As someone who has spent nearly two decades marketing myself, my practice, or practices for employers, I have learned a lot of skills by trial and error. One of my favorite strategies to expand my professional network is to “Follow the Patient.” By this I mean to follow the patient to a specialist consult, to a procedure, or to a referral that you helped to coordinate. This must be done with the patient in mind, first and foremost, and then also the provider and their practice environment, so as not to have that practice shut the door on you in the future. Of course, this process can look different if you are in a health network because as an insider, you will likely be more welcome and have all the right credentials in order to simply attend a patient’s provider visit. If you are in a private practice, there are sometimes more hoops and permissions to negotiate. Following are some tips I have learned about this strategy of nurturing referral sources.
 Offer the idea to the patient and see if they are open to it. It might sound like this: “If you are interested, I may be able to accompany you to your upcoming appointment. Does that interest you?” It’s very important that the patient is consenting to you being in attendance at their appointment, as the visit is for them. It may be best to not promise that you can clear your schedule, or coordinate the visit, but finding out if the patient is open to the idea is the first step.
Offer the idea to the patient and see if they are open to it. It might sound like this: “If you are interested, I may be able to accompany you to your upcoming appointment. Does that interest you?” It’s very important that the patient is consenting to you being in attendance at their appointment, as the visit is for them. It may be best to not promise that you can clear your schedule, or coordinate the visit, but finding out if the patient is open to the idea is the first step.
2. Check in with the provider’s office. This can be accomplished by you or by the patient. This might sound like this: “I’d like to be sure that your provider would welcome me at your appointment. Would you prefer to contact the provider’s office or shall I?” In my experience, the provider’s office will say “if it’s ok with the patient, it’s fine with us!” Typically, a patient can bring whomever they like to an appointment, so that’s not much of an issue, unless there is close quarters or some other limiting scenario. The good thing about giving a heads up is it allows the provider’s office the opportunity to know that you may be joining your patient. I was able to follow a patient into a hernia repair surgery, and the nurses were so surprised that a physical therapist was in the prep room, they asked me “does the doctor know you are here?” in which case I was able to affirm that I indeed had permission from the surgeon.
3. When you attend the visit, allow the patient to introduce you or politely introduce yourself. Then listen. This is not the time to tell the medical provider all of the wonderful things you have been doing, or all of the things you have to offer their patients. Sometimes when reporting their history, the patient will look questioningly at me to recall details, and unless I am needed to give a brief response, I like to be quiet and stay out of the story until later. This is the time for the patient and the provider to get to know each other, establish rapport, and fewer interruptions are best.
4. Be prepared to summarize your thoughts when given the opportunity to share. Typically I have found that a medical provider will at some point turn and ask me a few questions, or simply state, “Do you have anything to add?” at which point I try to make concise yet thoughtful statements about the patient’s progress, continued challenges, and the reasoning behind the referral if I was the one to coordinate it. The summary might sound like this: “The original severe pain locations have eased, function has improved in this way, and the symptom or issue that is persisting is this. I was interested in knowing if there is potentially something else going on, or if you have a recommendation towards furthering their progress.” At this point, it’s best to not get too far ahead of yourself, or put expectations in front of the patient beyond a brief summary. In other words, don’t request specific imaging or suggest a particular procedure, as this may create an imbalance in the patient’s expectations and the reality of what takes place. If the provider wants more details or thoughts from you, they are likely to ask directly. (You can also send a progress report or summary letter prior to your visit if you have specific thoughts or concerns about what is going on.)
5. Allow the visit to unfold, listen carefully and take mental or written notes. I have often found that I recall details of anatomy, medications, or suggested interventions easily and the patient may ask about the details in a follow-up visit. This type of partnership allows the patient to have “another pair of ears” and can serve as a valuable part of the rehabilitation care planning. For example, perhaps the provider said, “Let’s try this imaging, if nothing of interest shows up, continue rehabilitation for 6 weeks. If no significant progress, I’d like to see you back here within a couple of months from today.” This allows the therapist to note that a provider visit was requested at 6 weeks following the appointment.
Marketing our services, in the long run, and especially in pelvic health, is critical in sharing awareness of the role of pelvic rehabilitation. Marketing is about relationships, and the easiest way to create a relationship is face to face. “Following” a patient along their healing journey, while it may take time out of the clinic for you, is a valuable way of engaging with providers and of being part of a collaborative process. When another provider or therapist requests that I see their patient to offer another view, I find it helpful to welcome the referring therapist to join the patient as well. This can lead to valuable discussions, sharing of information, and ultimately the patient may experience more efficient care that is directed to optimal strategies.
When reading published research on a subject matter directly relating to what we do in our career, we may need to remember the expression, “Don’t throw the baby out with the bathwater.” Sometimes the test results for a promising hypothesis are not statistically significant, and we can close our minds to the concept entirely. If we skim the abstract and hone in on the “results” or “conclusion” rather than reading the whole article, particularly a study’s limitations, we may drop a sound clinical pearl down the drain.
A research article published in May 2017 by Amorim et al., looked at the force generation and maintenance of the pelvic floor muscles when combined with hip adduction or abduction contractions. They hypothesized that pelvic floor muscle (PFM) contraction combined with hip abduction contraction (rather than adduction) should produce a greater PFM contraction because of the myofascial connection of the obturator internus to the levator ani muscle. The study included 20 nulliparous women without pelvic floor dysfunction. The pelvic floor muscle contraction was measured in isolation, with 30% and 50% maximum hip adduction contraction, and with 30% and 50% maximum hip abduction contraction. The forces were measured with a cylindrical, intravaginal strain-gauge for PFM and another strain-gauge around the hips for adduction/abduction force generation. The women were given visual feedback to help them obtain the required hip contraction force. An average of 3 contractions (10 seconds each with a 1 minute rest) was used for each condition. This was all performed again 4 weeks later.
 The results of this study by Amorim et al.2017 did not support the hypothesis. No statistically significant difference was found among any of the conditions measured. The intravaginal PFM force generation was not different when combined with hip abduction versus hip adduction contraction. Neither hip adduction nor abduction made a significant change in force of the PFM contraction compared to isolated PFM contraction. The authors had to conclude there is no evidence to support the efficacy of combining PFM training with contraction of the hip abductors or adductors.
The results of this study by Amorim et al.2017 did not support the hypothesis. No statistically significant difference was found among any of the conditions measured. The intravaginal PFM force generation was not different when combined with hip abduction versus hip adduction contraction. Neither hip adduction nor abduction made a significant change in force of the PFM contraction compared to isolated PFM contraction. The authors had to conclude there is no evidence to support the efficacy of combining PFM training with contraction of the hip abductors or adductors.
Even Amorim et al., admitted the study had limitations, and the benefit of PFM training combined with the hip contractions could exist under more “chronic” conditions rather than the brief testing period used in the research. They also used healthy women who had no children, which could make for a different outcome than if they used women with pelvic dysfunction. The specificity of the strain-gauges and the feedback given was not flawless. The authors encouraged further study on the subject. Perhaps there could be an important correlation between PFM and hip abduction contraction not yet found.
Reading research is an integral part of being a responsible healthcare professional, but without solid discernment, we could be entranced or blinded by bubbles as the “baby” escapes us. Taking a course (online or in person) that enhances overall understanding of a subject matter such as the correlation between the lumbopelvic region and the hip can equip the practitioner with a broader foundation upon which clinical decisions can be made. Recognize what concepts to keep and which to wash away, and realize one patient may benefit from what a randomized controlled trial could not cleanly prove to work.
Amorim, A. C., Cacciari, L. P., Passaro, A. C., Silveira, S. R. B., Amorim, C. F., Loss, J. F., & Sacco, I. C. N. (2017). Effect of combined actions of hip adduction/abduction on the force generation and maintenance of pelvic floor muscles in healthy women. PLoS ONE, 12(5), e0177575. http://doi.org/10.1371/journal.pone.0177575
One of my greatest nemeses when I was racing at 30 years of age was a woman in her 50’s. Although I hated losing to her, I was always inspired by her speed at her age. She motivated me to continue training hard, realizing my fastest days could be yet to come. As I now race in the “master’s” category in my 40’s, I still find myself crossing the line behind an older competitor occasionally. Research shows I should take heart and keep in step with females who continue to move their bodies beyond menopause.
 Mazurek et al., (2017) studied how organized physical activity among post-menopausal women could reduce cardiovascular risk. The study included 35 sedentary women aged 64.7 ± 7.7 years who had no serious health issues. They all participated in the Active Leisure Time Programme (ALTP) 3 times per day for 40–75 minute sessions for 2 weeks, including 39 physical activities. Exercise intensity stayed within 40–60% of maximal HR, and ratings of perceived exertion (RPE) on the Borg scale stayed between 8 and 15 points. This exercise training was followed by 3 months of the Prevent Falls in the Elderly Programme (PFEP), which is a general fitness exercise program to prevent falls in the elderly. Health status was measured at baseline, 2 weeks into the program, and after 3 months. The results showed significant reductions in central obesity, which increased the exercise and aerobic capacity of the subjects and improved lipid profiles. A significant reduction also occurred in the absolute 10-year risk of death from cardiac complications. The authors concluded these exercise programs could be effective in preventing primary and secondary cardiovascular disease in the >55 years old female population.
Mazurek et al., (2017) studied how organized physical activity among post-menopausal women could reduce cardiovascular risk. The study included 35 sedentary women aged 64.7 ± 7.7 years who had no serious health issues. They all participated in the Active Leisure Time Programme (ALTP) 3 times per day for 40–75 minute sessions for 2 weeks, including 39 physical activities. Exercise intensity stayed within 40–60% of maximal HR, and ratings of perceived exertion (RPE) on the Borg scale stayed between 8 and 15 points. This exercise training was followed by 3 months of the Prevent Falls in the Elderly Programme (PFEP), which is a general fitness exercise program to prevent falls in the elderly. Health status was measured at baseline, 2 weeks into the program, and after 3 months. The results showed significant reductions in central obesity, which increased the exercise and aerobic capacity of the subjects and improved lipid profiles. A significant reduction also occurred in the absolute 10-year risk of death from cardiac complications. The authors concluded these exercise programs could be effective in preventing primary and secondary cardiovascular disease in the >55 years old female population.
Nyberg et al., (2016) took a physiological look at exercise training on the vascular function of pre- and postmenopausal women, studying the prostanoid system. Prostanoids are vasoconstrictors, and prostacyclins are vasodilators. The loss of estrogen in menopause affects the ability of the vasodilators to function properly or even be produced, thus contributing to vascular decline. The authors checked the vasodilator response to an intra-arterial fusion of a prostacyclin analog epoprostenol as well as acetylocholine in 20 premenopausal and 16 early postmenopausal women before and after a 12-week exercise program. Pre-exercise, the postmenopausal women had a reduced vasodilator response. The women also received infusion of ketorolac (an inhibitor of cyclooxygenase) along with acetylcholine, creating a vasoconstriction effect, and the vascular response was reduced in both groups. The infusions and analyses were performed again after 12 weeks of exercise training, and the exercise training increased the vasodilator response to epoprostenol and acetylcholine in the postmenopausal group. The reduced vasodilator response to epoprostenol prior to exercise in early postmenopausal women suggests hormonal changes affect the capacity of prostacyclin signaling; however, the prostanoid balance for pre and postmenopausal women was unchanged. Ultimately, the study showed exercise training can still have a positive effect on the vascularity of newly postmenopausal women.
There are randomized controlled clinical trials and scientific evidence supporting the importance to keep moving as women (and men) age. Menopause should not be a self-proclaimed pause from activity in life. Not everyone has to become a competitive athlete to preserve cardiac and vascular integrity as we age, but we need to engage in some physical activity to keep our systems running for years to come.
Those interested in learning more about menopause rehabilitation considerations should consider attending Menopause Rehabilitation and Symptom Management.
Mazurek, K., Żmijewski, P., Kozdroń, E., Fojt, A., Czajkowska, A., Szczypiorski, P., Tomasz Mazurek, T. (2017). Cardiovascular Risk Reduction in Sedentary Postmenopausal Women During Organised Physical Activity. Kardiologia Polska. 75, 5: 476–485. http://doi:10.5603/KP.a2017.0035
Nyberg, M., Egelund, J., Mandrup, C., Nielsen, M., Mogensen, A., Stallknecht, B., Bangsbo, J., Hellsten, Y. (2016). Early Postmenopausal Phase Is Associated With Reduced Prostacyclin-Induced Vasodilation That Is Reversed by Exercise Training: The Copenhagen Women Study. Hypertension. 68:1011-1020. https://doi.org/10.1161/HYPERTENSIONAHA.116.07866
As I read about male phimosis, I thought about a shirt that just won’t go over my son’s big noggin. I tug and pull, and he screams as his blond locks stick up from static electricity. Ultimately, if I want this shirt to be worn, I either have to cut it or provide a prolonged stretch to the material, or my child will suffocate in a polyester sheath. This is remotely similar to the male with physiological phimosis.
 In a review article, Chan and Wong (2016) described urological problems among children, including phimosis. They reported “physiological phimosis” is when the prepuce cannot be retracted because of a natural adhesion to the glans. Almost all normal male babies are born with a foreskin that does not retract, and it becomes retractable in 90% of boys once they are 3 years old. A biological process occurs, and the prepuce becomes retractable. In “pathological phimosis” or balanitis xerotica obliterans, the prepuce, glans, and sometimes even the urethra experience a progressive inflammatory condition involving inflammation of the glans penis, an unusually dry lesion, and occasional endarteritis. Etiology is unknown, but males by their 15th birthday report a 0.6% incidence, and the clinical characteristics include a white tip of the foreskin with a ring of hard tissue, white patches covering the glans, sclerotic changes around the meatus, meatal stenosis, and sometimes urethral narrowing and urine retention.
In a review article, Chan and Wong (2016) described urological problems among children, including phimosis. They reported “physiological phimosis” is when the prepuce cannot be retracted because of a natural adhesion to the glans. Almost all normal male babies are born with a foreskin that does not retract, and it becomes retractable in 90% of boys once they are 3 years old. A biological process occurs, and the prepuce becomes retractable. In “pathological phimosis” or balanitis xerotica obliterans, the prepuce, glans, and sometimes even the urethra experience a progressive inflammatory condition involving inflammation of the glans penis, an unusually dry lesion, and occasional endarteritis. Etiology is unknown, but males by their 15th birthday report a 0.6% incidence, and the clinical characteristics include a white tip of the foreskin with a ring of hard tissue, white patches covering the glans, sclerotic changes around the meatus, meatal stenosis, and sometimes urethral narrowing and urine retention.
This review article continues to discuss the appropriate treatment for phimosis (Chan & Wong 2016). Once phimosis is diagnosed, the parents of the young male need to be educated on keeping the prepuce clean. This involves retracting the prepuce gently and rinsing it with warm water daily to prevent infection. Parents are warned against forcibly retracting the prepuce. A study has shown complete resolution of the phimosis occurred in 76% of boys by simply stretching the prepuce daily for 3 months. Topical steroids have also been used effectively, resolving phimosis 68.2% to 95%. Circumcision is a surgical procedure removing foreskin to allow a non-covered glans. Jewish and Muslim boys undergo this procedure routinely, and >50% of US boys get circumcised at birth. Medical indications are penile malignancy, traumatic foreskin injury, recurrent attacks of severe balanoposthitis (inflammation of the glans and foreskin), and recurrent urinary tract infections.
Pedersini et al., (2017) evaluated the functional and cosmetic outcomes of “trident” preputial plasty using a modified-triple incision for surgically managing phimosis in children ages 3-15. All patients seen in a 1 year period who were unable to retract the foreskin and had posthitis or balanoposthitis or ballooning of the foreskin during urination were included and treated initially with a two-month trial of topic corticosteroids. Only the patients unresponsive to corticosteroids were treated with the "trident" preputial plasty. At 12 months post-surgery, 97.6% (all but one of the 41 subjects) of patients were able to retract the prepuce, and cosmetics and function were satisfactorily restored.
Phimosis is apparently not a highlight in medical school curriculum, and parents often seek attention for other issues that lead to the diagnosis of phimosis. Like the tight material lining the neck of a shirt, the prepuce can be given a prolonged static stretch, and, over time, may retract appropriately. Or, cutting the shirt material may be necessary for long term success. Similarly, surgical intervention such as circumcision or the newer “trident” preputial plasty may be required.
Chan, Ivy HY and Wong, Kenneth KY. (2016). Common urological problems in children: prepuce, phimosis, and buried penis. Hong Kong Medical Journal. 22(3):263–9. DOI: 10.12809/hkmj154645
Pedersini, P, Parolini, F, Bulotta, AL, Alberti, D. (2017). "Trident" preputial plasty for phimosis in childhood. Journal of Pediatric Urology. 13(3):278.e1-278.e4. doi:10.1016/j.jpurol.2017.01.024
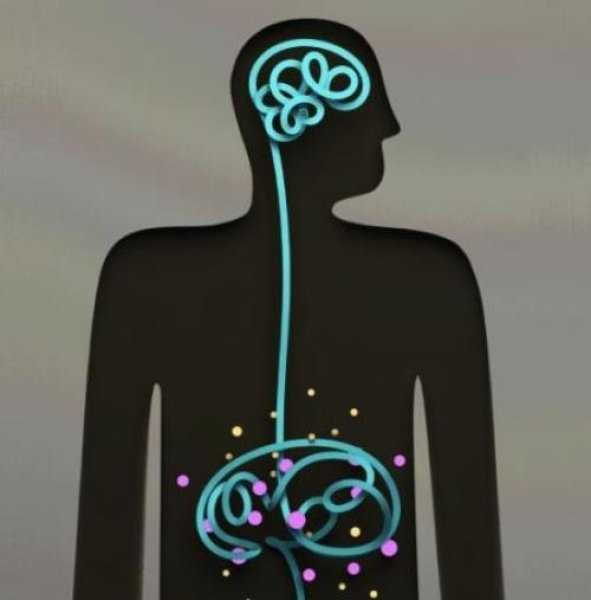
Recently I had a patient referred to me for fecal incontinence. She looked so familiar to me and we realized she had seen me before, years ago, for bladder issues. She was a sweet 60 something single woman who had raised 6 kids on her own after her husband left her. We laughed as she remembered something funny I had said back then. Then we got down to business. In recent years my patient “Inez” had been diagnosed with both diabetes and Crohn’s disease. She was managing the Crohn’s very well but her sugars were much harder for her to get under control. When I asked her about her current complaints and symptoms she reported that most days her bowels were perfect. She reported one or two soft easy to pass stools per day. But when she had to leave the house for a doctor appointment, she would have explosive diarrhea. This didn’t happen if she went to the grocery store or to visit a friend. Upon further questioning she realized she was really anxious about her diabetes and her interactions with her medical provider regarding her diabetes had not been positive. She felt frustrated, scared, and powerless. 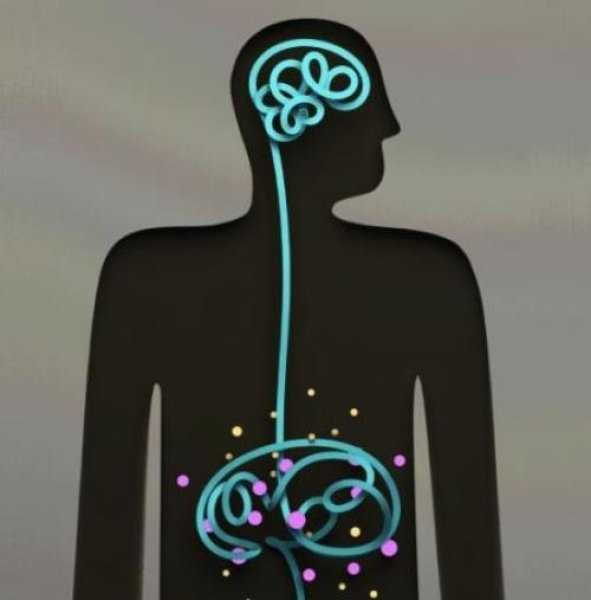
As a pelvic health PT I could have treated Inez in a variety of ways. With my initial exam I did not see any glaring musculoskeletal issues. I suggested to Inez the possibility that her nervous system was sending the wrong kind of signals to her bowels when she got anxious and that we could address this in PT. Inez agreed that she would like to try this approach. We decided that we would reevaluate after four visits to see if we needed to change the plan. Over four visits I used craniosacral therapy protocols to address nervous system upregulation and tension. I taught Inez relaxation techniques and encouraged 10 or 15 minutes of daily relaxation practice. Inez opened up about her relationship with her kids and how they tended to be takers but not givers. She would get frustrated and feel a bit used at times. We had conversations about boundaries and saying “no” and I shared some of my own experiences and struggles as well. Lastly we talked about how what we think can affect how we feel and what we do. Inez’s faith was important to her. She found a few bible verses that were meaningful to her about fear and anxiety and would repeat those during her daily relaxation time. On her fourth visit, Inez was all smiles. She brought me a jar of her homemade salsa as a graduation present. As we sat down to talk she reported to me that she saw her doctor yesterday. She had no bowel issues. And more than that, as her doctor began to talk over her she said to him, “No. Stop. You are always talking and never listening. I need you to listen to me today.” She went on to explain to him how it worried her that she was not able to control her diabetes well and she didn’t think he was doing enough to help her. Her physician did stop and listen and asked Inez, “what would you like me to do for you?” She asked for a referral to a specialist and he obliged. Inez was thrilled that she was able to manage her anxiety in a way that helped her bowels and to find the courage to confront her doctor to get the care she felt she needed.
As we grow in the knowledge of how the human body works it seems like all roads lead back to the nervous system. All of our treatments and interactions with patients affect the nervous system in one way or another. In our fast paced, stressed out world, finding ways to be intentional in addressing the nervous system can be a game changer for patients (as well as for ourselves). If this is an area you would like to grow in, please consider a new course being offered this January in Tampa, Florida. Participants taking Holistic Interventions and Meditation will experience and explore evidence-based information on strategies to address the nervous system. Topics covered include practical meditation, use of essential oils, supplements, yoga, calming and centering manual techniques and instruction in how to best dialogue with patients struggling with pain, anxiety and the effects of trauma. Nari Clemons and I hope to see you there.
Faurot, K. K. R., Gaylord, S., Palsson, O. S., Garland, E. L., Mann, J. D., & Whitehead, W. E. (2014). 715 Mindfulness Meditation Has Long-Term Therapeutic Benefits in Women With Irritable Bowel Syndrome (IBS): Follow-Up Results From a Randomized Controlled Trial. Gastroenterology, 146(5), S-124.
Kearney, D. J. (2012). Mindfulness meditation for women with irritable bowel syndrome–evidence of benefit from a randomised controlled trial. Evidence-based nursing, 15(3), 80-81.
Keefer, L., & Blanchard, E. B. (2001). The effects of relaxation response meditation on the symptoms of irritable bowel syndrome: results of a controlled treatment study. Behaviour research and therapy, 39(7), 801-811.
On my son’s due date, I ran 5 miles (as I often did during my pregnancy), hoping he would be a New Year’s baby. The thought of low bone density never crossed my mind, even living in Seattle where the sun only intermittently showers people with Vitamin D. However, bone mineral density changes do occur over the course of carrying a fetus through the finish line of birth. And sometimes women experience a relatively rare condition referred to as pregnancy-related osteoporosis.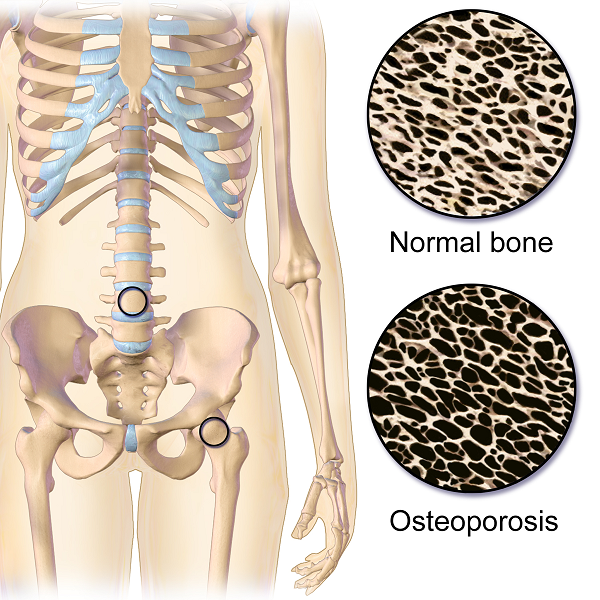
Krishnakumar, Kumar, and Kuzhimattam2016 explored vertebral compression fracture due to pregnancy-related osteoporosis (PAO). The condition was first described over 60 years ago, and risk factors include low body mass index, physical inactivity, low calcium intake, family history, and poor nutrition. Of 535 osteoporotic fractures considered, 2 were secondary to PAO. A 27-year-old woman complained of back pain during her 8th month of pregnancy, and 3 months postpartum, she was found to have a T10 compression fracture. A 31-year-old with scoliosis had back pain at 1 month postpartum but did not seek treatment until 5 months after giving birth, and she had T12, L1, and L2 compression fractures. The women were treated with the following interventions: cessation of breastfeeding, oral calcium 100 mg/day, Vitamin D 800 IU/day, alendronate 70 mg/week, and thoracolumbar orthosis. Bone density improved significantly, and no new fractures developed during the 2-year follow up period.
Nakamura et al.2015 reviewed literature on pregnancy-and-lactation-associated osteoporosis, focusing on 2 studies. The authors explained symptoms of severe low back, hip, and lower extremity joint pain that occur postpartum or in the 3rd trimester of pregnancy can be secondary to this disorder, but it is often not considered immediately. A 30-year-old woman with such debilitating pain in her spine with movement 2 months postpartum had to stop breastfeeding, and 10 months later, she was found to have 12 vertebral fractures. She had low bone mineral density (BMD) in her lumbar spine, and she was given 0.5mg/day alfacalcidol (ALF), an active vitamin D3 analog, as well as Vitamin K. No more fractures developed over the next 6 years. A 37-year-old female had severe back pain 2 months postpartum, and at 7 months was found to have 8 vertebral fractures due to PAO. Her pain subsided after stopping breastfeeding, using a lumbar brace, and supplementing with 0.5mg/day ALF and Vitamin K. The authors concluded goals for treating PAO include preventing vertebral fractures and increasing BMD and overall fracture resistance with Vitamins D and K.
Other treatment approaches for similar case presentations have been published. One gave credit to denosumab injections giving pain relief and improved BMD to 2 women, ages 35 and 33, after postpartum vertebral fractures (Sanchez, Zanchetta, & Danilowicz2016). Guardio and Fiore2016 reported success using the amino-bisphosphonates, neridronate, in a 38-year-old with PAO T4 fracture.
Thankfully for these women experiencing PAO vertebral fractures, supplements boosted their BMD and prevented further fractures. However, they all had to prematurely stop breastfeeding to reduce their pain as well. This rare condition can be used as a warning for women to proactively increase their BMD. The course, Meeks Method for Osteoporosis, can help therapists implement safe, effective, and active ways to promote bone health for all - especially the pregnant population in serious need of support.
Krishnakumar, R., Kumar, A. T., & Kuzhimattam, M. J. (2016). Spinal compression fractures due to pregnancy-associated osteoporosis. Journal of Craniovertebral Junction & Spine, 7(4), 224–227. http://doi.org/10.4103/0974-8237.193263
Nakamura, Y., Kamimura, M., Ikegami, S., Mukaiyama, K., Komatsu, M., Uchiyama, S., & Kato, H. (2015). A case series of pregnancy- and lactation-associated osteoporosis and a review of the literature. Therapeutics and Clinical Risk Management, 11, 1361–1365. http://doi.org/10.2147/TCRM.S87274
Sánchez, A., Zanchetta, M. B., & Danilowicz, K. (2016). Two cases of pregnancy- and lactation- associated osteoporosis successfully treated with denosumab. Clinical Cases in Mineral and Bone Metabolism, 13(3), 244–246. http://doi.org/10.11138/ccmbm/2016.13.3.244
Gaudio, A., & Fiore, C. E. (2016). Successful neridronate therapy in pregnancy-associated osteoporosis. Clinical Cases in Mineral and Bone Metabolism, 13(3), 241–243. http://doi.org/10.11138/ccmbm/2016.13.3.241
So many physiological changes occur to a woman’s body during pregnancy, it is no wonder that pregnant women have back and lower extremity aches and pains. These women experience hormonal changes, weight gain, reduced abdominal strength, and their center of mass shifts anteriorly. These physiological changes result in altered spinal and pelvic alignment, and increased joint laxity. Also, many women report increases in size of their feet and a tendency to have flatter arches during and after pregnancy. Alignment changes may influence pain. Altered alignment could change the physical stresses placed upon different tissues of the body, which that specific tissue was not adapted to, therefore, causing pain or injury to that tissue.
 A recent study published in 2016, in the Journal of Women’s Health Physical Therapy1, investigated if there may be a relationship between anthropometric changes of the foot that occur with pregnancy, and pregnancy related musculoskeletal pain of the lower extremity. The study included 15 primigravid women and 14 weight matched controls. This study was a repeated-measurements design study, where the investigators measured foot length, foot width, arch height index, arch rigidity index (ARI), arch drop (AD), rear foot angle, and pelvic obliquity during the second and third trimesters and post-partum. The subjects were surveyed on pain in the low back, hips/buttocks, and foot/ankle.
A recent study published in 2016, in the Journal of Women’s Health Physical Therapy1, investigated if there may be a relationship between anthropometric changes of the foot that occur with pregnancy, and pregnancy related musculoskeletal pain of the lower extremity. The study included 15 primigravid women and 14 weight matched controls. This study was a repeated-measurements design study, where the investigators measured foot length, foot width, arch height index, arch rigidity index (ARI), arch drop (AD), rear foot angle, and pelvic obliquity during the second and third trimesters and post-partum. The subjects were surveyed on pain in the low back, hips/buttocks, and foot/ankle.
The author’s findings were that measures of arch flexibility (ARI and AD) correlated with pain at the low back and the foot and ankle. They concluded that medial longitudinal arch flexibility may be related to pain in the low back and foot. The more flexible arches were associated with more pain in the study participants. They reported the participants in their study did not have very high pain levels in general, and recommend further studies to compare pregnant women who experience severe pain with women who do not while comparing their alignment factors. This article is a good reminder for physical therapists to consider the changes that occur to the foot including changes in arch height, arch flexibility, and foot size and how that influences the pelvis and lower extremity for prevention and treatment of musculoskeletal pain during pregnancy.
Educating our pregnant patients on shoe wear seems even more important now. Making recommendations, unique to each individual patient based on their objective data, foot type, and arch flexibility status seems like an appropriate addition to a well-rounded treatment plan. Doesn’t it seem prudent to wear shoes that provide some arch support to hopefully reduce musculoskeletal pain associated with pregnancy changes? I have observed some patients who are pregnant arrive to physical therapy wearing unsupportive flip flops and other poor shoe wear choices. I understand there are barriers for pregnant patients, I remember from when I was pregnant that reaching your feet to put shoes on can be very difficult, and sometimes your feet are swelling so it may be near impossible to physically get shoes on your feet. You might even need a new pair of shoes, as your shoes may no longer fit. However, an article such as this one, seems like something I could easily share with a patient to help persuade them of the importance of good shoe wear or at least proper arch support. Being able to discuss a recent scientific study with a patient can be powerful and motivating to a patient. Additionally, an article such as this reminds a practitioner of specific objective data to monitor such as arch height and flexibility as it changes throughout the patient’s pregnancy. How does the patient’s changing arch height and flexibility influence their specific pelvic, hip, knee, and ankle alignment? How does swelling play a part in the patients’ foot anthropometrics day to day, trimester to trimester? Ask more questions about their daily activities, are they ‘barefoot and pregnant’? Could something as simple as having them wear appropriate, arch supportive shoes while in the home reduce their lower extremity or back pain?"
Harrison, K. D., Mancinelli, C., Thomas, K., Meszaros, P., & McCrory, J. L. (2016). The Relationship Between Lower Extremity Alignment and Low Back, Hip, and Foot Pain During Pregnancy: A Longitudinal Study of Primigravid Women Versus Nulliparous Controls. Journal of Women’s Health Physical Therapy, 40(3), 139-146.
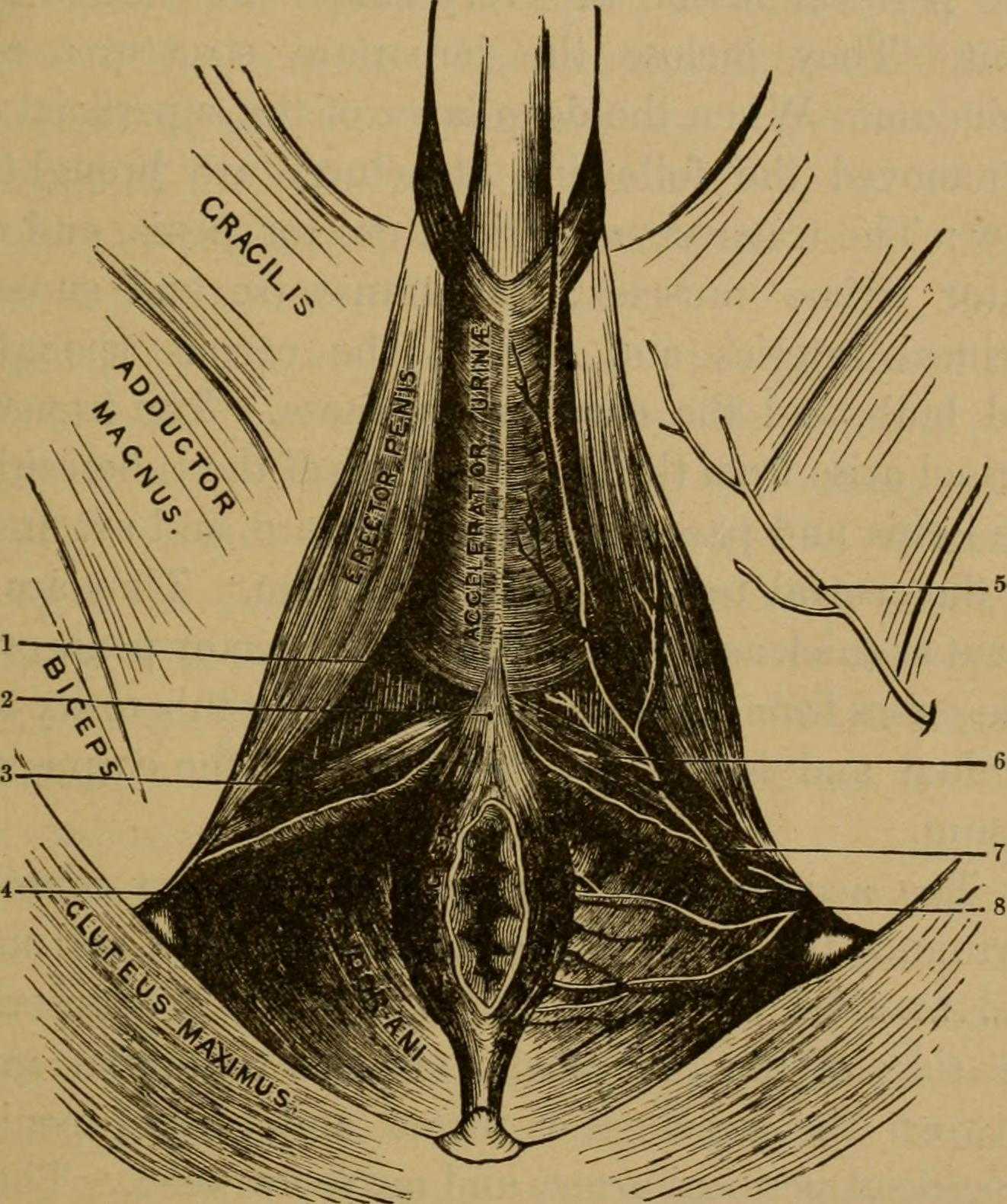 Many therapists transition to treating men with the knowledge and training from female patients. When therapists apply this knowledge, for the most part, it works. When we spend some attention on learning what is a bit different, we might be drawn to the superficial muscles of the perineum. This old anatomy image does a wonderful job of "calling it like it is" or using anatomical terms that describe an action versus naming only the structure. In the image we are looking from below (inferior view) at the perineum and genitals. Just anterior to the anus we can see the anterior muscles within the urogenital triangle, with the base of the shaft of the penis located just anterior to (above in this image) the anus and perineal body. Notice that at the midline, we see muscle names the "accelerator urine". Modern textbooks refer to this muscle as the bulbocavernosus, or bulbospongiosus. Taking the name of accelerator urine, we can understand that this muscle will have an effect on aiding the body in emptying urine. It does this through rhythmic contractions, most often noted towards the end of urination, when the typical spurts of urine follow a more steady stream. This assistance with emptying can take place because the urethra is located within the lower part of the penis, the portion known as the corpus spongiosum. Because the bulbocavernosus muscle covers this part of the penis, and the inferior and lateral parts of the urethra are virtually wrapped within the bulbocavernosus, the muscle can have an effect on emptying the urine in the urethra.
Many therapists transition to treating men with the knowledge and training from female patients. When therapists apply this knowledge, for the most part, it works. When we spend some attention on learning what is a bit different, we might be drawn to the superficial muscles of the perineum. This old anatomy image does a wonderful job of "calling it like it is" or using anatomical terms that describe an action versus naming only the structure. In the image we are looking from below (inferior view) at the perineum and genitals. Just anterior to the anus we can see the anterior muscles within the urogenital triangle, with the base of the shaft of the penis located just anterior to (above in this image) the anus and perineal body. Notice that at the midline, we see muscle names the "accelerator urine". Modern textbooks refer to this muscle as the bulbocavernosus, or bulbospongiosus. Taking the name of accelerator urine, we can understand that this muscle will have an effect on aiding the body in emptying urine. It does this through rhythmic contractions, most often noted towards the end of urination, when the typical spurts of urine follow a more steady stream. This assistance with emptying can take place because the urethra is located within the lower part of the penis, the portion known as the corpus spongiosum. Because the bulbocavernosus muscle covers this part of the penis, and the inferior and lateral parts of the urethra are virtually wrapped within the bulbocavernosus, the muscle can have an effect on emptying the urine in the urethra.
Notice that if you follow the fibers of the accelerator urine muscle towards the top of the image, where the penis continues, you will notice fibers of the muscle wrapping around the sides of the penis. These fibers will continue as a fascial band that travels over the dorsal vessels of the penis. This allows the muscle to also have a significant action during sexual activity, in which blood flow (getting blood into, keeping blood in, and letting blood out of the penis) is paramount.
On either side of the penis we can see what is labeled the erector penis. As these muscles cover the legs, or crura which form the two upper parts of the penis, when the muscles contract, blood is shunted towards the main body of the penis. This of course helps with penile rigidity, as the smooth muscles in the artery walls of the penis allow blood to fill the spongy chambers.
Once we discuss the usual functions of these muscles, we can then imagine the dysfunctions potentially created by less than optimal activity. Consider the difficulty that these muscles will create in contracting or relaxing if they are either too weak, or too tense. These issues can create difficulty emptying well the urethra, often leading to post-void dribble. Blood flow and therefore penile rigidity with erections may be negatively impacted by inability of these muscles to contract or stay contracted, and blood flow leaving the penis may be impaired if the muscles cannot relax. When we work with patients who have genital pain, pelvic floor muscle weakness, dyscoordination, or tension, we can often improve sexual function, bladder emptying, and tasks that might otherwise be affected by pain.
If you are interested in learning more about how to assess and treat these muscles, you have one more opportunity this year to attend the 3-day Male Course instructed by Holly Tanner. Holly has been teaching this course for over 10 years when she co-wrote the first course with colleague and faculty member Stacey Futterman. The course has been updated and turned into a 3-day course to include more manual therapy techniques. Hurry to grab one of the remaining spots in the October 27-29 course in Grand Rapids!
Mindful eating requires slowing down and paying attention to the present moment experience of eating. Rather than mindlessly put food into your mouth and not really taste what you’re eating, you deliberately notice the appearance, smell, texture and taste of the food and pay attention to your thoughts, feelings, and physical sensations. Eating mindfully can interrupt habitual eating behaviors and promote greater self-regulation of food choices.1 Warren and colleagues conclude mindful eating has the potential to help address maladaptive eating behaviors and the difficulties many face with controlling food intake.2
 Although mindful breathing, body scan and movement are the core skills I teach patients with persistent pain, I introduce mindful eating as another strategy to cultivate present moment awareness. Patients can have surprising shifts in their relationship to food and frequently comment, “If I ate more mindfully, I would enjoy my food more and eat less!”
Although mindful breathing, body scan and movement are the core skills I teach patients with persistent pain, I introduce mindful eating as another strategy to cultivate present moment awareness. Patients can have surprising shifts in their relationship to food and frequently comment, “If I ate more mindfully, I would enjoy my food more and eat less!”
Lucie Khadduri, PT, DPT, PRPC clinician and Adjunct Professor at the University of Puget Sound School of Physical Therapy, took my course last spring and describes her patient’s experience with mindful eating:
I have been meaning to email for some time to thank you for the April 2017 course on Mindfulness for Rehab Professionals. Your class really impacted my daily PT practice in a positive way. I wanted to share with you one story in particular to illustrate the power that these new tools you have given me have helped others.
I have this male patient who is about 35 years old who struggled with chronic constipation, bloating and anxiety related to his intense fecal urges that were then followed by an inability to defecate. When he started PT, he had just left his job and took a job working from home just so that he could have consistent, stress free bathroom access.
I spoke to him about diaphragmatic breathing and mindfulness and its impact on the autonomic nervous system. What helped him the most, though, was the mindful eating exercise. He has since started applying these concepts to when he eats. He told me on his discharge visit that in the past, he would eat 4 slices of pizza very quickly, without thinking about it and then have horrible pain afterward. Now, he says it is easy to eat 1 slice and have a salad not because he knows salad is better for him, but because his mouth and mind crave different textures and colors in his food. Mindful eating gave him the ability to slow down, focus on the physical sensations of eating and he found that this has changed his relationship with food. As a result, his constipation is much better managed and his anxiety and stress are much better.
Thanks again for an excellent class. I often encourage patients to go to your website for your free 10 minute meditations.
Thank you, Lucie, for sharing this story. It reflects one of the many ways patients benefit from training in mindful awareness. I look forward to introducing colleagues to mindful eating and additional experiential mindful exercises and current research in my upcoming class, Mindfulness-Based Pain Treatment, at Loyola University Stritch School of Medicine, Maywood, Il, September 30 and October 1.
1. Miller CK. Mindful eating with diabetes. Diabetes Spectr. 2017 May;30(2):89-94.
2. Warren JM, Smith N, Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviors: effectiveness and associated potential mechanisms. Nutr Res Rev. 2017 Jul 18:1 – 12.
Image courtesy of California Institute of Technology
At the peak of my racing career I won awards in all my races from 5k to marathon. While warming up I would scope out my competition, intimidated by muscular females wearing outfits to accentuate their physiques. Many times, appearance out-weighed running capacity. In a similar manner, one strong pelvic floor contraction produced by a female athlete does not always mean she has the endurance to stay dry in the long run.
 Brennand et al. (2017) researched urinary leakage during exercise in Canadian women. A summary of their findings concluded that skipping, trampoline, jumping jacks, and running/jogging were most likely to cause leakage. To combat the problem, 93.2% emptied their bladder just before exercise, 62.7% required voiding breaks during exercise, and 37.3% actually restricted their fluid intake to minimize leakage. While 90.3% of women who reported leakage impacted their activity just decreased their intensity, 80.7% avoided the activity entirely. Many women used pads (49.2%). Interest in pelvic floor physiotherapy to improve their UI was high (84.6%), but 63.5% of women still sought pessary or surgical management. Unfortunately, 35.6% of the women had no idea treatment was even an option.
Brennand et al. (2017) researched urinary leakage during exercise in Canadian women. A summary of their findings concluded that skipping, trampoline, jumping jacks, and running/jogging were most likely to cause leakage. To combat the problem, 93.2% emptied their bladder just before exercise, 62.7% required voiding breaks during exercise, and 37.3% actually restricted their fluid intake to minimize leakage. While 90.3% of women who reported leakage impacted their activity just decreased their intensity, 80.7% avoided the activity entirely. Many women used pads (49.2%). Interest in pelvic floor physiotherapy to improve their UI was high (84.6%), but 63.5% of women still sought pessary or surgical management. Unfortunately, 35.6% of the women had no idea treatment was even an option.
Nygaard & Shaw (2016) reviewed and summarized the cross-sectional studies regarding the association between physical activity and pelvic floor disorders. Trampolinists, especially those in the 3rd tertile of competition, even those who were nulliparous, experienced greater leakage. Competitive athletes in the highest quartile of time exercising were found to have 2.5 times the amount of urinary incontinence (UI) as the lowest inactive quartile; however, 2nd and 3rd quartile recreational athletes had no difference in UI compared to inactive women. Type and dosage of exercise were both factors in UI risk. Various studies showed habitual walking decreased UI in older women, moderate exercise decreased the risk of UI, and no exercise increased the risk of UI. The incidence of UI being related to having performed strenuous exercise early in life has been limited and variable, with one study of Norwegian athletes and US Olympians not having any greater UI later in life, while another showed middle-aged women who used to exercise 7.5 hours per week had a higher incidence of UI. This review also reported athletes had a 20% greater cross sectional area of the levator ani muscle and a greater pubovisceral muscle mean diameter; however, the pelvic floor strength recorded was lower than non-athletes.
Interestingly, Leitner et al. (2017) explored pelvic floor muscle activation for continent and incontinent females during running. For 10 seconds, EMG tripolar vaginal probe recorded activity at 7, 11, and 15km/h. No statistically significant differences between continent or incontinent subjects were found for the EMG values. Pre-activity and reflex activity mean EMG increased significantly with speed; mean pelvic floor muscle EMG activity during running was significantly above onset activation value; and, maximum voluntary contraction was exceeded 100% for all time intervals at 15km/h in women with UI. These authors suggested the stimulus of running could actually be beneficial in pelvic floor muscle training considering the reflex activity of the muscles.
At races now, I still silently survey my competition, but now I am more curious as to how many women are actually able to complete the run without leakage. The prevalence of UI among athletes continues and is becoming more of an open topic of conversation. The research as to how much and which kind of exercise correlates with UI or what activity and level of participation may be preventative for UI is growing. The need for pelvic floor therapists to treat athletes who are fit to be dry is ever increasing.
Brennand, E., Ruiz-Mirazo, E., Tang, S., Kim-Fine, S., Calgary Women’s Pelvic Health Research Group. (2017). Urinary leakage during exercise: problematic activities, adaptive behaviors, and interest in treatment for physically active Canadian women. International Urogynecology Journal. http://www.doi:10.1007/s00192-017-3409-1
Nygaard, I. E., & Shaw, J. M. (2016). Physical Activity and the Pelvic Floor. American Journal of Obstetrics and Gynecology, 214(2), 164–171. http://doi.org/10.1016/j.ajog.2015.08.067
Leitner M, Moser H, Eichelberger P, Kuhn A, Radlinger L. (2017). Evaluation of pelvic floor muscle activity during running in continent and incontinent women: An exploratory study. Neurourology and Urodynamics. 36:1570–1576. https://doi.org/10.1002/nau.23151
By accepting you will be accessing a service provided by a third-party external to https://hermanwallace.com./









































