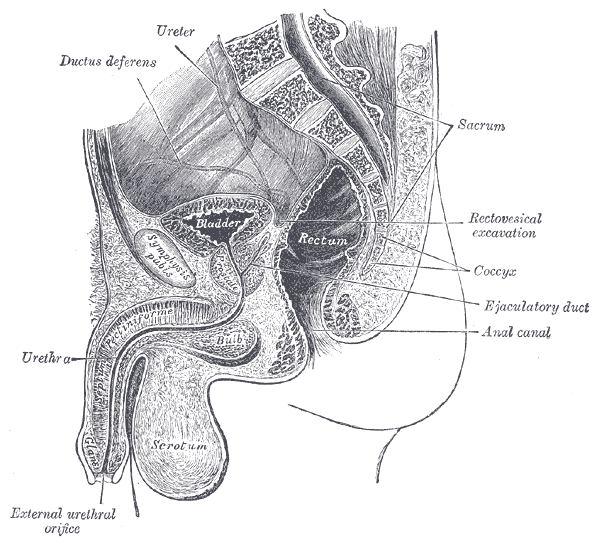 Radical prostatectomy can result in nerve injury to the penis. Moreover, significant fibrotic changes take place in the corpus cavernosum of the penis postoperatively. It takes approximately 1-2 years for erectile function to return after radical prostatectomy. This is a period of “neuropraxia,” during which there is transient cavernosal nerve dysfunction. However, a prolonged “flaccid state” might lead to irreversible damage to the cavernous tissue 1.
Radical prostatectomy can result in nerve injury to the penis. Moreover, significant fibrotic changes take place in the corpus cavernosum of the penis postoperatively. It takes approximately 1-2 years for erectile function to return after radical prostatectomy. This is a period of “neuropraxia,” during which there is transient cavernosal nerve dysfunction. However, a prolonged “flaccid state” might lead to irreversible damage to the cavernous tissue 1.
Research on penile hemodynamics in these patients have shown that venous leakage is also implicated in its pathophysiology. An injury to the neurovascular bundles likely leads to smooth muscle cell death, which then leads to irreversible veno-occlusive disease.
There is a potential role of hypoxia in stimulating growth factors (TGF-beta) that stimulate collagen synthesis in cavernosal smooth muscle. Prostaglandin E1 (PGE1) was found to suppress the effect of TGF-β1 on collagen synthesis.
Role of Penile Rehabilitation
The goal of Penile Rehabilitation is to limit and reverse ED in post-prostatectomy patients. The idea is to minimize fibrotic changes during the period of “penile quiescence” after nerve-sparing radical prostatectomy. Several approaches have been tried, including PGE1 injection, vacuum devices, and phosphodiesterase type 5 (PDE-5) inhibitors.
Mulhall and coworkers followed 132 patients through an 18-month period after they were placed in “rehabilitation” or “no rehabilitation” groups after radical prostatectomy, and 52% of those undergoing rehabilitation (sildenafil + alprostadil) reported spontaneous functional erections, compared with 19% of the men in the no-rehabilitation group 2.
Prostaglandin E1 (PGE1)
Alprostadil is a vasodilatory prostaglandin E1 that can be injected into the penis or placement in the urethra in order to treat ED. Montorsi, et al. studied the use of intracorporeal injections of alprostadil starting at 1 month after bilateral nerve-sparing radical prostatectomy and reported a higher rate of spontaneous erections after 6 months compared with no treatment 3. Gontero, et al. investigated alprostadil injections at various time points after non–nerve-sparing radical prostatectomy and found that 70% of patients receiving injections within the first 3 months were able to achieve erections sufficient for intercourse, compared with 40% of patients receiving injections after the first 3 months 4.
Vacuum constriction device (VCD)
VCD is an external pump that is used to get and maintain an erection. Raina, et al evaluated the daily use of a VCD beginning within two months after radical prostatectomy, and reported that after 9 months of treatment, 17% of patients using the device had return of natural erections sufficient for intercourse, compared with 11% of patients in the nontreatment group 4.
PDE-5 Inhibitors
PDE-5 inhibitors (such as Sildenafil) are the first-line treatment for ED of many etiologies. Several studies have shown that the use of PDE-5 inhibitors might lead to an overall improvement in endothelial cell function in the corpus cavernosum. Chronic use of oral PDE-5 inhibitors suggest a beneficial effect on endothelial cell function. Desouza, et al. concluded that daily sildenafil improves overall vascular endothelial cell function. However, Zagaja, et al. found that men taking oral sildenafil within the first 9 months of a nerve-sparing procedure did not have any erectogenic response 4.
Overall, accumulating scientific literature is suggesting that penile rehabilitation therapies have a positive impact on the sexual function outcome in post-prostatectomy patients. It must be noted that these methods do not cure ED and should be used with caution.
1Penson DF, McLerran D, Feng Z, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005;173:1701-1705.
2Mulhall J, Land S, Parker M, et al. The use of an erectogenic pharmacotherapy regimen following radical prostatectomy improves recovery of spontaneous erectile function. J Sex Med. 2005; 2:532-540.
3Montorsi F, Guazzoni G, Strambi LF, et al. Recovery of spontaneous erectile function after nerve-sparing radical retropubic prostatectomy with and without early intracavernous injections of alprostadil: results of a prospective, randomised trial. J Urol. 1997;158:1408-1410.
4Gontero P, Fontana F, Bagnasacco A, et al. Is there an optimal time for intracavernous prostaglandin E1 rehabilitation following non- nerve sparing radical prostatectomy? Results from a hemodynamic prospective study. J Urol. 2003;169:2166-2169.
In a previous post on The Pelvic Rehab Report Sagira Vora, PT, MPT, WCS, PRPC told us how "women with sexually adverse experiences tend to have impaired genital response when in consensual sexual situations, however, women who do not have sexual abuse histories and but have sexual pain tend to have appropriate genital response." Today Sagira helps us understand how the pelvic floor responds to consensual sexual activity in women with a history of sexual trauma.
Today we try to look for answers for questions that came up during the last blogs.
 How does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past?
How does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past?
To answer these questions, it’s important to understand two facts about the pelvic floor. 1) the pelvic floor plays a role in emotional processing1, and 2) muscle activity in all muscles, including the pelvic floor, increases with exposure to stress and during anxiety evoking experiences2.
We explored in the last blog that women with sexual abuse histories responded with increased pelvic floor overactivity when watching movie clips with sexually threatening and consensual sexual content. Apparently, for women with sexual abuse history even consensual sexual situations can be experienced as threatening1.
Lehrer et. al. found overactivity in the neuronal and hormonal circuits that increase sexual arousal and activity. These circuits are already overactive in individuals who have Post Traumatic Stress Disorder (PTSD), and increased activity can increase anxiety, fear and other symptoms of PTSD instead of normal sexual arousal and excitement during a sexual experience2. For the woman with PTSD this means that sexual arousal signals impending threat rather than pleasure1. And as we already learned in previous blogs and above that when humans feel threatened they respond by tightening muscles and most notably the pelvic floor muscle.
Significant co-relation is found between sexual abuse, subsequent PTSD and chronic pelvic pain3. Hooker et. al, found irritable bowel syndrome, pelvic pain, and physical and sexual abuse to be the most commonly diagnosed together4. More importantly, when patients were successfully treated for PTSD they continued to be 2.7 times more likely to have pelvic floor dysfunction and 2.4 times more likely to have sexual dysfunction. This builds the case for interventions that are multidisciplinary to help patients of abuse and sexual assault, with the pelvic floor therapist playing a significant role.
In the next blog, lets explore how the pelvic floor therapist can work with a counselor and a sex therapist to help the woman with sexual pain dysfunction.
Anna Padoa and Talli Rosenbaum. The overactive pelvic floor. Springer. 1st ed. 2016
Yehuda R, Lehrner A, Rosenbaum TY. PTSD and sexual dysfunction in men and women. J Sex Med. 2015:12(5):1107-19
Blok BF. Holstege G. The neuronal control of micturition and its relation to the emotional motor system. Prog Brain Res. 1996; 107:113-26
Para ML, Chen LP, Goranson EN, Sattler AL, Colbenson KM, Seime RJ, Et. al. Sexual abuse and lifetime diagnoses of somatic disorders. JAMA. 2013; 302:550-61
Hooker AB, van Moorst BR, van Haarst EP, Van Ootegehem NAM, van Dijken DKE, Heres MHB, Chronic pelvic pain: evaluation of the epidemiology, baseline characteristics, and clinical variables via a prospective and multidisciplinary approach. Clin Exp Obstet Gynecol. 2013; 40:492-8
In a previous post on The Pelvic Rehab Report Sagira Vora, PT, MPT, WCS, PRPC shared that "cognitive-behavioral therapy appears to play a significant role in improving sexual function in women". Today, in part three of her ongoing series on sex and pelvic health, Sagira explores how sexual pain affects sexual dysfunction in women.
 After having explored what allows for women to have pleasurable sexual experiences including pain-free sex and mind-blowing orgasms, we now turn towards our cohort that have pain with sex and intimacy. How does this group differ from women who do not have pain with sex? Are there some common factors with this group of women, and perhaps understanding these factors may help the pelvic floor therapist render more effective and successful treatment?
After having explored what allows for women to have pleasurable sexual experiences including pain-free sex and mind-blowing orgasms, we now turn towards our cohort that have pain with sex and intimacy. How does this group differ from women who do not have pain with sex? Are there some common factors with this group of women, and perhaps understanding these factors may help the pelvic floor therapist render more effective and successful treatment?
There are few studies exploring sexual arousal in women with sexual pain disorders. However, their findings are remarkable. Brauer and colleagues found that genital response, as measured by vaginal photoplethysmography and subjective reports, was found to be equal in women with sexual pain vs. women who did not have pain, when they were shown oral sex and intercourse movie clips. This and other studies have shown that genital response in women with dyspareunia is not impaired. Genital response in women with dyspareunia is however, effected by fear of pain. When Brauer and colleagues subjected women with dyspareunia to threat of electrical shock (not actual shock) while watching an erotic movie clip they found that women with dyspareunia had much diminished sexual response including diminished genital arousal. But Spano and Lamont found that genital response was diminished by fear of pain equally in women with sexual pain and women without sexual pain.
Fear of pain also resulted in increased muscle activity in the pelvic floor. However, this increase was noted in women with pain and women without sexual pain equally and was noted with exposure to sexually threatening film clips as well as threatening film clips without sexual content. The conclusion, then, from these results is that the pelvic floor plays a role in emotional processing and tightening, or overactivity is a protective response noted in all women regardless of sexual pain history.
The one difference that was noted was with women who had the experience of sexual abuse. For them, pelvic floor overactivity was noted when watching sexually threatening as well consensual sexual content. Women without sexual abuse history did not have increased pelvic floor activity when watching consensual sexual content.
In summary, evidence supports the hypothesis that women with sexually adverse experiences tend to have impaired genital response when in consensual sexual situations, however, women who do not have sexual abuse histories and but have sexual pain tend to have appropriate genital response. Both groups, however, have increased pelvic floor muscle activity in consensual sexual situations. This increase in pelvic floor muscle activity leads to muscle pain, reduced blood flow, reduced lubrication, increased friction between penis and vulvar skin and hence leads to pain.
This brings us to our next questions, how does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past? Please tune in to the next blog for answers…
Blok BF, Holstege G. The neuronal control of micturition and its relation to the emotional motor system. Prog Brain Res. 1996; 107:113-26
Brauer M, Laan E, ter Kuile MM. Sexual arousal in women with superficial dyspareunia. Arch Sex Behav. 2006; 35:191-200
Brauer M, ter Kuile MM, Janssen S, Lann E. The effect of pain-related fear on sexual arousal in women with superficial dyspareunia. Eur J Pain: 2007; 11:788-98
Spano L, Lamont JA. Dyspareunia: a symptom of female sexual dysfunction. Can Nurse 1975;71:22-5
It’s St Valentine’s day this week – you may have noticed hearts and flowers everywhere you look and a general theme of love and romance. For many women going through cancer treatment, sex may be the last thing on their mind…or not! Women who are going through treatment for gynecologic cancer are often handed a set of dilators with minimal instruction on how to use them, or as one patient reported, they are told to have sex three or four times a week during radiation therapy ‘to keep your vagina patent’. As a pelvic rehab practitioner with a special interest in oncology rehab, I know that we can (we must!) do better, in helping women live well after cancer treatment ends.
 As Susan Gubar, an ovarian cancer survivor, writes in the New York Times ‘…It can be difficult to experience desire if you don’t love but fear your body or if you cannot recognize it as your own. Surgical scars, lost body parts and hair, chemically induced fatigue, radiological burns, nausea, hormone-blocking medications, numbness from neuropathies, weight gain or loss, and anxiety hardly function as aphrodisiacs…’
As Susan Gubar, an ovarian cancer survivor, writes in the New York Times ‘…It can be difficult to experience desire if you don’t love but fear your body or if you cannot recognize it as your own. Surgical scars, lost body parts and hair, chemically induced fatigue, radiological burns, nausea, hormone-blocking medications, numbness from neuropathies, weight gain or loss, and anxiety hardly function as aphrodisiacs…’
Although sexual changes can be categorised into physical, psychological and social, the categories cannot be neatly delineated in the lived experience (Malone at al 2017). The good news? Pelvic rehab therapists not only have the skills to enhance pelvic health after cancer treatment and are ideally positioned to be able to take a global and local approach to the sexual health difficulties women may face after cancer treatment ends, but there is also a good and growing body of evidence to support the work we do. Factors to consider include physical issues leading to dyspareunia, including musculo-skeletal/ orthopaedic, Psychological issues, including loss of libido and other pelvic health issues impacting sexual function such as faecal/ urinary incontinence, pain or fatigue.
In Hazewinkel’s 2010 paper, women reported that they thought their physicians would tell them if solutions were available…most reported reasons for not seeking help were that women found their symptoms bearable in the light of their cancer diagnosis and lacked knowledge about possible treatments but when informed of possible treatment strategies ‘…women stated that care should be improved, specifically by timely referral to pelvic floor specialists’. The good news: ‘‘Pelvic Floor Rehab Physiotherapy is effective even in gynecological cancer survivors who need it most.’ (Yang 2012)
The issue therefore may be one of awareness – for both the women who need our services and the physicians and healthcare team who work in the field of gynecologic oncology. What we need is acknowledgement of the issues and confident conversation and assessment by clinicians – interested in learning more? Come and join the conversation in Tampa next month at my Oncology & the Female Pelvic Floor course!
‘Sex after Cancer’ by Susan Gubar, https://www.nytimes.com/2018/01/18/well/live/sex-after-cancer.html
Malone et al 2017: ‘‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’
Hazewinkel et al 2010 ‘Reasons for not seeking medical help for severe pelvic floor symptoms: a qualitative study in survivors of gynaecological cancer’
I work at University of Chicago and we are in the throes of preparing for a (big T) Trauma Center. But I am physical therapist who works with (little t) traumatized patients- as I treat only pelvic or oncology patients (and usually both).
From the online dictionary: Trauma is 1. A deeply distressing or disturbing experience (little t trauma) or 2. Physical injury (injury, damage, wound) yes- big T Trauma. In my experience, the Trauma creates the trauma and the body responds in characteristically uncharacteristic ways (more on this later).
 People in distress/trauma-affected do not respond rationally or characteristically, so I have learned to respond to distress/trauma in a rational, ethical, legal and caring manner. Always. Every time. To the best of my ability, and without shame or blame.
People in distress/trauma-affected do not respond rationally or characteristically, so I have learned to respond to distress/trauma in a rational, ethical, legal and caring manner. Always. Every time. To the best of my ability, and without shame or blame.
Let’s talk briefly about Trauma Informed Approach
This is a (person), program, institution or system that:
- Realizes the widespread impact of trauma and understands potential paths for recovery
- Recognizes the signs and symptoms of trauma in clients, families, staff and others affected
- Responds by fully integrating knowledge about trauma into policies, procedures and practices
- Seeks to actively resist retraumatization
The Tenets of Trauma Informed Approach
- Safety
- Trustworthiness and transparency
- Peer support
- Collaboration and mutuality
- Empowerment, voice and choice
- Cultural, historical and gender issues
Trauma Specific Interventions
- Survivors need to be respected, informed, supported, connected, and hopeful- in their recovery
- Interrelation between trauma and symptoms of trauma such as substance abuse, eating disorders, depression, anxiety, musculoskeletal presentation, and acute crisis- including suicidal/homicidal ideations (coordination with other service providers)
- Work in a collaborative way with survivors, families and friends of survivor, and other service providers in a way that will empower survivors
Types of trauma are varied but I usually treat survivors of emotional, verbal, sexual and medical trauma. I have even treated patients who felt traumatized by other pelvic floor physical therapists (again, no judgement). Since most of my clinical experience include sexual and medical trauma survivorship, I try to reframe these experiences as potential Post Traumatic Growth, especially when working with my oncology patients. For my pelvic patients who divulge sexual trauma, I don’t dictate or name anything. I allow the survivor to make the rules and definitions. Survivors of sexual trauma need extra care when treating pelvic floor dysfunction.
First, when treating survivors of sexual trauma: expect ‘characteristically uncharacteristic’ events to occur. These include the psychological/somatic effects of passing out, flashbacks, seizures, tremors, dissociation and other mechanisms of coping with the trauma. Have a plan ready for these patients.
Triaging the survivor to assess their needs, when trauma has been verbalized/disclosed:
- Are you safe right now?
- Do you need medical treatment right now?
- What do you need to feel in control of (PT session/immediately after disclosure of trauma)?
- You have choices in your treatment and in your response to trauma.
- I believe you.
- Lastly, is this a situation for mandated reporting?
After assisting the survivor in their journey towards healing, it is imperative that you take care of yourself. Making healthy boundaries (with patients and others), taking time to decompress, creating healthy ritualistic behaviors, mindfulness/relaxation and somatic release (like yoga, massage or working out) is crucial to successfully treating patients who have experienced trauma and who have shared that trauma experience with you.
Because I use gentle yoga for both my trauma survivors’ treatment and for my own self-care, my new course implements evidenced based trauma sensitive yoga. Additionally, modifications for manual therapy are explored. The class is designed to be informative and experiential while integrating the Trauma Informed Approaches of Safety, Trustworthiness and transparency, Peer support, Collaboration and mutuality, Empowerment, voice and choice and Cultural, historical and gender issues.
Join me in Trauma Awareness for the Pelvic Therapist, next available this March in Albany, NY.