Honestly, I have never noticed Curcumin on any of my patients’ lists of pharmaceuticals or supplements, but I will be certain to look for it now. Curcumin is the fat-soluble molecule that gives turmeric its yellow pigment, and it is best absorbed with the addition of black pepper extract. Patients often complain non-steroidal anti-inflammatory medicines (NSAIDs) tear apart their stomachs, so newer studies showing positive results with the use of an herb sound promising, even for pelvic health.
 A 2015 study by Kim et al. researched the inhibitory effect of curcumin on benign prostatic hyperplasia induced by testosterone in a rat model. Benign prostatic hyperplasia (BPH) is common among men and has a negative impact on the urinary tract of older males. Steroid 5-alpha reductase converts testosterone into dihydrotestosterone (DHT), and this increases as men age and may have negative effects on the prostate gland. Because of the side effects of conventional drugs (like finasteride) to inhibit steroid 5-alpha reductase, the authors wanted to determine if curcumin could play a protective role in BPH. They divided 8 rats into 4 groups after removal of testicles: 1) normal, 2) BPH testosterone induced subcutaneously, 3) daily curcumin (50mg/kg orally), and 4) daily finasteride (1mg/kg orally). The group receiving curcumin had significantly lower prostate weight and volume than the testosterone induced BPH group, and curcumin decreased the expression of growth factors in prostate tissue. The authors conclude curcumin may be a useful herb in inhibiting the development of BPH with fewer side effects than conventional drugs.
A 2015 study by Kim et al. researched the inhibitory effect of curcumin on benign prostatic hyperplasia induced by testosterone in a rat model. Benign prostatic hyperplasia (BPH) is common among men and has a negative impact on the urinary tract of older males. Steroid 5-alpha reductase converts testosterone into dihydrotestosterone (DHT), and this increases as men age and may have negative effects on the prostate gland. Because of the side effects of conventional drugs (like finasteride) to inhibit steroid 5-alpha reductase, the authors wanted to determine if curcumin could play a protective role in BPH. They divided 8 rats into 4 groups after removal of testicles: 1) normal, 2) BPH testosterone induced subcutaneously, 3) daily curcumin (50mg/kg orally), and 4) daily finasteride (1mg/kg orally). The group receiving curcumin had significantly lower prostate weight and volume than the testosterone induced BPH group, and curcumin decreased the expression of growth factors in prostate tissue. The authors conclude curcumin may be a useful herb in inhibiting the development of BPH with fewer side effects than conventional drugs.
In the urology realm, Cosentino et al.2016 explored the anti-inflammatory effects of a product called Killox®, a supplement with curcumin, resveratrol, N-acetylcysteine (NAC) and zinc. When benign prostatic hyperplasia (BPH) is not treated with drugs, a surgical intervention can be executed called a transurethral resection of the prostate (TURP); or, for bladder cancers, a transurethral resection of the bladder (TURB) can be performed. Either surgery generally requires administration of NSAIDs post-operatively for inflammation, urinary burning, or bladder spasms or to prevent later complications such as urethral stricture or sclerosis of the bladder neck. This open controlled trial involved Killox® tablet administration to 40 TURP patients twice a day for 20 days, to 10 TURB patients twice a day for 10 days and to 30 BPH patients who were not suited for surgical intervention once a day for 60 days. The control group received nothing for 1 week post-surgery, and 52.5% of TURP and 40% of TURB patients required NSAIDs to treat burning and inflammation the following 7 days. None of the Killox® treatment groups had post-operative or late complications except one, and none suffered epigastric pain like those using NSAIDs. The authors concluded Killox® had significant positive anti-inflammatory and analgesic effects on the patients and could be used as a safe alternative to NSAIDs by physicians.
Although “just” an herb, the use of curcumin should be supervised by a healthcare professional who understands proper dosage and any possible contraindications for a particular individual. The curcumin needs to be in a form that can be easily digested and used effectively by the body. Ultimately, it is exciting to learn about an alternative to gut-wrenching NSAIDs, making curcumin a noteworthy anti-inflammatory option for patients.
Nutrition plays an important part in patient wellness and rehabilitation. There are many reasons to consider diet when designing treatment regimens and you can learn all about them in Megan Pribyl's Nutrition Perspectives for the Pelvic Rehab Therapist course. Your next chance to take this course is March 31 - April 1, 2017 in White Plains, NY. Don't miss out!
Kim, S. K., Seok, H., Park, H. J., Jeon, H. S., Kang, S. W., Lee, B.-C., … Chung, J.-H. (2015). Inhibitory effect of curcumin on testosterone induced benign prostatic hyperplasia rat model. BMC Complementary and Alternative Medicine,15, 380. http://doi.org/10.1186/s12906-015-0825-y
Cosentino, V., Fratter, A., Cosentino M. (2016). Anti-inflammatory effects exerted by Killox®, an innovative formulation of food supplement with curcumin, in urology. Eur Rev Med Pharmacol Sci. 20: 7, 1390-1398. http://www.ncbi.nlm.nih.gov/pubmed/27097964#
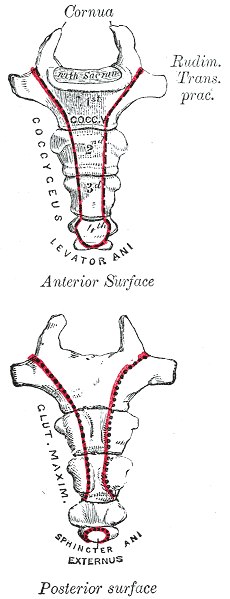
In my mid 20’s I had a sudden onset of severe, persistent pain at the bottom of my spine. I had fallen while running on trails and thought maybe I had fractured my coccyx. It hurt terribly to sit, especially on hard surfaces. When I finally succumbed to seeing a doctor, he diagnosed me with a pilonidal cyst and performed a simple excision of the infection right there in the office. I recall passing out on the table and waking up with an open wound stuffed with gauze. What I thought was “just” coccydynia turned out to be something completely different, requiring a specific and immediately effective treatment.
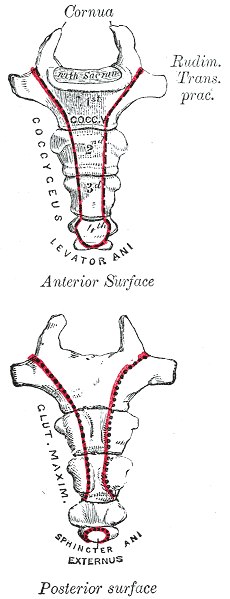 Differential diagnosis is essential in all medical professions. Blocker, Hill, and Woodacre2011 presented a case report on persistent coccydynia and the necessity of differential diagnosis. A 59-year old female reported constant coccyx pain after falling at a wedding. Her initial x-rays were normal, as was an MRI a year later, despite continued pain. Neither an ultrasound nor abdominal CT scan was performed until 16 months after the onset of pain, which was 2 months after she started having bladder symptoms. A CT scan then showed a tumor stemming from her sacrum and coccyx, and an MRI confirmed the sacrum as the tumor location. Chordomas are primary bone tumors generally found at the sacrum and coccyx or the base of the skull. They are relatively rare; however, they do exist in males and females and can present as low back pain, a soft tissue mass, or bladder/bowel obstruction. Clinicians need to listen for red flags of night pain and severe, unrelenting pain and ensure proper examination is performed for accurate diagnosis and expedient treatment.
Differential diagnosis is essential in all medical professions. Blocker, Hill, and Woodacre2011 presented a case report on persistent coccydynia and the necessity of differential diagnosis. A 59-year old female reported constant coccyx pain after falling at a wedding. Her initial x-rays were normal, as was an MRI a year later, despite continued pain. Neither an ultrasound nor abdominal CT scan was performed until 16 months after the onset of pain, which was 2 months after she started having bladder symptoms. A CT scan then showed a tumor stemming from her sacrum and coccyx, and an MRI confirmed the sacrum as the tumor location. Chordomas are primary bone tumors generally found at the sacrum and coccyx or the base of the skull. They are relatively rare; however, they do exist in males and females and can present as low back pain, a soft tissue mass, or bladder/bowel obstruction. Clinicians need to listen for red flags of night pain and severe, unrelenting pain and ensure proper examination is performed for accurate diagnosis and expedient treatment.
In a more recent case study by Gavriilidid & Kyriakou 2013, a 73 year old male presented with 6 months of tailbone pain, worse with sitting and rising from sitting. The physician initially referred him to a surgeon for a pilonidal cyst he diagnosed upon palpation. The surgeon found an unusual mass and performed a biopsy, which turned out to be a sacrococcygeal chordoma. The tumor was excised surgically along with the gluteal musculature, coccyx, and the fifth sacral vertebra, as well as a 2cm border of healthy tissue to minimize risk of recurrence of the chordoma. These authors reported coccygodynia is most often caused by pilonidal disease, clinically confirmed by abscess/sinus, fluid drainage, and midline skin pits. They concluded from this case study if one or more of those characteristic findings are absent, differential diagnoses of chordoma, perineural cyst, giant cell tumour, intra-osseous lipoma, or intradural Schwannoma should be investigated.
Honestly, if I were not a physical therapy tech when my coccyx started killing me 20 years ago, I am not sure I would have gone to the doctor right away. My boss called me out when I winced every time I sat down, and he sent me off to get an exam. The majority of patients are not blurting out specific details about buttock pain when they come for evaluation. Modesty prevails but does not always benefit a patient with persistent coccydynia. Thankfully I did not have a chordoma, but the pain was intense enough to bring me to tears, and it could have required surgery if I had not been diagnosed early enough. Providing a comfortable environment for our patients during their initial encounter can help them feel less vulnerable and discuss the root of their pain. If we can decipher between chordoma and other causes of coccydynia, we may strike a chord that saves a patient from a poor outcome.
The Herman & Wallace course "Coccyx Pain Evaluation & Treatment" is an excellent opportunity to learn new differential diagnosis techniques for coccyx pain patients. The next opportunity to attend this course is March 25-26 in Tampa, Florida.
Blocker, O., Hill, S., & Woodacre, T. (2011). Persistent coccydynia – the importance of a differential diagnosis. BMJ Case Reports, 2011, bcr0620114408. http://doi.org/10.1136/bcr.06.2011.4408
Gavriilidis, P., & Kyriakou, D. (2013). Sacrococcygeal chordoma, a rare cause of coccygodynia. The American Journal of Case Reports, 14, 548–550. http://doi.org/10.12659/AJCR.889688
In the world of pelvic health, we are constantly meeting patients who are surprised to learn about the scope of what we do. Oftentimes, it is because we mention the pelvic muscles’ roles in sexual health that a patient will offer up symptoms with their sexual health, or ask a few more questions. Outside of pelvic health professionals asking about sexual function, do men bring up these issues with anyone? Not usually. In Fisher and colleagues 2-part “Strike up a conversation” study (2005), the authors reported that men who have erectile dysfunction (ED) are worried about their partner’s reaction, don’t want to admit to having a chronic problem, and frankly, just don’t even know where to start. Unfortunately, the partners of men who have ED have the same concerns. In addition, partners are worried about bringing it up and “making their partners feel worse about it.” When men did bring up sexual concerns with their physician, although they reported feeling nervous and embarrassed, they also reported feeling hopeful and relieved.
 This issue was highlighted in a recent interview and article published on National Public Radio. The article shares that for war veterans, sexual intimacy is often affected, and yet, is often ignored. A Marine who suffered PTSD after a head injury and shrapnel to the head and neck describes how he had to go to the doctor several times just to work up the nerve to ask for help for his sexual dysfunction. He also shared how it was difficult to talk about “…because it contradicts a self-image so many Marines have.” Apparently you don’t have to be a Marine to feel the same intense pressure related to talking about sexual issues. I have spent more time in the past year trying to better understand why men don’t discuss these issues, with a best friend or partner, and each time, my question of “what would that be like if you brought it up?” is met with near bewilderment, as if revealing this issue were akin to revealing your deepest, darkest secret. Apparently, it is. Telling a buddy you have erectile dysfunction, for men, seems to be like showing your enemy where the chink in your armor is, or like setting yourself up to be the center of every “getting it up” joke for the remainder of your life.
This issue was highlighted in a recent interview and article published on National Public Radio. The article shares that for war veterans, sexual intimacy is often affected, and yet, is often ignored. A Marine who suffered PTSD after a head injury and shrapnel to the head and neck describes how he had to go to the doctor several times just to work up the nerve to ask for help for his sexual dysfunction. He also shared how it was difficult to talk about “…because it contradicts a self-image so many Marines have.” Apparently you don’t have to be a Marine to feel the same intense pressure related to talking about sexual issues. I have spent more time in the past year trying to better understand why men don’t discuss these issues, with a best friend or partner, and each time, my question of “what would that be like if you brought it up?” is met with near bewilderment, as if revealing this issue were akin to revealing your deepest, darkest secret. Apparently, it is. Telling a buddy you have erectile dysfunction, for men, seems to be like showing your enemy where the chink in your armor is, or like setting yourself up to be the center of every “getting it up” joke for the remainder of your life.
The bottom line is that we can be part of the solution to this problem, because men must be certain that their medical provider knows about any emerging or worsening erectile dysfunction. Loss of libido, or changes in erectile function can be associated with heart issues, with diabetes, or with other major medical concerns. Research such as the referenced “strike up a conversation study” has demonstrated that health care providers or partners may positively influence a patient’s access to care. Once medical evaluation has been completed, the role of the pelvic health provider is critical in improving sexual health for men with dysfunction. If you are interested in learning more about the role of the pelvic health provider for erectile dysfunction or pain related to sexual function, the Male Pelvic Health continuing education course will be offered 3 times this year through the Herman & Wallace Pelvic Rehabilitation Institute. Your next opportunity to learn about urinary and prostate conditions, male pelvic pain, sexual health and dysfunction is next month in Portland, Oregon.
Chang, A. (2016). For veterans, trauma of war can persist in struggles with sexual intimacy. Retrieved from http://www.npr.org/sections/health-shots/2017/01/01/507749611/for-veterans-trauma-of-war-can-persist-in-struggles-with-sexual-intimacy
Fisher, W. A., Meryn, S., Sand, M., Brandenburg, U., Buvat, J., Mendive, J., ... & Strike Up a Conversation Study Team. (2005). Communication about erectile dysfunction among men with ED, partners of men with ED, and physicians: The Strike Up a Conversation Study (Part I). The journal of men's health & gender, 2(1), 64-78.
Fisher, W. A., Meryn, S., Sand, M., & Strike up a Conversation Study Team. (2005). Communication about erectile dysfunction among men with ED, partners of men with ED, and physicians: the Strike Up a Conversation study (Part II). The journal of men's health & gender, 2(3), 309-e1.
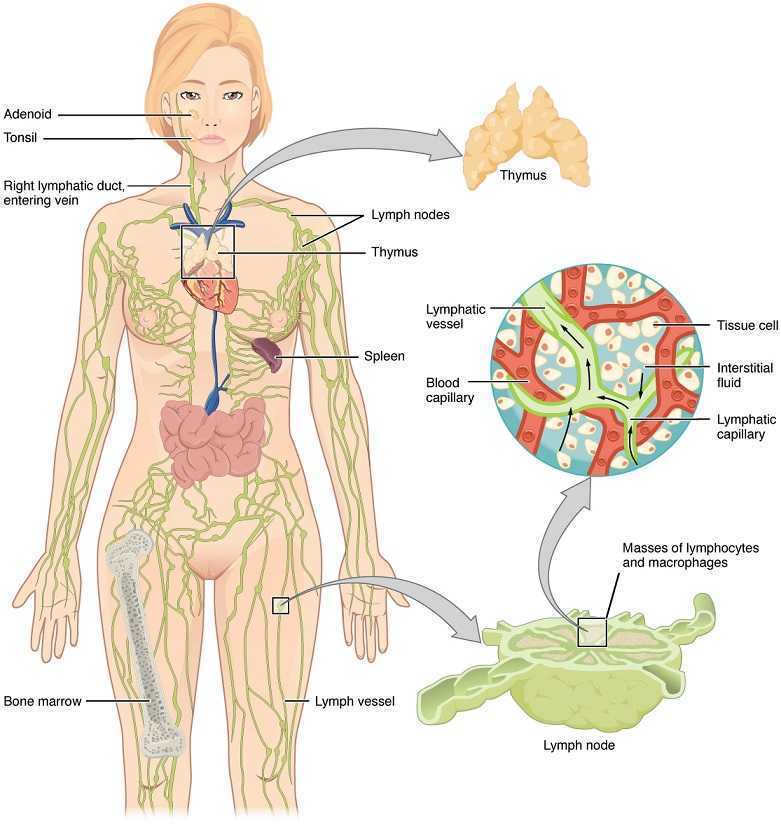
Lymphedema with regards to women’s health is most commonly associated with breast cancer. Upper extremity lymphedema can be limiting and painful without a doubt, and I have seen women suffering from irritating edema and limited shoulder range of motion and function after radical mastectomy. However, we may not always consider lower extremity lymphedema which can occur as a result of urogenital cancers and their treatments. Our knowledge and skilled hands can impact the quality of life of these patients who may seek treatment for their post-cancer complications.
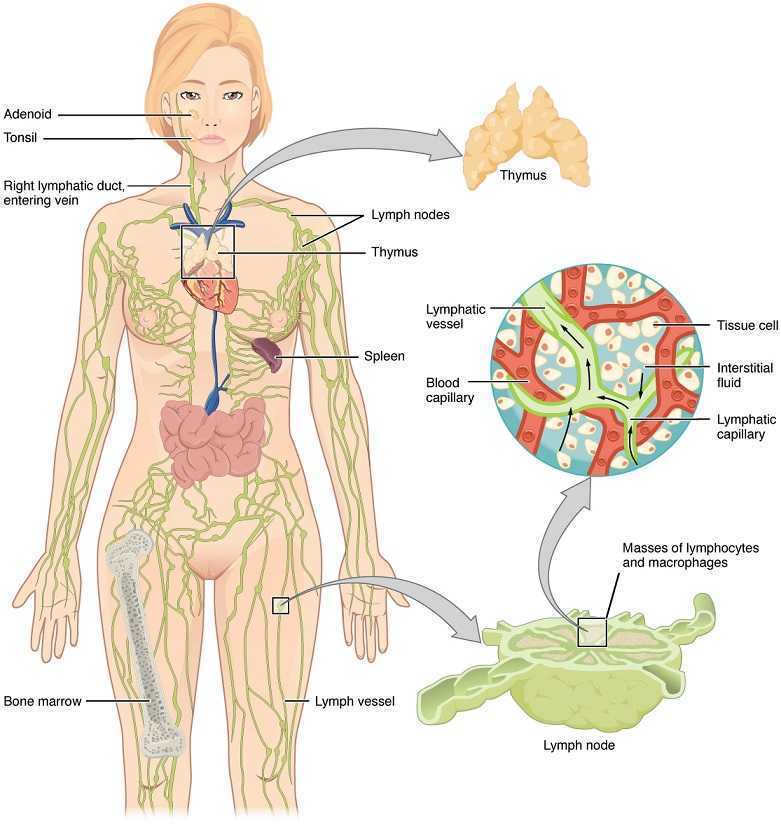 Mitra et al., published a 2016 retrospective study on lymphedema risk post radiation therapy in endometrial cancer. They considered 212 endometrial cancer survivors, and 7.1% who received adjuvant pelvic radiation therapy developed lower extremity lymphedema after treatment, whether they had chemotherapy or not. Finding at least 1 positive pathological lymph node was directly correlated with an increased risk of lymphedema, regardless of attempts to control pelvic lymph-node dissection. These statistics encourage finding prophylactic measures to take for stage III endometrial cancer patients to minimize the risk for long-term lymphedema. Regarding treatment for lower extremity lymphedema, this paper discussed compression stocking use, pneumatic compression stockings, and complex decongestive therapy, an intensive regimen of physical therapy and massage that is unfortunately not easily accessible for a majority of patients. The authors encouraged future research on the efficacy of exercise and compression for lymph node positive patients.
Mitra et al., published a 2016 retrospective study on lymphedema risk post radiation therapy in endometrial cancer. They considered 212 endometrial cancer survivors, and 7.1% who received adjuvant pelvic radiation therapy developed lower extremity lymphedema after treatment, whether they had chemotherapy or not. Finding at least 1 positive pathological lymph node was directly correlated with an increased risk of lymphedema, regardless of attempts to control pelvic lymph-node dissection. These statistics encourage finding prophylactic measures to take for stage III endometrial cancer patients to minimize the risk for long-term lymphedema. Regarding treatment for lower extremity lymphedema, this paper discussed compression stocking use, pneumatic compression stockings, and complex decongestive therapy, an intensive regimen of physical therapy and massage that is unfortunately not easily accessible for a majority of patients. The authors encouraged future research on the efficacy of exercise and compression for lymph node positive patients.
Shaitelman et al. presented a review of the progress made in the treatment and prevention of cancer-related lymphedema (2015). They stated gynecologic cancer treatment is associated with 25% incidence of lymphedema. Endometrial cancer had 1%, cervical cancer had 27%, and vulvar cancer had 30% incidence specifically. Sentinel lymph node biopsy (SLNB) can be an important part of cancer treatment, as lymphedema incidence was shown to average 9%. With treatment of genitourinary cancers, lymphedema occurred in 4% patients with prostate cancer, 16% patients with bladder cancer, and 21% patients with penile cancer. Shown to decrease limb volume and improve quality of life, the current standard of care is complete decongestive therapy (CDT). These authors state CDT involves the use of manual lymphatic drainage (MLD), bandaging on a daily basis, skin care, exercise, and a 3-phase protocol of compression. The use of SLNB helps identify the risk of lymphedema post cancer treatment; however, clinicians need to be aware of the signs and symptoms of lymphedema so the affected patient can be recognized early and referred to the appropriate specialist for treatment.
We may be referred patients with the confirmed diagnosis of lymphedema, but often we see post-cancer patients for rehab who develop lymphedema months after radiation or chemotherapy. Any healthcare professional involved with regular treatment of a cancer-surviving patient needs to have a keen sense for diagnosing and properly taking care of lymphedema. Courses such as “Lymphatics and Pelvic Pain: New Strategies” can open a whole new avenue for understanding what patients may need from us following urogenital and genitourinary cancers. Why not be prepared to face with knowledge and skill whatever pathology our patients present?
Mitra, D., Catalano, P.J., Cimbak, N., Damato, A.L., Muto, M.G., & Viswanathan, A.N. (2016). The Risk of Lymphedema After Postoperative Radiation Therapy in Endometrial Cancer. Journal of Gynecologic Oncology, 27(1), e4.
Shaitelman, S.F., Cromwell, K.D., Rasmussen, J.C., Stout, N.L., Armer, J.M., Lasinski, B.B., & Cormier, J.N. (2015). Recent Progress in Cancer-Related Lymphedema Treatment and Prevention. CA: A Cancer Journal for Clinicians, 65(1), 55-81.
During labor, I had no problem breathing out. My hang up came when I had to inhale - actually oxygenate my blood and maintain a healthy heart rate for my almost newborn baby. When extra staff filled the delivery room, and an oxygen mask was placed over my face, my husband remained calm but later told me how freaked out he was. He was watching the monitors that showed a drop in my vitals as well as our baby’s. In retrospect, I wonder if practicing yoga, particularly the breathing techniques involved with pranayama practice, could have prevented that moment.
 A research article by Critchley et al., (2015) broke down breathing to a very scientific level, determining the consequences of slow breathing (6 breaths/minute) versus induced hypoxic challenges (13% inspired O2) on the cardiac and respiratory systems and their central neural substrates. Functional magnetic resonance imaging measured the 20 healthy subjects’ specific brain activity during the slow and normal rate breathing. The authors mentioned the controlled slow breathing of 6 breaths/minute is the rate encouraged during yoga practice. This rate decreases sympathetic activity, lessening vasoconstriction associated with hypertension, and it prevents physiological stress from affecting the cardiovascular system. Each part of the brain showed responses to the 2 conditions, and the general conclusion was modifying breathing rate impacted autonomic activity and improved both cardiovascular and psychological health.
A research article by Critchley et al., (2015) broke down breathing to a very scientific level, determining the consequences of slow breathing (6 breaths/minute) versus induced hypoxic challenges (13% inspired O2) on the cardiac and respiratory systems and their central neural substrates. Functional magnetic resonance imaging measured the 20 healthy subjects’ specific brain activity during the slow and normal rate breathing. The authors mentioned the controlled slow breathing of 6 breaths/minute is the rate encouraged during yoga practice. This rate decreases sympathetic activity, lessening vasoconstriction associated with hypertension, and it prevents physiological stress from affecting the cardiovascular system. Each part of the brain showed responses to the 2 conditions, and the general conclusion was modifying breathing rate impacted autonomic activity and improved both cardiovascular and psychological health.
Vinay, Venkatesh, and Ambarish (2016) presented a study on the effect of 1 month of yoga practice on heart rate variability in 32 males who completed the protocol. The authors reported yoga is supposed to alter the autonomic system and promote improvements in cardiovascular health. Not just the breathing but also the movements and meditation positively affect mental health and general well-being. The subjects participated in 1 hour of yoga daily for 1 month, and at the end of the study, the 1 bpm improvement in heart rate was not statistically significant. However, heart rate variability measures indicated a positive shift of the autonomic system from sympathetic activity to parasympathetic, which reduces cortisol levels, improves blood pressure, and increases circulation to the intestines.
Bershadsky et al., (2014) studied the effect of prenatal Hatha yoga on cortisol levels, affect and depression in the 34 women who completed pre, mid, and post pregnancy saliva tests and questionnaires. While levels of cortisol increase naturally with pregnancy, yoga was found to minimize the mean levels compared to the days the subjects did not participate in yoga. After a single 90-minute yoga session, during which breathing was emphasized throughout the session, women had higher positive affect; but, the cortisol level was not significantly different from the control group. Overall, the authors concluded yoga had potential to minimize depression and cortisol levels in pregnancy.
Considering the positive effect of slow breathing practiced in yoga, the positive shift in the autonomic nervous system function and the decrease in cortisol levels, yoga is gaining credibility as an effective adjunct to treatment during pregnancy. If a woman enters the delivery room with a solid practice of slow breathing under her belt, she may be equipped to handle the intensity of contractions and the pain of pushing a little better. Yoga may help a woman breathe for her life and her baby’s as well.
If you're interested in learning more about yoga for pregnant patients, consider attending Yoga as Medicine for Pregnancy with Ginger Garner, PT, DPT, ATC/LAT, PYT. The next opportunity is in Fort Lauderdale, FL on January 28th and 29th, 2017. Don't miss out!
Critchley, H. D., Nicotra, A., Chiesa, P. A., Nagai, Y., Gray, M. A., Minati, L., & Bernardi, L. (2015). Slow Breathing and Hypoxic Challenge: Cardiorespiratory Consequences and Their Central Neural Substrates. PLoS ONE, 10(5), e0127082.
Vinay, A., Venkatesh, D., & Ambarish, V. (2016). Impact of short-term practice of yoga on heart rate variability. International Journal of Yoga, 9(1), 62–66.
Bershadsky, S., Trumpfheller, L., Kimble, H. B., Pipaloff, D., & Yim, I. S. (2014). The effect of prenatal Hatha yoga on affect, cortisol and depressive symptoms. Complementary Therapies in Clinical Practice, 20(2), 106–113.
Myofascial release (MFR) can be one of your greatest treatment tools as a pelvic rehabilitation practitioner. Just in case you don’t think about fascia often here are a couple helpful things to remember. Fascia is the irregular connective tissue that covers the entire body, and it is the largest sensory system in the body, making it highly innervated. The mobilizing effect of MFR techniques occurs by stimulating various mechanoreceptors within the fascia (not by the actual force applied). MFR techniques can help to reduce tissue tension, relax hypertonic muscles, decrease pain, reduce localized edema, and improve circulation just to name a few physiological effects.
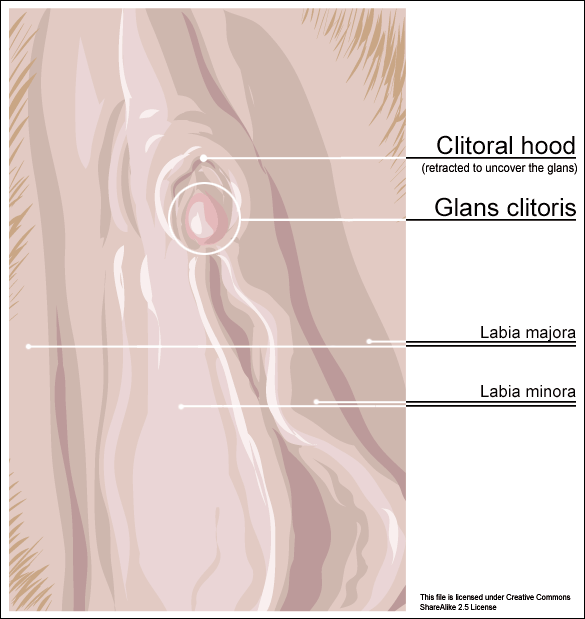
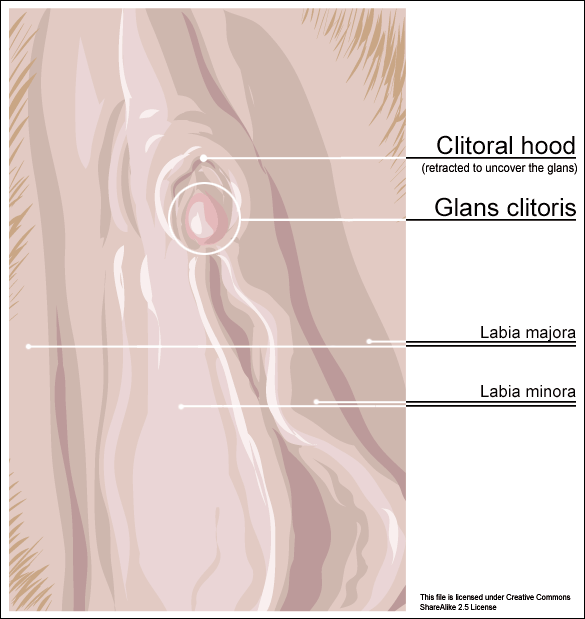 An interesting case report published in 2015 by the Journal of Women’s Health Physical Therapy1 offers a wonderful example of how a physical therapist used specific MFR techniques for a patient with clitoral phimosis and dyspareunia. The specific MFR techniques used helped to provide relief and restore mobility to the pelvic tissues for this patient.
An interesting case report published in 2015 by the Journal of Women’s Health Physical Therapy1 offers a wonderful example of how a physical therapist used specific MFR techniques for a patient with clitoral phimosis and dyspareunia. The specific MFR techniques used helped to provide relief and restore mobility to the pelvic tissues for this patient.
Clitoral phimosis is adherence between the clitoral prepuce (also known as the clitoral hood) and the glans. This condition can be the result of blunt trauma, chronic infection, inflammatory dermatoses, and poor hygiene. In this case report, the 41-year-old female patient had sustained a blunt trauma injury to the vulva (when her toddler son charged, contacting his head forcibly into her pubic region). She presented to physical therapy with complaints of dyspareunia, low back pain, a bruised sensation of her pubic region, vulvar pain provoked by sexual arousal, decreased clitoral sensitivity, and anorgasmia. The physical therapist completed an orthopedic assessment for the lower quarter (including spine and extremities), as well as a thorough pelvic floor muscle assessment.
Treatment for this patient addressed not only the pelvic complaints, but the lower quarter complaints as well. A detailed treatment summary for each visit is outlined in the case report. The clitoral MFR and stretching was performed by applying a small amount of topical lubricant to the clitoral prepuce. Then, a gloved finger or a cotton swab was used to stabilize the clitoris, a prolonged MFR or sustained stretch was applied in the direction away from the fixated clitoris by the therapist’s other finger. The therapist applied this technique along the entire length of the prepuce. The other physical therapy interventions this patient was treated with were stretching, joint mobilization, muscle energy techniques, transvaginal pelvic floor muscle massage, clitoral prepuce MFR techniques, biofeedback, Integrative Manual Therapy (IMT) techniques, nerve mobilization, and therapeutic and motor control exercises. Additionally, between the physical therapy evaluation and the second visit the patient did use topical Clobetasol 0.05% cream (commonly prescribed for vulvar dermatitis issues such as Lichen Sclerosis) for 30 days with no change to her clitoral phimosis.
After 11 sessions, the patient had resolution of dyspareunia, vulvar pain, pubic pain, and reduced low back pain. Also, the patient had 100% restored mobility of the clitoral prepuce, as well as normalized clitoral sensitivity and clitoral orgasm. The patient felt these improvements were still present at her 6-month follow-up interview over the phone. Current medical management for clitoral phimosis is surgical release or topical/injectable corticosteroids. Having a conservative treatment option, such as MFR, for this condition can be helpful for patients. As with most evolving treatment techniques, more research and studies are appropriate.
Not one health care professional had ever assessed the fascial mobility of the clitoris until this physical therapist did. This case report is an example of how MFR techniques can be effective treatment tools for your patients with pelvic disorders and a good reminder to check the fascial mobility of the pelvic tissues.
Morrison, P., Spadt, S. K., & Goldstein, A. (2015). The Use of Specific Myofascial Release Techniques by a Physical Therapist to Treat Clitoral Phimosis and Dyspareunia. Journal of Women’s Health Physical Therapy, 39(1), 17-28.
One of my dear patients was recently diagnosed with Ehlers-Danlos sydrome (EDS). The diagnosis brought a sense of relief for sweet Katie who for years struggled with numerous health problems and was often misunderstood and under cared for by the medical community. Katie was referred to me 2 years ago at 28 for pelvic pain, endometriosis and IC. Upon exam we also discovered a significant elimination disorder and paradoxical elimination. Katie regularly timed her elimination and was spending at times up to 2 hours trying to empty her bowels. As we worked together we uncovered bilateral hip dysplasia, left hip labral tear, ilioinguinal and pudendal neruralgia and POTS (Postural Orthostatic Hypotension Syndrome). Katie already had a history of anxiety and depression but managed well with good family and friend support. When the diagnosis of EDS came, she finally felt like she had an explanation for why her body is like it is. This brought great relief as well as the knowledge that her condition was genetic and her conditions needed to be managed as best as possible to give her the most function, but would likely never be fully resolved.
 In her book "A Guide to Living with Ehler's Danlos Syndrome" Isobel Knight does a beautiful job outlining the various genetic subtypes of Ehlers Danlos but also highlighting the fact that EDS hypermobility type (Type III) does not just affect the connective tissue in the musculoskeletal sytem leading to joint instability and hypermoblity, muscle tears, dislocations, subluxations, hip dysplasia and flat feet. EDS can also affect the body's systemic collagen leading to increased risk for endometriosis, POTS, Renauds, bladder problems, fibromyalgia, headaches, restless legs, ashtma, consitpation, bloatedness, prolapse, IBS symptoms, anxiety, depression and learning difficulties. She notes that some people have only a few of these systemic symptoms while others may be more affected. Per Isobel: "it is important that all symptoms are treated seriously and not ridiculed and that the appropriate medical support is given to them when necessary."
In her book "A Guide to Living with Ehler's Danlos Syndrome" Isobel Knight does a beautiful job outlining the various genetic subtypes of Ehlers Danlos but also highlighting the fact that EDS hypermobility type (Type III) does not just affect the connective tissue in the musculoskeletal sytem leading to joint instability and hypermoblity, muscle tears, dislocations, subluxations, hip dysplasia and flat feet. EDS can also affect the body's systemic collagen leading to increased risk for endometriosis, POTS, Renauds, bladder problems, fibromyalgia, headaches, restless legs, ashtma, consitpation, bloatedness, prolapse, IBS symptoms, anxiety, depression and learning difficulties. She notes that some people have only a few of these systemic symptoms while others may be more affected. Per Isobel: "it is important that all symptoms are treated seriously and not ridiculed and that the appropriate medical support is given to them when necessary."
It seems that EDS is becoming more widely recognized. As rehabilitation specialists we should be alert to problems stemming from joint hypermobility when we notice how our patients position themselves. Often legs are curled up or double crossed. Upon questioning we might find that the patient has a history of being "double jointed" or was able to do "party tricks" with their bodies. The Bighton scale is a test of joint hypermobility which we should all be familiar with. It is also important to note that a patient may have hypermobility without having EDS, and that EDS is usually associated with pain. A rheumatologist, or in Katie's case a geneticist, can help confirm a suspected EDS diagnosis.
If you have a patient with hypermobliiy or with EDS, know that their ability to know where their body is in space is limited as their joints have much more range of motion than normal. The proprioceptors do not fire well at mid range and the patient will have to be trained to become accustomed to neutral joint positions. This was really painful for Katie and it took a huge mental and physical effort. She is getting stronger now and it is becoming easier to achieve. Stretching and soft tissue massage can feel really good when your muscles have to work so hard to maintain your joints in healthy positions. Patients should be instructed to not stretch into end range and also not "hang out" on their ligaments. Some patients may have to begin just with isometrics. I used Sara Meeks' program for safe and effective floor exercise with Katie. The floor gave her support while she strengthened her core muscles. Then she was able to progress to seated and seated on a ball as well as standing exercises. She loves the body blade! Yoga, Pilates, exercise in water can be effective for strength, propriception and movement reeducation. Mirrors are helpful for increasing position sense.
It is also helpful to note that even patients with EDS may be hypermobile in some joints and hypomobile in others. Isobel reports that her SI joints were extremely unstable while her thoracic spine was very rigid to the point that her lung capacity was affected. Having her therapist work on the hypomobility and doing breath work was life changing.
As pelvic health therapists and rehabilitation providers we may be the first professional to suspect EDS in a patient. There is a great deal that we and the greater medical and holistic community can do to help patients with EDS lead lives with less pain and dysfunction.
In the 80’s, I would stand in my older sister’s bedroom wearing a button-down, collared shirt under a sweater and beg her to “fix me.” I felt stuck and wanted to cry until she twisted the shirt and loosened the snags of the knitted covering and made the outfit lay properly together. The myofascial system can often make us feel the same way if what’s lying underneath the intricately woven network of tissue has trigger points and inflammatory mediators rearing their ugly heads. When myofascial restrictions strike the pelvic region, every move a person makes can tug at the affected fascia and magnify the pain.
 How do we know if someone has myofascial pain syndrome? Itza et al., (2015) published a study on turns-amplitude analysis (TAA) efficacy for diagnosing the syndrome in patients with chronic pelvic pain. The 128 subjects (64 with chronic pelvic pain and 64 healthy controls) underwent electromyogram (EMG) tests conducted in the levator ani muscle and the external anal sphincter. The mean TAA data was analyzed automatically, and an increase in the score was considered to be positive, while a decrease was negative. An increased TAA was found in 86% of the patients (no difference between men and women), and 100% of the control subjects displayed no increase in TAA. This study showed TAA to be an effective means by which to diagnose myofascial pain syndrome of the pelvic floor.
How do we know if someone has myofascial pain syndrome? Itza et al., (2015) published a study on turns-amplitude analysis (TAA) efficacy for diagnosing the syndrome in patients with chronic pelvic pain. The 128 subjects (64 with chronic pelvic pain and 64 healthy controls) underwent electromyogram (EMG) tests conducted in the levator ani muscle and the external anal sphincter. The mean TAA data was analyzed automatically, and an increase in the score was considered to be positive, while a decrease was negative. An increased TAA was found in 86% of the patients (no difference between men and women), and 100% of the control subjects displayed no increase in TAA. This study showed TAA to be an effective means by which to diagnose myofascial pain syndrome of the pelvic floor.
What are some treatments being researched? Anderson et al., (2016) conducted a study on using a multi-modal protocol with an internal myofascial trigger point wand to treat men and women with chronic pelvic pain syndrome (CPPS). After 6 days of training, male and female subjects with CPPS engaged in 6 months of pelvic floor trigger point release with an internal trigger point device that was self-administered in combination with paradoxical relaxation training. In the end, women and men subjects experienced similar reduction of symptoms as trigger point sensitivity decreased significantly.
Adelowo et al., (2013) explored the efficacy of botulinum toxin type A (Botox) for treatment of myofascial pelvic pain via a retrospective cohort study. Trigger points and pelvic floor hypertonicity were identified and confirmed with digital palpation. Twenty-nine women were assessed after intralevator injection with Botox A, and 79.3% reported reduction of pain. Botox A was deemed an effective and safe intervention with only mild, spontaneously resolving side effects occurring in 8 of the patients.
In 2012, Fitzgerald et al. studied the difference in outcomes between myofascial physical therapy (MPT) versus global therapeutic massage (GTM) for patients with interstitial cystitis/painful bladder syndrome. Of the 81 women randomly allocated to the two treatment groups, the MPT group had the greater response with 59% reporting moderate or marked improvement in symptoms (compared to 26% in the GTM group). Ultimately, myofascial physical therapy was considered beneficial for pelvic disorders.
Being able to adjust an outward snag such as a twisted sweater or stocking is much less complicated than deciphering and untangling the internal myofascial dysfunctions in the pelvis. When you are without an EMG, high-tech internal wands, or Botox, it is up to your hands and keen sensibility to detect the presence of the trigger points and release the restrictions. Thankfully, courses like “Mobilization of the Myofascial Layer: Pelvis and Lower Extremity” can guide you towards greater efficacy in this endeavor.
Itza, F., Zarza, D., Salinas, J., Teba, F., & Ximenez, C. (2015). Turn-amplitude analysis as a diagnostic test for myofascial syndrome in patients with chronic pelvic pain. Pain Research & Management : The Journal of the Canadian Pain Society, 20(2), 96–100.
Anderson, R.U., Wise, D., Sawyer, T. et al. (2016). Equal Improvement in Men and Women in the Treatment of Urologic Chronic Pelvic Pain Syndrome Using a Multi-modal Protocol with an Internal Myofascial Trigger Point Wand. Applied Psychophysiology Biofeedback. 41:215.
ADELOWO, A., HACKER, M. R., SHAPIRO, A., Modest, A. M., & ELKADRY, E. (2013). Botulinum Toxin Type A (BOTOX) for Refractory Myofascial Pelvic Pain. Female Pelvic Medicine & Reconstructive Surgery, 19(5), 288–292.
FitzGerald, M., Payne, C., Lukacz, E., Yang, C., Peters, K., Chai, T., … Nyberg, *LM. (2012). Randomized Multicenter Clinical Trial of Myofascial Physical Therapy in Women with Interstitial Cystitis/Painful Bladder Syndrome (IC/PBS) and Pelvic Floor Tenderness. The Journal of Urology, 187(6), 2113–2118.
Faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC has written in to encourage us all to practice kindness and patience. A positive attitude can affect more than just your friends and family; your patients will benefit in so many ways as well!
 First a little personal story. Several years ago my daughter was going through a tough time and we worked with a child psychologist. He was a wonderful man who taught my husband and I so much about how to raise a challenging kiddo. The foundation of what we needed to learn was the power of positive. People need nine (or so) positive interactions to override a negative one. Poor kid was definitely at a deficit! So if she did something that needed correcting, we were to give her a chance at a "do over" where sometimes we had to coach her to choose a better action. After she got it right, we lavished praise on our little pumpkin. And would you believe, not only did all that positiveness make a difference for her, it made a difference for her parents too!
First a little personal story. Several years ago my daughter was going through a tough time and we worked with a child psychologist. He was a wonderful man who taught my husband and I so much about how to raise a challenging kiddo. The foundation of what we needed to learn was the power of positive. People need nine (or so) positive interactions to override a negative one. Poor kid was definitely at a deficit! So if she did something that needed correcting, we were to give her a chance at a "do over" where sometimes we had to coach her to choose a better action. After she got it right, we lavished praise on our little pumpkin. And would you believe, not only did all that positiveness make a difference for her, it made a difference for her parents too!
Now back to the clinical. Just about two years ago I had the privilege of teaching with Nari Clemons. We taught PF2B together. Nari said something during one of her lectures that revolutionized my PT practice. She challenged us in lab to find three positive things about our lab partner and share those things before recognizing any deficits. How many times do we get finished with an evaluation and sit down with a patient and list all the things we found that need correction or help, perhaps drawing on our Netter images to fully illustrate the parts of their body that are broken or need fixing.
So I changed things up a bit and started remarking about the positive things I found on exam. "Wow, your hips are really strong and stable." "You've got a really coordinated breathing pattern, that is going to work in your favor." "You're pelvic muscles are really strong." and then later drawing on those positives outline how we could use the patient's strengths to help them overcome their challenges. "Because you have a great breathing strategy we are going to use that to help your whole nervous system to relax which with help your pelvic floor relax," for example.
The results were shocking. Person after person told me how much it meant to them to leave feeling positive and hopeful. One delightful woman who I saw for a diastasis had amazing leg muscles and I told her so. When she returned she said, "I've felt so self conscious about my flabby belly, but this week all I could think about were my strong leg muscles. Thanks for telling me that."
We do know is that our attitudes and beliefs as providers influence not only our clinical management but patient outcomes as well. Darlow et. al. performed a comprehensive literature review looking at how attitudes and beliefs among health care providers affected outcomes in patients with low back pain and discovered, "There is strong evidence that health care provider beliefs about back pain are associated with the beliefs of their patients."
Why not use that truth to our advantage and be positive? Would love to hear about your experiences!
Join Jennafer at one of her upcoming courses, Pelvic Floor Level 2B - Trenton, NJ - February 24-26, 2017, Pelvic Floor Series Capstone - Arlington, VA - May 5-7, 2017, Pelvic Floor Series Capstone - Columbus, OH - August 18-20, 2017, and Pelvic Floor Series Capstone - Tampa, FL - December 2-4, 2016.
With menopause and the hormonal shifts that take place, some women suffer more than others with symptoms such as hot flashes. If you have ever been near someone during a hot flash, you know that this curious condition is more than feeling a little hot under the collar. During a hot flash, women will suddenly disrobe, wake from a deep sleep covered in sweat (so much so that they have to change the sheets!), or otherwise appear distressed and oftentimes suffer interference in whatever activity in which they were engaging. As we reported in an earlier post, women on average may have hot flashes for 5 years after the date of her last period. Some women (up to 1/3 in the referenced study) will report hot flashes for 10 or more years after menopause.
 Hot flashes and night sweats also significantly disrupt sleep, according to research by Baker and colleagues. Menopausal women with insomnia may also have higher levels of psychologic, somatic, vasomotor symptoms, and score lower on the Beck Depression Inventory, and sleep efficiency and duration scores. Poor sleep can be associated with morbidity such as hypertension, stroke, diabetes and depression, so interrupted sleep is more than an inconvenience, but potentially a serious health issue.
Hot flashes and night sweats also significantly disrupt sleep, according to research by Baker and colleagues. Menopausal women with insomnia may also have higher levels of psychologic, somatic, vasomotor symptoms, and score lower on the Beck Depression Inventory, and sleep efficiency and duration scores. Poor sleep can be associated with morbidity such as hypertension, stroke, diabetes and depression, so interrupted sleep is more than an inconvenience, but potentially a serious health issue.
A more recent study linked anxiety as a potential risk factor for menopausal hot flashes. In 233 women who are premenopausal at baseline and who were followed for at least a year after their final menstrual cycle, anxiety symptoms, hormone levels, hot flashes and other psychosocial variables were assessed. During the 14 year follow-up 72% of the women reported having moderate to severe hot flashes, and the researchers correlated somatic anxiety as a potential predictive association with anxiety. Somatic anxiety refers to the physical symptoms of anxiety, such as stomach ache, increased heart rate, sweating, muscle aches.
In order to help a woman support her wellness during menopausal transitions, being able to address somatic anxiety and conditions like hot flashes is imperative. Teaching skills such as breathing, relaxation training, meditation, or mindfulness may positively impact the anxiety, and therefore have the potential to reduce hot flashes and other adverse symptoms. Herman & Wallace's Menopause Rehabilitation and Symptom Management course is an excellent opportunity to learn some of these valuable skills.
Baker, F. C., Willoughby, A. R., Sassoon, S. A., Colrain, I. M., & de Zambotti, M. (2015). Insomnia in women approaching menopause: beyond perception. Psychoneuroendocrinology, 60, 96-104.
Freeman, E. W., & Sammel, M. D. (2016). Anxiety as a risk factor for menopausal hot flashes: evidence from the Penn Ovarian Aging cohort. Menopause, 23(9), 942-949.
Freeman, E. W., Sammel, M. D., & Sanders, R. J. (2014). Risk of long term hot flashes after natural menopause: Evidence from the Penn Ovarian Aging Cohort. Menopause (New York, NY), 21(9), 924.