My name is Tina Allen. I teach a course called Manual Therapy Techniques for the Pelvic Rehab Therapist. I developed this course in 2016 out of desire to help clinicians feel comfortable in their palpation and hands on skills.
 My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
My journey as a pelvic rehab therapist started with a patient whispering to me in the middle of a busy sports/ortho clinic gym; “is it normal to leak when you laugh”. I was treating her after her total hip replacement and my first question was “where are you leaking”? I was concerned that her incision was leaking, that she had an infection and it was beyond me to understand why it would happen when she laughed! I was 24 years old and 2 years out of PT school. Little did I know, that one whispered question would lead me to where I am today. I am in my 25th year as a PT and 20th year specializing in pelvic rehabilitation.
When I started out there just were not many classes. I spent time learning from physicians, reading anything I could find and applying ‘general ‘orthopedic principles to the pelvis. I traveled to clinics and learned from other clinicians. I soaked up anything I could and brought it back to my clinical practice. When Holly Herman and Kathe Wallace asked me to teach with them I was humbled, honored and terribly nervous. Holly and Kathe where two of my greatest resources and to be able to teach along side them to help others along was humbling. As I prepared to teach I realized the breadth of what we do as pelvic rehab clinicians has grown exponentially since I started out.
Over the past 10 years of teaching the pelvic series with H&W; I noticed that for some of the participants there was a gap in confidence in palpation skills and in treatment techniques applied to the pelvic floor region. For most, it’s confidence in what they are feeling and where they are. This course came out of wanting to fill that gap. I wanted to allow a space that clinicians could come and spend two days learning, affirming and building confidence in their hands. They could then take those skills and confidence back to their clinics and help more patients.
The thought of writing this course was daunting. First off, written words are not my thing. Don’t get me wrong I love to read but me coming up with what to put on paper, much less a power point slide, frightened me. With much encouragement and support from colleagues and H&W, I got to work. The first thing was to think about what techniques to include. At some point after 20 years in the field, your hands just do the work and you don’t think about how you do something. My colleague and dear friend Katy Rice allowed me to sit down with her, practice a technique and then write down each specific step to do the skill. She would read them over and then attempt to do the technique by following only the written instructions. I also had patients who were instrumental in helping me choose what techniques to include. They would say to me “that is what made all the difference for me; it has to be included in what you teach others. “
I would think about who taught me each technique, whether it was a course, another clinician or a patient. I know that I did not make any of these up myself; while I may have modified a technique to work with my hands I did not originate them. Holly Tanner was so kind to brain storm with me and lead me to references for some of the techniques that we as clinicians use every day and that I was planning to include.
What happened next was months of me sitting at the kitchen table combing through books, articles, course manuals and online videos looking for origins of the techniques I use every day in my clinical practice. I wanted to be sure to give credit to sources. It was tedious but also inspiring to realize that some of these techniques have been around and documented since 1956 (Dicke, E., & Bischof-Seeberger, I.) and also that the same techniques are sited by multiple different sources. After about 6 months of our kitchen table not being suitable for dinner it was time to see what I had gathered and how it would all fit together. The result was this 2 day course: Manual Therapy Techniques for the Pelvic Rehab Therapist which has seven labs including internal, external and combination techniques, home program/self care ideas and time for brainstorming treatment progressions. Join me in Philadelphia, PA this October 20 - 21 to learn these essential skills.
Nutrition Perspectives for the Pelvic Rehab Therapist
There are moments when I pause and realize how far we’ve come in a short period of time, and then others when I’m acutely reminded how far we have yet to go. Our destination is an integrative health care system which addresses nourishment first and early versus last, not at all, or only when all else fails. My mission is to support the concept of nourishment first and early though sharing of “Nutrition Perspectives for the Pelvic Rehab Therapist” through the Herman & Wallace Pelvic Rehab Institute.
 After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After each weekend I teach Nutrition Perspectives for the Pelvic Rehab Therapist, I feel affirmed that this class, this information is vital and at times life-changing for practicing clinicians. And every time I teach, participants share that they take away much more than they expected. It’s a course that makes accessible complex concepts to entry level participants while offering timely and cutting edge integrative instruction to the advanced clinician eager to incorporate this knowledge into their practice. Supportive literature is woven throughout the tapestry of the course.
After the most recent live course event, a participant shared with me a letter she received from a patient in 2016 who mentions the lack of nutritional attention during her cancer treatment. I want to share with you the essence of this letter:
“In October 2015, I was diagnosed with cancer. The following December I started treatments of radiation and chemotherapy. I really appreciate all the fine employees who helped me through care and treatments. Every clinician I came across, whether a doctor, nurse, phlebotomist, radiation and chemo teams, and my PT, were all exceptional in showing care, concern and knowledge.
However, one area I felt was lacking in was nutrition. I was frequently offered a standard hospital-issue protein drink. When offered, I explained that I would not take it due to it containing high fructose corn syrup (HFCS). I asked if they knew that HFCS was like putting and accelerant on a fire? I received a smile and a nod of head as to say they understood.
I was also offered soda pop to wash down bad tasting medicines/ liquids I was to take. I opted to just down the medication without chasing it as I didn’t want to exacerbate my condition. While taking chemotherapy, I was offered snacks containing HFCS and other non-nutritive so-called foods.
I was also offered limited entree choices, but there were plenty of pies, cakes, jellies, and other non-nutritive foods to choose from. All Items I would not consider for a cancer diet or even a healthy diet. I finally took a picture of the menu selection sheet as I thought no one would believe such a thing could happen.
I received excellent care throughout your system with the exception of nutrition . I would ask that you take a look at making menus with truly healthy options as well as giving patients options that do not contain ingredients that feed the cancer.”
While this letter addresses an inpatient issue at one regional health system, it correspondingly brings into focus the irony present in the vast majority of health care settings across the nation from inpatient to outpatient settings: there is a profound lack of clarity about what it means to be nourished, especially when we are at our most vulnerable.
I cannot claim “Nutrition Perspectives” will solve our nation-wide problem, however, I am certainly encouraging a movement towards a collective understanding of the imperative fact that food is medicine - powerful medicine - and we must as front-line practitioners harness what this understanding can offer. Pelvic rehab practitioners are uniquely positioned to process this information and begin immediately sharing it in clinical practice.
Like many providers, this same participant shared with me that upon receipt of this letter two years ago, she struggled to make progress with what and how to offer nutritional information - mainly because of the overwhelming nature of the subject, and also because of the conflicting and oftentimes confusing information traditionally shared with the public. After attending Nutrition Perspectives, she said “I cannot even begin to describe how much your course has met ALL my hopes for helping clients!….I had struggled to put something together and here it all is - so unbelievably grateful.”
And that’s what this course is all about - empowering you as you broaden your scope of knowledge in a way that teaches you not facts, but deep understanding. Once that foundational understanding is laid, this grass-roots effort will progress like putting an accelerant on the integrative movement. Soon we’ll see the inclusion of nourishment information as first-line practice, and the lives impacted in a positive way will continue to grow.
Please join me at the next opportunity to share in this live experience with other like-minded clinicians. Nutrition Perspectives for the Pelvic Rehab Therapist will be coming to Denver, CO September 15 & 16, 2018!
Tamara Rial, PhD, CSPS, co-founder and developer of Low Pressure Fitness will be presenting the first edition of “Low Pressure Fitness and abdominal massage for pelvic care” in Princeton, New Jersey in July, 2018. Tamara is internationally recognized for her work with hypopressive exercise and Low Pressure Fitness. In this article she presents the novel topic of hypopressives as a complementary pelvic floor muscle training tool for incontinence after prostate cancer surgery.
Urinary Incontinence is the most common side effect men suffer after prostate cancer surgery along with erectile dysfunction. Although it is not life threatening, urinary incontinence definitely has a negative impact on the patient’s quality of life Sountoulides et al., 2013. Beyond the frustration and embarrassment associated with pelvic floor dysfunction, many patients describe it as depressing, disheartening and devastating.
The first line of conservative treatment - and most often recommended - is pelvic floor muscle training Andersen et al., 2015. Over the past few years, some researchers have also recommended alternative exercise programs with a holistic approach such as Pilates and hypopressives to improve the patient’s quality of life and urinary incontinence symptoms (Santa Mina et al., 2015). These alternative pelvic floor muscle training programs draw upon the connection between the pelvic floor, it’s synergistic muscles (abdominal, pelvic, lumbar) and their interrelated role in posture and breathing Hodges, 2007; Sapsford, 2004; Madill and McLean, 2008; Talasz et al., 2010. Among these complementary exercise programs, hypopressives have gained increasing attention for the recovery of post-prostatectomy urinary incontinence Santa Mina et al., 2015; Mallol-Badellino, et al. 2015.
What is known about hypopressives for post-prostatectomy incontinence?
Although hypopressive exercise has become popular for women, some researchers, clinicians and practitioners have begun to apply these exercises for specific male issues such as urinary incontinence following a prostatectomy. Recently, a case-study I co-authored about an adapted program of hypopressive exercise for urinary incontinence following a radical prostatectomy surgery was published in the Journal of the Spanish physiotherapy association Chulvi-Medrano & Rial, 2018. We describe the case of a 46-year-old male with severe stress urinary incontinence six months after surgery. We used a pelvic floor exercise program consisting of hypopressive exercises as described in the Low Pressure Fitness level 1 practical manual Rial & Pinsach, 2017 combined with contraction of the pelvic floor muscles. Satisfactory results were obtained after the rehabilitation protocol as evidenced by a reduction from 3 daily pads to none. Of note, clinical trails have demonstrated the benefits of initiating a rehabilitation program to strengthen the pelvic floor as soon as possible after prostatectomy. Previously, I’ve studied hypopressive exercise for female urinary incontinence Rial et al., 2015 and for the improvement of female athletes pelvic floor function Álvarez et al., 2016. However, this was the first time we’ve studied hypopressives in the context of male urinary leakage.
In the same light, other researchers have also included hypopressives in their pelvic floor training protocol for post-prostatectomy urinary incontinence. For example, Serda et al (2010) and Mallol-Badellino (2015) used protocols that combined pelvic floor contractions with postural re-education and hypopressives. Both studies found improvements in the severity of involuntary leakages and improvements in the patients’ quality of life. Similar results are also described in the clinical case by Scarpelini et al. (2014) who used hypopressives and psoas stretching exercises to reduce urinary incontinence after prostatectomy.
But how do hypopressives work?
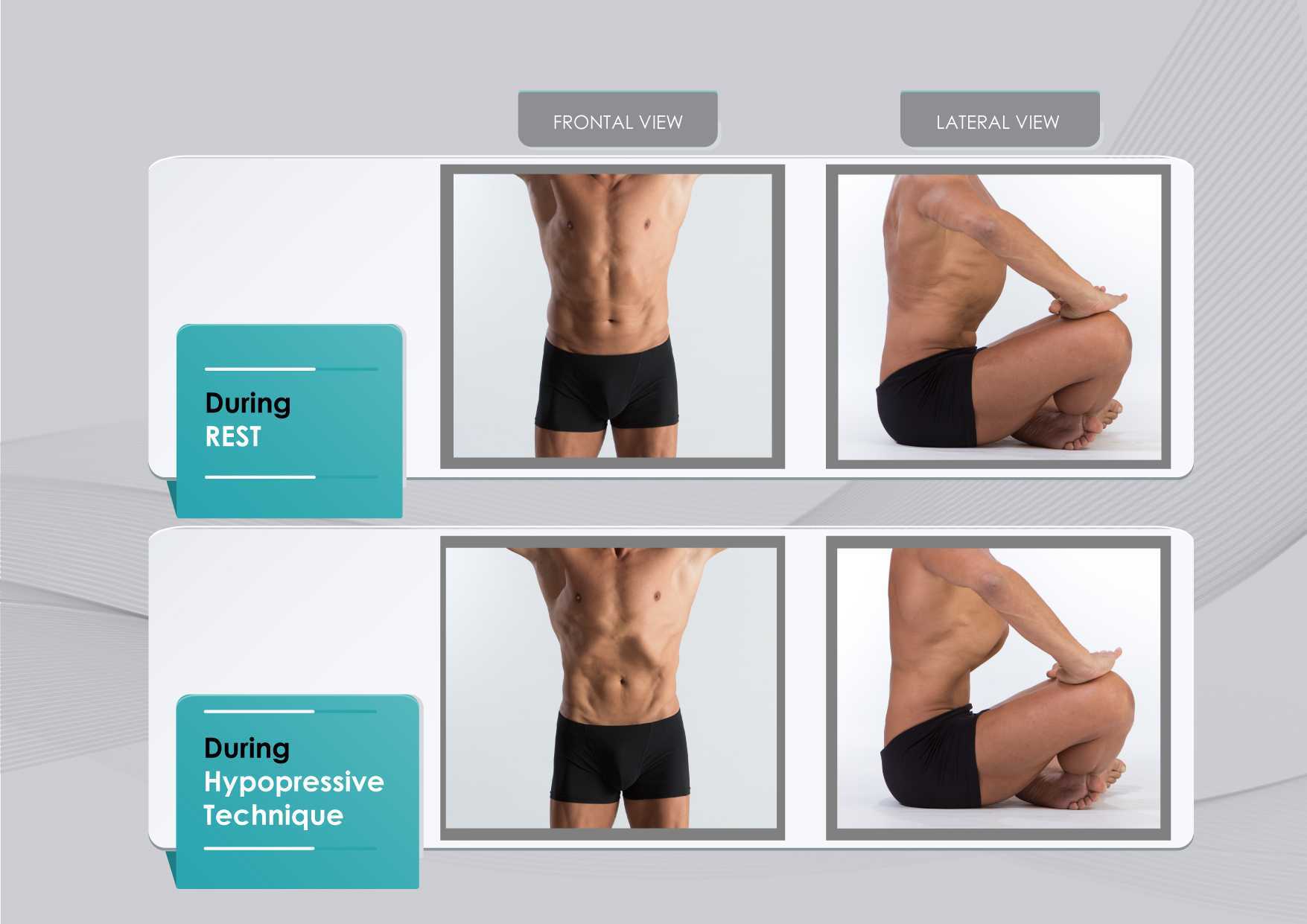
The hypothesis underlying the use of hypopressives as a complementary pelvic floor and core exercise program is that it retrains the core system with specific postural and breathing strategies while reducing pressure on the pelvic organs and structures. The most striking part of hypopressives breathing technique is the abdominal vacuum. This breathing maneuver involves a low pulmonary volume exhale-hold technique followed by a rib-cage expansion involving the activation of the inspiratory muscles. The rib-cage expansion during the breath-holding phase leads to a noticeable draw-in of the abdominal wall and simultaneously to the rise of the thoracic diaphragm. Recent observational studies have shown how the hypopressive technique was able to elevate the pelvic viscera and to activate the pelvic floor and deep core muscles in women trained with hypopressives Navarro et al., 2017. From an historical point of view, this characteristic breathing maneuver was first described and practiced as a yoga pranayama called Uddiyanha Bandha Omkar & Vishwas, 2009.
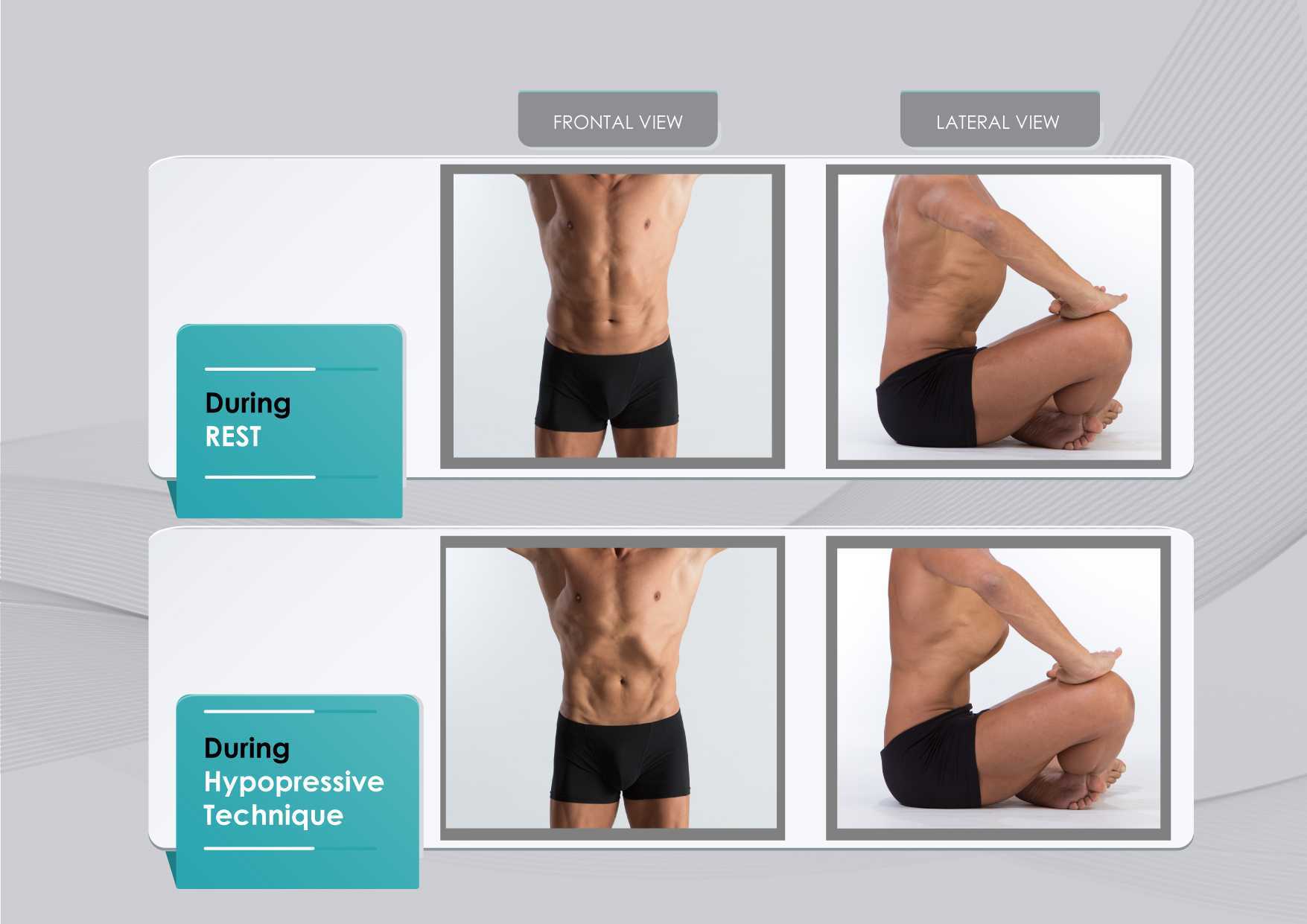
Figure 1 shows the anatomical behavior of the rib cage and the abdominal wall when performing the hypopressive breathing maneuver, which should not be confused with an abdominal hollowing, or a bracing maneuver. Anatomical observation of the thoracic and abdominal behavior during the breathing maneuver of the hypopressive exercise. Figure elaborated by the author.
In addition to breath control, the hypopressive technique involves a series of static and dynamic poses which operate on the hypothesis of training the stabilizing muscles of the spine, such as the core and pelvic muscles. In this sense, hypopressives are not exclusively a breathing technique, but rather they are an integrated whole-body technique. The practice of hypopressives involves body control, body awareness, postural correction and mindfulness throughout its different poses and postural techniques. The introduction of holistic exercise programs to train the synergist pelvic floor muscles and breathing patterns can be viewed as complementary tools for the restoration of a patient’s body awareness and functionality.
Another hypothesis of the effects of the hypopressive-breathing in the pelvic floor is the ability to move the pelvic viscera cranially as a consequence of the ribcage opening up after the breath-hold. This vacuum lifts the diaphragm and consequently creates an upward tension on the transversalis fascia, the peritoneum and other related fascial structures. In addition to the diaphragmatic suction effect, a correct alignment of the rib cage and pelvis during the exercise contributes to an improved suspension and position of the viscera in the pelvis. The mobility achieved with the breathing and its body sensations may be one of the reasons why hypopressives have also been recommended as a proprioceptive facilitator for those with low ability to “find their pelvic floor” Latorre et al., 2011.
It’s crucial to highlight that a complete surgical resection of the prostate will cause - in most of the cases - post-operative fibrosis and neurovascular damage Hoy-Land et al., 2014. Both, the neurovascular and musculoskeletal injuries are contributing factors for urinary incontinence post-prostatectomy. Subsequently, exercises focusing on increasing local vascular irrigation and re-activating the damaged musculature have been highlighted as the main goals to help patients recover continence. In this sense, breathing movements, fascia manipulation and decreased pelvic pressure can result in increased vascular supply. A previous study has shown an improvement in venous return of the femoral artery during the hypopressive-breathing maneuver Thyl et al., 2009. Collectively, all these factors may favor microcirculation in the pelvic area. Finally, the muscle activation of the pelvic floor and core muscles observed during the practice of hypopressives (Ithamar et al., 2017) and the changes of puborectalis and iliococcygeus muscles after an intensive pelvic floor muscle training (Dierick et al., 2018) are other factors that could have impact on urge incontinence, stress incontinence and overflow incontinence symptoms common after prostatectomy surgeries.
To date, the results from these investigations and clinical reports open new complementary pelvic floor training strategies for the treatment of post-prostatectomy incontinence. Hypopressives and pelvic floor muscle exercises are non-invasive, don’t require expensive material, and provide an exercise-based approach as part of a healthy lifestyle. However, qualified instruction, technique-driven progression and adherence to the intervention are critical components of any pelvic floor and hypopressive training protocol.
Álvarez M, Rial T, Chulvi-Medrano I, García-Soidán JL, Cortell JM. 2016. Can an eight-week program based on the hypopressive technique produce changes in pelvic floor function and body composition in female rugby players? Retos nuevas Tendencias en Educación Física, Deporte y Recreación, 30(2): 26-29.
Anderson CA, Omar MI, Campbell SE, Hunter KF, Cody JD, Glazener CM. 2015. Conservative management for postprostatectomy urinary incontinence. Cochrane Database Syst Rev, 1:CD001843.
Chulvi-Medrano I, Rial T. 2018. A case study of hypopressive exercise adapted for urinary incontinence following radical prostactetomy surgery. Fisioterapia, 40, 101-4. Doi: DOI: 10.1016/j.ft.2018.01.004
Dierick F, Galrsova E, Laura C, Buisseret F, Bouché FB, Martin L. 2018. Clinical and MRI changes of puborectalis and iliococcygeus after a short period of intensive pelvic floor muscles training with or without instrumentation. European Journal of Applied Physiology, doi:10.1007/s00421-018-3899-7
Ithamar, L., de Moura Filho, A.G., Benedetti-Rodrigues, M.A., Duque-Cortez, K.C., Machado, V.G., de Paiva-Lima, C.R.O., et al. 2017. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J. Bodywork. Mov. Ther. doi: 10.1016/j.jbmt.2017.06.011.
Latorre G, Seleme M, Resende AP, Stüpp L, Berghmans B. Hypopressive gymnastics: evidences for an alternative training for women with local proprioceptive deficit of the pelvic floor muscles. Fisioterapia Brasil 2011; 12(6): 463-6.
Hodges P. 2007. Postural and respiratory functions of the pelvic floor muscles. Neurourol Urodyn, 26(3): 362-371.
Hoyland K, Vasdev N, Abrof A, Boustead G. 2014. Post-radical prostatectomy incontinence: etiology and prevention. Rev Urol. 16(4), 181-8.
Madill, S., McLean, L. 2008. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle ontractions. J. Electromyogr. Kinesiol. 18, 955-64. doi: 10.1016/j.jelekin.2007.05.001.
Mallol-Badellino J., et al. 2015. Resultados en la calidad de vida y la severidad de la incontinencia urinaria en varones prostatectomizados por neoplasia de próstata. Rehabilitación, 49(4); 210-215.
Navarro, B., Torres, M., Arranz, B. Sánchez, O. 2017. Muscle response during a hypopressive exercise after pelvic floor physiotherapy: Assessment with transabdominal ultrasound. Fisioterapia. 39, 187-194. doi:10.1016/j.ft.2017.04.003.
Omkar, S., Vishwas, B. 2009. Yoga techniques as a means of core stability training. J. Bodywork Mov. Thep. 13, 98-103. doi: 10.1016/j.jbmt.2007.10.004.
Rial T, Chulvi-Medrano I, Cortell-Tormo JM, Álvarez M. 2015. Can an exercise program based on hypopressive technique improve the impact of urinary incontinence on women´s quality of life? Suelo Pélvico, 11:27-32.
Rial, T., Pinsach, P. 2017. Low Pressure Fitness practical manual level 1. International Hypopressive and Physical Therapy Institute, Vigo.
Santa Mina D, Au D, Alibhai S, Jamnicky L, Faghani N, Hilton W, Stefanky L, et al. 2015. A pilot randomized trial of conventional versus advanced pelvic floor exercises on treat urinary incontinence after radical prostatectomy: a study protocol. BMC Urology, 15. DOI 10.1186/s12894-015-0088-4
Sapsford R. 2004. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther, 9(1): 3-12.
Serdá B, Vesa, A. del Valle, y Monreal P. 2010. La incontinencia urinaria en el cáncer de próstata: diseño de un programa de rehabilitación. Actas Urológicas Españolas, 34(6): 522-30.
Scarpelini P, Andressa Oliveira F, Gabriela Cabrinha S, Cinira H. 2014. Protocolo de ginástica hipopressiva no tratamento da incontinência urinária pós-prostatectomia: relato de caso. UNILUS Ensino e Pesquisa, 11(23): 90-95
Talasz, H., Kofler, M., Kalchschmid, E., Pretterklieber, M., Lechleitner, M. 2010. Breathing with the pelvic floor? Correlation of pelvic floor muscle function and expiratory flows in healthy young nulliparous women. Int. Urogynecol. J. 21, 475-81. doi: 10.1007/s00192-009-1060-1.
Thyl S., Aude P, Caufriez M, Balestra C. 2009. Incidence de l'aspiration diaphragmatique associée à une apnée expiratoire sur la circulation de retour veineuse fémorale: étude par échographie-doppler. Kinésithérapie scientifique, 502; 27-30.
Coaching Patients to Engage in Positive Activities to Improve Outcomes
Substantial attention has been given to the impact of negative emotional states on persistent pain conditions. The adverse effects of anger, fear, anxiety and depression on pain are well-documented. Complementing this emphasis on negative emotions, Hanssen and colleagues suggest that interventions aimed at cultivating positive emotional states may have a role to play in pain reduction and/or improved well-being in patients, despite pain. They suggest positive affect may promote adaptive function and buffer the adversities of a chronic pain condition.
 Hanssen and colleagues propose positive psychology interventions could contribute to improved pain, mood and behavioral measures through various mechanisms. These include the modulation of spinal and supraspinal nociceptive pathways, buffering the stress reaction and reducing stress-induced hyperalgesia, broadening attention, decreasing negative pain-related cognitions, diminishing rigid behavioral responses and promoting behavioral flexibility.
Hanssen and colleagues propose positive psychology interventions could contribute to improved pain, mood and behavioral measures through various mechanisms. These include the modulation of spinal and supraspinal nociceptive pathways, buffering the stress reaction and reducing stress-induced hyperalgesia, broadening attention, decreasing negative pain-related cognitions, diminishing rigid behavioral responses and promoting behavioral flexibility.
In a feasibility trial, 96 patients were randomized to a computer-based positive activity intervention or control condition. The intervention required participants perform at least one positive activity for at least 15 minutes at least 1 day/week for 8 weeks. The positive activity included such tasks as performing good deeds for others, counting blessings, taking delight in life’s momentary wonders and pleasures, writing about best possible future selves, exercising or devoting time to pursuing a meaningful goal. The control group was instructed to be attentive to their surroundings and write about events or activities for at least 15 minutes at least 1 day/week for 8 weeks. Those in the positive activity intervention demonstrated significant improvements in pain intensity, pain interference, pain control, life satisfaction, and depression, and at program completion and 2-month follow-up. Based on these promising results, authors suggest that a full trial of the intervention is warranted.
Rehabilitation professionals often encourage patients with persistent pain conditions to participate in activities they enjoy. This research highlights the importance of this instruction and patient guidelines can include the activities identified in the Muller article. In addition, mindful awareness training may further enhance a patient’s experience as he or she learns to pay close attention to the physical sensations, emotions and thoughts that accompany positive experiences. I look forward to discussing this article as well as sharing the principles and practices of mindfulness in my upcoming course, Mindfulness-Based Pain Treatment at Samuel Merritt University, Oakland, CA. Course participants will learn about mindfulness and pain research, practice mindful breathing, body scan and movement and expand their pain treatment tool box with practical strategies to improve pain treatment outcomes. I hope you will join me!
Hanssen MM, Peters ML, Boselie JJ, Meulders A. Can positive affect attenuate (persistent) pain? Curr Rheumatol Rep. 2017;19(12):80.
Muller R, Gertz KJ, Molton IR, et al. Effects of a tailored positive psychology intervention on well-being and pain in individuals with chronic pain and physical disability: a feasibility trial. Clin J Pain.2016;32(1):32-44.
Angie Mueller PT, DPT is the instructor of Low Pressure Fitness and Abdominal Massage for Pelvic Floor Care, a new course on the hypopressive technique and abdominal massage for pelvic health. Join Dr. Mueller on July 27-29 in Princeton, NJ to learn more!
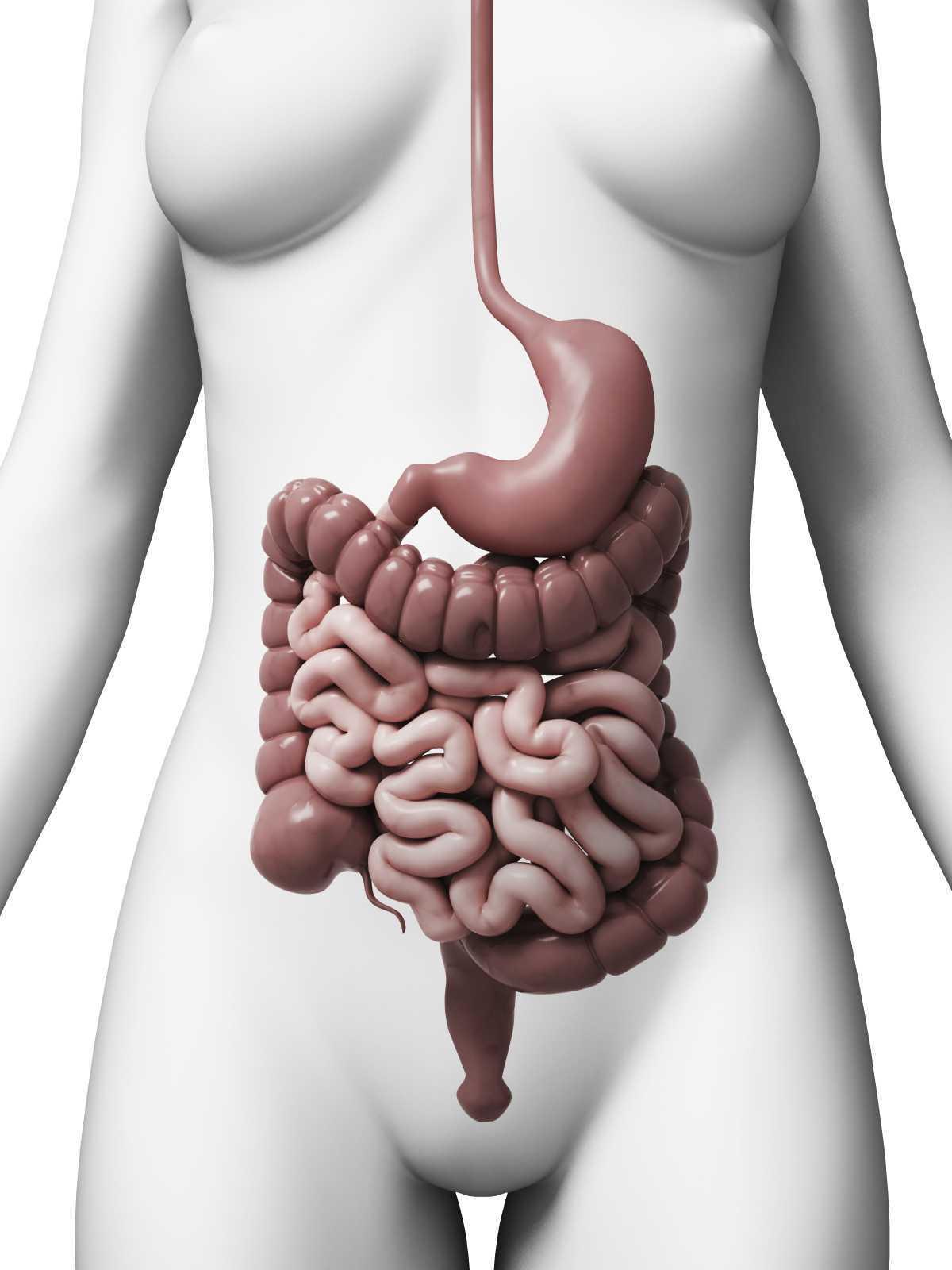
One of the first things I do as a pelvic PT when helping a woman recover from pelvic or core dysfunction, is center her uterus. I believe the uterus is the center of a women- biomechanically, physiologically, and energetically. I have seen that when the uterus is out of position, everything else in the pelvis and core is largely impacted and functions less efficiently. This includes muscular, gastrointentinal, liver, bowel and bladder, hormonal and sexual function.
 The uterus is supported by several important ligaments, which extend from the uterus out to the pelvic bones, as well as to the organs surrounding it- bladder, bowel and intestines. So if this magnificent central organ is out of her “center”- leaning forwards or backwards, or tipped to on side or the other- this can lead to a myofascial imbalance in the pelvis and cause symptoms of pelvic floor dysfunction, pain, and hormonal imbalances.
The uterus is supported by several important ligaments, which extend from the uterus out to the pelvic bones, as well as to the organs surrounding it- bladder, bowel and intestines. So if this magnificent central organ is out of her “center”- leaning forwards or backwards, or tipped to on side or the other- this can lead to a myofascial imbalance in the pelvis and cause symptoms of pelvic floor dysfunction, pain, and hormonal imbalances.
In treating thousands of women with pelvic dysfunction, I have observed that a uterus which is leaning too far forward (anteflexed) is often associated with urinary incontinence, issues with bladder urgency and frequency, and bladder prolapse (cystocele). A uterus that is tipped backwards is often associated with constipation, hemorrhoids and bowel prolapse (rectocele). A uterus that is leaning left or right is often associated with hip dysfunction, sacroiliac joint dysfunction and lumbo-pelvic alignment issues. This leads to and hip and/or knee and/or back pain due to asymmetrical pulling of the internal abdomino-pelvic fascia, especially the uterosacral and cardinal ligaments, which affects pelvic and sacral bone alignment, and then knee and ankle tracking. So centering the uterus will balance the internal pelvic and abdominal fascia, and can significantly improves cases of back pain, hip pain, knee or ankle pain.
Ensuring our organs are in their best position for receiving blood, lymph, nerve and hormonal support is critical to their health and function! If any organ in the body, especially the uterus, is not in its optimal position to receive blood, nerve, lymphatic and hormonal circulation, its function will be impacted. Therefore a mal-positioned uterus can also lead to problems with the menstrual cycle, painful periods, and fertility. When assisting any woman through a rehabilitative process, I have found it critical to appreciate how her uterine position contributes to and impacts her overall pelvic and core health- from a musculoskeletal, biomechanical and physiological perspective.
I have found that the best pelvic therapy outcomes result from use of both passive and active techniques to center the uterus. The first step is passive positioning of the uterus, which is most efficiently accomplished through abdominal massage. Abdominal self massage should be done daily. Abdominal massage will help to release any myofascial and ligamentous restrictions that are leading to a mal-positioned uterus. Abdominal massage also greatly improves blood flow and lymphatic circulation to the gut and pelvic organs leading to improved digestion and organ detoxification. Once her uterus is centered by the massage, it is important to immediately implement an active technique that will keep the uterus centered. This active uterine positioning technique must trigger the appropriate posture and breath that will keep her uterus centered with movement and throughout the activities of the day.
The second step to positioning her uterus is active activation of abdomino-pelvic musculature and key fascial chains that elevate and center the pelvic organs. This is accomplished through one of the latest core neuro-reeducation techniques- Low Pressure Fitness®. The Low Pressure Fitness methodology involves a seamless progression of postures and poses that cause a reduction in pressure in the abdomen and trigger an automatic response from the core muscles- abdominals, pelvic floor, multifidus, diaphragm. Low Pressure Fitness uses a breathing technique known as Hypopressive Breathing to reduce intra-abdominal pressure and optimize organ position. The term Hypopressive means “low pressure”. Traditional exercise, core training, sports, and most of our everyday activities are Hyperpressive – they increase the pressure in the abdomen. When the pressure in the abdomen is not appropriately managed, pressure increases, and this causes the spine to compress and the organs (especially the uterus) to move downward and away from their optimal “centered” position. But when the hypopressive breath is triggered, the pressure in the abdomen is reduced, the spine decompresses, the core musculature is gently strengthened, all of the organs lift, and the uterus is centered.
When the uterus is centered, magic happens… the fascial tension in the pelvis balances out; the resting tone of the abdominal and pelvic muscles improve and become easier to strengthen; the blood flow and lymphatic circulation in the pelvis is improved and sexual function and fertility is enhanced; hormones are better regulated and monthly cycles regulate; bowel and bladder function is optimized; the waistline reduces; pain in the back, abdomen and hips is reduced and posture improves. When all of these wonderful things occur, it is directly associated with improved energy, mood, creativity and self confidence. So remember, centering the uterus, through both active and passive techniques, is key when treating any woman. Self abdominal massage followed up by Low Pressure Fitness® are the most powerful techniques I have found to center the uterus and resolve pelvic and core dysfunction in women of all ages and lifestyles.
Using sEMG biofeedback to get real-time results
Tiffany Lee, MA, OTR, BCB-PMD and Jane Kaufman, PT, BCB-PMD are internationally board-certified clinicians in the treatment of pelvic floor muscle dysfunction through the Biofeedback Certification International Alliance. Combined, they have over fifty years of treatment experience using sEMG biofeedback. Their new course, “Biofeedback for Pelvic Floor Muscle Dysfunction”, will provide the nuts and bolts of this powerful tool so that clinicians can return to the clinic after this course with another component to their toolbox of treatment strategies.
 As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
So exactly what is biofeedback? Why should I consider this modality? Biofeedback provides a non-invasive opportunity for patients to see muscle function visualized on a computer screen in a way that allows for immediate feedback, simple representation of muscle function, and allows the patient and the clinician the opportunity to alter the physiological process of the muscle through basic learning strategies and skilled cues. Many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation is what helps patients really hone in on body awareness and connect all the dots. Here are a few comments that our patients have made; “I can now pay attention to my muscle while at work thanks to the visual of my muscle when sitting and standing”; “I needed to see my muscle to fully understand how to release the tension in it “; “I totally get what I need to do now that I have a clear picture of what you want”; “Seeing is believing”.
A 2017 study by Moretti, E., et al. is a great article that helps support the concept that measuring the pelvic floor electrical activity through a standard vaginal sensor is not always an option. For many patients, use of surface electrodes with peri-anal electrodes will provide the same reading and offer a more comfortable alternative for those patients who cannot use an internal sensor. This allows the clinician more opportunities to use this treatment modality with ease and assurance that the patient can learn from the visual representation of the muscle without fear of penetration from a sensor, and get great results!
In another study by Aysun Ozlu MD, et al. the authors conclude that biofeedback assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than home exercise program alone.
Herman & Wallace is offering a course for clinicians in Alexandria, Virginia this June that will answer all of your questions and concerns about this fabulous treatment tool: biofeedback! This course enables the clinician to learn and practice this valuable tool and gain knowledge about the benefits of this modality, so that treatment can begin immediately with ample opportunity for patient’s positive feedback and awareness of muscle function. Participants will experience being a biofeedback practitioner and patient (using a self-inserted vaginal or rectal sensor). Participants will be administering biofeedback assessments, analyzing and interpreting sEMG signals, conducting treatment sessions, and role-playing patient instruction/education for each diagnosis presented during the many hands-on lab experiences. Biofeedback is a powerful tool that can benefit your patient population, and add to your skill-set.
Moretti, E., Galvao de moura Filho, A., Correia de Almedia, J., Araaujo, C., Lemos, C. “Electromyographic assessment of women’s pelvic floor: What is the best place for a superficial sensor?” Neurology and Urodynamics; 2017; 9999:1-7.;
Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD, “Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence”
Speaking with a runner friend the other day, I mentioned I was writing a blog on yoga for pelvic pain. She had the same reaction many runners do, stating she has doesn’t care for yoga, she never feels like she is tight, and she would hate being in one position for so long. Ironically, neither of us has taken a yoga class, so any preconceived ideas about it are null and void. I told her yoga is being researched for beneficial health effects, and one day we just might find ourselves in a class together!
 Saxena et al.2017 published a study on the effects of yoga on pain and quality of life in women with chronic pelvic pain. The randomized case controlled study involved 60 female patients, ages 18-45, who presented with chronic pelvic pain. They were randomly divided into two groups of 30 women. Group I received 8 weeks of treatment only with nonsteroidal anti-inflammatory medication (NSAIDS). Group II received 1 hour, 5 days per week, for 8 weeks of yoga therapy (asanas, pranayama, and relaxation) in addition to NSAIDS (as needed). Table 1 in the article outlines the exact protocol of yoga in which Group II participated. The subjects were assessed pre- and post-treatment with pain scores via visual analog scale score and quality of life with the World Health Organization quality of life-BREF questionnaire. In the final analysis, Group II showed a statistically significant positive difference pre and post treatment as well as in comparison to Group I in both categories. The authors concluded yoga to be an effective adjunct therapy for patients with chronic pelvic pain and an effective option over NSAIDS for pain.
Saxena et al.2017 published a study on the effects of yoga on pain and quality of life in women with chronic pelvic pain. The randomized case controlled study involved 60 female patients, ages 18-45, who presented with chronic pelvic pain. They were randomly divided into two groups of 30 women. Group I received 8 weeks of treatment only with nonsteroidal anti-inflammatory medication (NSAIDS). Group II received 1 hour, 5 days per week, for 8 weeks of yoga therapy (asanas, pranayama, and relaxation) in addition to NSAIDS (as needed). Table 1 in the article outlines the exact protocol of yoga in which Group II participated. The subjects were assessed pre- and post-treatment with pain scores via visual analog scale score and quality of life with the World Health Organization quality of life-BREF questionnaire. In the final analysis, Group II showed a statistically significant positive difference pre and post treatment as well as in comparison to Group I in both categories. The authors concluded yoga to be an effective adjunct therapy for patients with chronic pelvic pain and an effective option over NSAIDS for pain.
In the Pain Medicine journal, Huang et al.2017 presented a single-arm trial attempting to study the effects of a group-based therapeutic yoga program for women with chronic pelvic pain (CPP), focusing on severity of pain, sexual function, and overall well-being. The comprehensive program was created by a group of women’s health researchers, gynecological and obstetrical medical practitioners, yoga consultants, and integrative medicine clinicians. Sixteen women with severe pelvic pain of at least 6 months’ duration were recruited. The group yoga classes focused on lyengar-based techniques, and the subjects participated in group classes twice a week and home practice 1 hour per week for 6 weeks. The Impact of Pelvic Pain (IPP) questionnaire assessed how the participants’ pain affected their daily life activities, emotional well-being, and sexual function. Sexual Health Outcomes in Women Questionairre (SHOW-Q) offered insight to sexual function. Daily logs recorded the women’s self-rated pelvic pain severity. The results showed the average pain severity improved 32% after the 6 weeks, and IPP scores improved for daily living (from 1.8 to 0.9), emotional well-being (from 1.7 to 0.9), and sexual function (from 1.9 to 1.0). The SHOW-Q "pelvic problem interference" scale also improved from 53 to 23. The multidisciplinary panel concluded they found preliminary evidence that teaching yoga to women with CPP is feasible for pain management and improvement of quality of life and sexual function.
Whatever treatment we provide for our patients, we need to consider the individual and their often biased opinions or perceptions. Providing research and educating each patient on the efficacy behind the proposed therapy will likely impact their outcome. The Yoga for Pelvic Pain course can enhance a clinician’s understanding and allow them to better implement a potentially life-changing therapy for their clients.
Saxena, R., Gupta, M., Shankar, N., Jain, S., & Saxena, A. (2017). Effects of yogic intervention on pain scores and quality of life in females with chronic pelvic pain. International Journal of Yoga, 10(1), 9–15. http://doi.org/10.4103/0973-6131.186155
Huang, AJ, Rowen, TS, Abercrombie, P, Subak, LL, Schembri, M, Plaut, T, & Chao, MT. (2017). Development and Feasibility of a Group-Based Therapeutic Yoga Program for Women with Chronic Pelvic Pain. Pain Medicine. http://doi.org/10.1093/pm/pnw306
What if we were only taught treatment techniques during our healthcare training with no theory or explanation as to why or on whom or under what circumstances they should be used? Focusing on “how to” but ignoring the “discernment as to why” would make for a weak clinician. Manual therapy for the pelvic floor is a treatment approach to implement once we have used our heads and palpation skills to reveal the underlying source of dysfunction.

Pastore and Katzman (2012) published a thorough article describing the process of recognizing when myofascial pain is the source of chronic pelvic pain in females. They discuss active versus latent myofascial trigger points (MTrPs), which are painful nodules or lumps in muscle tissue, with the latter only being symptomatic when triggered by physical (compression or stretching) or emotional stress. Hyperalgesia and allodynia are generally present in patients with MTrPs, and muscles with MTrPs are weaker and limit range of motion in surrounding joints. In pelvic floor muscles, MTrPs refer pain to the perineum, vagina, urethra, and rectum but also the abdomen, back, thorax, hip/buttocks, and lower leg. The authors suggest detecting a trigger point by palpating perpendicular to the muscle fiber to sense a taut band and tender nodule and advise using the finger pads with a flat approach in the abdomen, pelvis and perineum. They emphasize a multidisciplinary approach to finding and treating MTrPs and making sure urological, gynecological, and/or colorectal pathologies are addressed. A thorough subjective and physical exam that leads to proper diagnosis of MTrPs should be followed by manual physical therapy techniques and appropriate medical intervention for any corresponding pathology.
Halder et al. (2017) investigated the efficacy of myofascial release physical therapy with the addition of Botox in a retrospective case series for women with myofascial pelvic pain. Fifty of the 160 women who had Botox and physical therapy met the inclusion/exclusion criteria, and the primary complaint in all those subjects was dyspareunia. The Botox was administered under general anesthesia, and then the same physician performed soft tissue myofascial release transvaginally for 10-15 minutes, with 10-15 additional minutes performed if rectus muscles had trigger points. The patients were seen 2 weeks and 8 weeks posttreatment. Average pelvic pain scores decreased significantly pre- and posttreatment, with 58% of subjects reporting improvements. Significantly fewer patients (44% versus 100%) presented with trigger points on pelvic exam after the treatment. The patients who did not show improvement tended to have inflammatory or irritable bowel diseases or diverticulosis. Blocking acetylcholine receptors via Botox in combination with pelvic floor physical therapy could possibly provide longer symptom-free periods. Although the nature of the study could not determine a specific interval of relief, the authors were encouraged as an average of 15 months passed before 5 of the patients sought more treatment.
The need for the specific treatment for myofascial pelvic pain is determined by a clinician competent in palpation of the pelvic floor musculature finding trigger points and restrictions in the tissue. Listening to a patient’s symptoms and understanding pelvic pathology allow for better treatment planning. Manual Therapy Techniques for the Pelvic Rehab Therapist is a comprehensive course to enhance knowledge in your head to lead your hands in the right direction for assessing/treating patients with pelvic pain.
Pastore, E. A., & Katzman, W. B. (2012). Recognizing Myofascial Pelvic Pain in the Female Patient with Chronic Pelvic Pain. Journal of Obstetric, Gynecologic, and Neonatal Nursing : JOGNN / NAACOG, 41(5), 680–691. http://doi.org/10.1111/j.1552-6909.2012.01404.x
Halder, G. E., Scott, L., Wyman, A., Mora, N., Miladinovic, B., Bassaly, R., & Hoyte, L. (2017). Botox combined with myofascial release physical therapy as a treatment for myofascial pelvic pain. Investigative and Clinical Urology, 58(2), 134–139. http://doi.org/10.4111/icu.2017.58.2.134
While recently visiting Seattle with my daughter, we had the pleasure of talking with Dr. Ghislaine Robert, owner of Sparclaine Regenerative Medicine. She is a highly respected sports medicine doctor who has steered much of her practice towards regenerative medicine, with a focus on stem cell and platelet enriched plasma (PRP) injections. She brought to my attention the use of stem cells for pelvic floor disorders. And, like any successful practitioner, she encouraged me to research it for myself.
In 2015, Cestaro et al. reported early results of 3 patients with fecal incontinence receiving intersphincteric anal groove injections of fat tissue. They aspirated about 150ml of the fat tissue and used the Lipogem system technology lipofilling technique to provide micro-fragmented and transplantable clusters of lipoaspirate. The intersphincteric space was then injected with the lipoaspirate. A proctology exam was performed at 1 week, 1 month, and 6 months following the procedure. All 3 patients all had reduced Wexner incontinence scores 1 month post-treatment and a significant improvement in quality of life 6 months post-procedure. Resting pressure of the internal anal sphincter increased after 6 months, and the internal anal sphincter showed increased thickness.
A 2016 study by Mazzanti et al., used rats to explore whether unexpanded bone marrow-derived mononuclear mesynchymal cells (MNC) could effectively repair anal sphincter healing since expanded ones (MSC) had already been shown to enhance healing after injury in a rat model. They divided 32 rats into 4 groups: sphincterotomy and repair (SR) with primary suture of anal sphincters and a saline intrasphincteric injection (CTR); SR of anal sphincter with in-vitro expanded MSC; SR of anal sphincter with minimally manipulated MNC; and, a sham operation with saline injection. Muscle regeneration as well as contractile function was observed in the MSC and MNC groups, while the control surgical group demonstrated development of scar tissue, inflammatory cells and mast cells between the ends of the interrupted muscle layer 30 days post-surgery. Ultimately, the authors found no significant difference between expanded or unexpanded bone marrow stem cell types used. Post-sphincter repair can be enhanced by stem cell therapy for anal incontinence, even when the cells are minimally manipulated.
Finally, in 2017, Sarveazad et al. performed a double-blind clinical trial in humans using human adipose-derived stromal/stem cells (hADSCs) from adipose tissue for fecal incontinence. The hADSCs secrete growth factor and can potentially differentiate into muscle cells, which make them worth testing for improvement of anal sphincter incontinence. They used 18 subjects with sphincter defects, 9 undergoing sphincter repair with injection of hADSCs and 9 having surgery with a phosphate buffer saline injection. After 2 months, there was a 7.91% increase in the muscle mass in the area of the lesion for the cell group compared to the control. Fibrous tissue replacement with muscle tissue, allowing contractile function, may be a key in the long term for treatment of fecal incontinence.
As long as accessing human-derived stem cells is a viable option for patients, the preliminary studies show promise for success. With fecal incontinence being such a debilitating problem for people, especially socially, stem cells are definitely an up and coming treatment, and we should all keep up on this research. After all, who wouldn’t spare some adipose tissue for life-changing, functional gains?
Cestaro, G., De Rosa, M., Massa, S., Amato, B., & Gentile, M. (2015). Intersphincteric anal lipofilling with micro-fragmented fat tissue for the treatment of faecal incontinence: preliminary results of three patients. Videosurgery and Other Miniinvasive Techniques, 10(2), 337–341. http://doi.org/10.5114/wiitm.2014.47435
Mazzanti, B., Lorenzi, B., Borghini, A., Boieri, M., Ballerini, L., Saccardi, R., … Pessina, F. (2016). Local injection of bone marrow progenitor cells for the treatment of anal sphincter injury: in-vitro expanded versus minimally-manipulated cells. Stem Cell Research & Therapy, 7, 85. http://doi.org/10.1186/s13287-016-0344-x
Sarveazad, A., Newstead, G. L., Mirzaei, R., Joghataei, M. T., Bakhtiari, M., Babahajian, A., & Mahjoubi, B. (2017). A new method for treating fecal incontinence by implanting stem cells derived from human adipose tissue: preliminary findings of a randomized double-blind clinical trial. Stem Cell Research & Therapy, 8, 40. http://doi.org/10.1186/s13287-017-0489-2
During labor, I had no problem breathing out. My hang up came when I had to inhale - actually oxygenate my blood and maintain a healthy heart rate for my almost newborn baby. When extra staff filled the delivery room, and an oxygen mask was placed over my face, my husband remained calm but later told me how freaked out he was. He was watching the monitors that showed a drop in my vitals as well as our baby’s. In retrospect, I wonder if practicing yoga, particularly the breathing techniques involved with pranayama practice, could have prevented that moment.
 A research article by Critchley et al., (2015) broke down breathing to a very scientific level, determining the consequences of slow breathing (6 breaths/minute) versus induced hypoxic challenges (13% inspired O2) on the cardiac and respiratory systems and their central neural substrates. Functional magnetic resonance imaging measured the 20 healthy subjects’ specific brain activity during the slow and normal rate breathing. The authors mentioned the controlled slow breathing of 6 breaths/minute is the rate encouraged during yoga practice. This rate decreases sympathetic activity, lessening vasoconstriction associated with hypertension, and it prevents physiological stress from affecting the cardiovascular system. Each part of the brain showed responses to the 2 conditions, and the general conclusion was modifying breathing rate impacted autonomic activity and improved both cardiovascular and psychological health.
A research article by Critchley et al., (2015) broke down breathing to a very scientific level, determining the consequences of slow breathing (6 breaths/minute) versus induced hypoxic challenges (13% inspired O2) on the cardiac and respiratory systems and their central neural substrates. Functional magnetic resonance imaging measured the 20 healthy subjects’ specific brain activity during the slow and normal rate breathing. The authors mentioned the controlled slow breathing of 6 breaths/minute is the rate encouraged during yoga practice. This rate decreases sympathetic activity, lessening vasoconstriction associated with hypertension, and it prevents physiological stress from affecting the cardiovascular system. Each part of the brain showed responses to the 2 conditions, and the general conclusion was modifying breathing rate impacted autonomic activity and improved both cardiovascular and psychological health.
Vinay, Venkatesh, and Ambarish (2016) presented a study on the effect of 1 month of yoga practice on heart rate variability in 32 males who completed the protocol. The authors reported yoga is supposed to alter the autonomic system and promote improvements in cardiovascular health. Not just the breathing but also the movements and meditation positively affect mental health and general well-being. The subjects participated in 1 hour of yoga daily for 1 month, and at the end of the study, the 1 bpm improvement in heart rate was not statistically significant. However, heart rate variability measures indicated a positive shift of the autonomic system from sympathetic activity to parasympathetic, which reduces cortisol levels, improves blood pressure, and increases circulation to the intestines.
Bershadsky et al., (2014) studied the effect of prenatal Hatha yoga on cortisol levels, affect and depression in the 34 women who completed pre, mid, and post pregnancy saliva tests and questionnaires. While levels of cortisol increase naturally with pregnancy, yoga was found to minimize the mean levels compared to the days the subjects did not participate in yoga. After a single 90-minute yoga session, during which breathing was emphasized throughout the session, women had higher positive affect; but, the cortisol level was not significantly different from the control group. Overall, the authors concluded yoga had potential to minimize depression and cortisol levels in pregnancy.
Considering the positive effect of slow breathing practiced in yoga, the positive shift in the autonomic nervous system function and the decrease in cortisol levels, yoga is gaining credibility as an effective adjunct to treatment during pregnancy. If a woman enters the delivery room with a solid practice of slow breathing under her belt, she may be equipped to handle the intensity of contractions and the pain of pushing a little better. Yoga may help a woman breathe for her life and her baby’s as well.
If you're interested in learning more about yoga for pregnant patients, consider attending Yoga as Medicine for Pregnancy with Ginger Garner, PT, DPT, ATC/LAT, PYT. The next opportunity is in Fort Lauderdale, FL on January 28th and 29th, 2017. Don't miss out!
Critchley, H. D., Nicotra, A., Chiesa, P. A., Nagai, Y., Gray, M. A., Minati, L., & Bernardi, L. (2015). Slow Breathing and Hypoxic Challenge: Cardiorespiratory Consequences and Their Central Neural Substrates. PLoS ONE, 10(5), e0127082.
Vinay, A., Venkatesh, D., & Ambarish, V. (2016). Impact of short-term practice of yoga on heart rate variability. International Journal of Yoga, 9(1), 62–66.
Bershadsky, S., Trumpfheller, L., Kimble, H. B., Pipaloff, D., & Yim, I. S. (2014). The effect of prenatal Hatha yoga on affect, cortisol and depressive symptoms. Complementary Therapies in Clinical Practice, 20(2), 106–113.