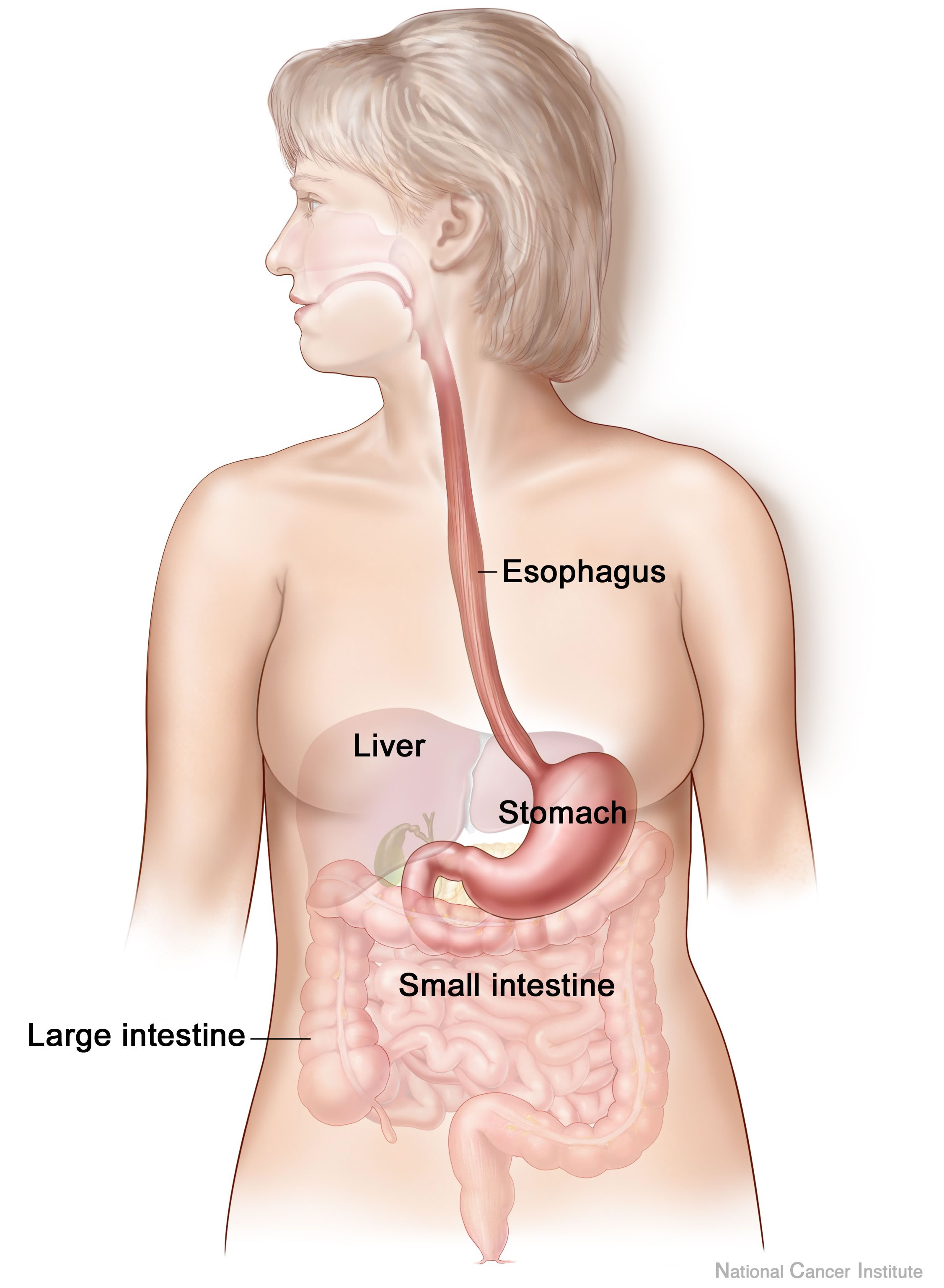
Anxiety and depression are frequently encountered co-morbidities in the clients we serve in pelvic rehabilitation. This observation several years ago in clinical practice is one of many that prompted me down the path of exploring the connection between the gut, the brain, and overall health. In answering the question about these connections, I discovered many nutritionally related truths that are being rapidly elucidated in the literature.
A recent study by Sandhu, et.al. (2017) examines the role of the gut microbiota on the health of the brain and it’s influence on anxiety and depression. The title of the study, “Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry” gives us pause to consider the impact of our diets on this axis and in turn, on the health of our nervous system. The authors state:
It is diet composition and nutritional status that has been repeatedly been shown to be one of the most critical modifiable factors regulating the gut microbiota at different time points across the lifespan and under various health conditions.
With diet and nutritional status being the most critical modifiable factors in the health of this system, it becomes our responsibility to seek to understand this system and its influencing factors. We need to learn how to nourish the microbiota-gut-brain axis.
While anxiety and depression are common co-morbidities we encounter, we also commonly detect imbalance between the sympathetic and parasympathetic nervous system in our patients leading to, for example, pelvic floor muscle tension. In light of this study we must first and foremost ask: what is the microbiota? How can it influence our nervous system? How does this correlate to anxiety and depression? The answers to these questions provide clinical insight with far-reaching impact. We also consider: which circumstances disrupt the health of this system and which improve it? Finally, could understanding of this axis, among other nutritional correlates, provide a novel approach to bowel dysfunction, bladder dysfunction, chronic pelvic pain?
Be a part of the paradigm shift to integrative understanding as we explore these and many other burning questions. Please join us for insightful discussion in White Plains, NY March 31-April 1, 2017 for our next offering of Nutrition Perspectives for the Pelvic Rehab Therapist.
Sandhu, K. V., Sherwin, E., Schellekens, H., Stanton, C., Dinan, T. G., & Cryan, J. F. (2017). Feeding the microbiota-gut-brain axis: diet, microbiome, and neuropsychiatry. Transl Res, 179, 223-244. doi:10.1016/j.trsl.2016.10.002
In the comedy, Kindergarten Cop, Detective John Kimble may only have had a headache, not a tumor, but sometimes our patients do have a tumor. One of my patients was actually just diagnosed with a brain tumor after responding poorly to a cortisone injection for her neck pain. Tumors in other areas of the body, even in the pelvis, can be the source of symptoms that may seem like a nerve entrapment. This is a serious consideration to be given when diagnosing pudendal neuralgia.
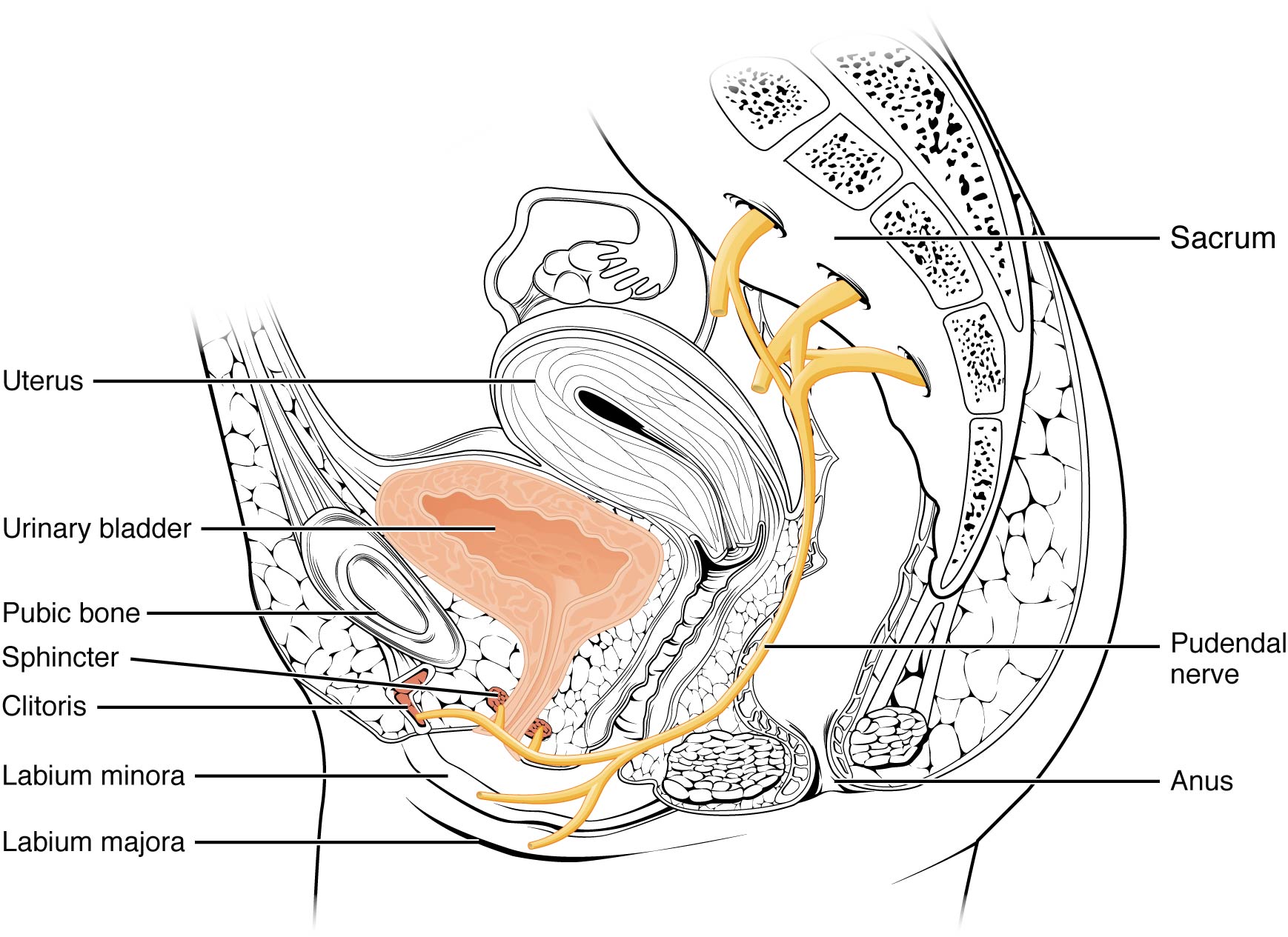 In 2008, Labat et al. published the “Diagnostic Criteria for Pudendal Neuralgia by Pudendal Nerve Entrapment” in Neurourology and Urodynamics . A group in Nantes, France, established criteria in 2006, since the diagnosis is primarily clinical in nature. The results of this paper concluded the five essential diagnostic criteria (Nantes criteria) are as follows:
In 2008, Labat et al. published the “Diagnostic Criteria for Pudendal Neuralgia by Pudendal Nerve Entrapment” in Neurourology and Urodynamics . A group in Nantes, France, established criteria in 2006, since the diagnosis is primarily clinical in nature. The results of this paper concluded the five essential diagnostic criteria (Nantes criteria) are as follows:
- Pain located in the anatomical region of the pudendal nerve.
- Pain worsened with sitting.
- Pain does NOT awaken the patient at night.
- Negative sensory loss upon clinical exam.
- Pain is relieved with an anesthetic pudendal nerve block.
A recent study by Waxweiler, Dobos, Thill, & Bruyninx explored the Nantes criteria as related to choosing surgical candidates for pudendal neuralgia from nerve entrapment. They looked at how a patient’s response to the anesthetic block corresponded to appropriate selection of patients for a successful surgical outcome. Six of 34 patients in the study had a negative anesthetic pudendal nerve block, and 100% of those patients had no symptom relief after surgery. In contrast, 64% of the patients who met all five of the Nantes criteria responded positively to surgery. The authors concluded confirmation of the 5th criteria as essential for predicting success of surgery for pudendal neuralgia by pudendal nerve entrapment.
In Pain Physician in 2016, Ploteau et al. present two case studies where consideration of the Nantes criteria helped diagnose rare tumors in patients who demonstrated red flags during examination. Warning signs such as nocturnal awakening, point-specific pain, pain of a neuropathic nature, and neurological deficits cannot be overlooked when a patient presents with pudendal neuralgia. In the case studies presented, the 31 year old woman did not have pain exacerbated with sitting and woke at night with pain, and the 62 year old woman was awakened at night with pain. Each patient had magnetic resonance imaging performed, and rare diagnoses of endometrial stromal sarcoma and adenoid cystic carcinoma were made, respectively. The tumors arose in the ischiorectal fossa and compressed the pudendal nerve, presenting as pudendal neuralgia in atypical forms requiring careful clinical examination and referral for MRI for accurate diagnosis.
Although a tumor rarely exists, it is our duty to recognize signs and symptoms that do not follow established criteria. Paying attention to what your patients say just may be lifesaving. Proper diagnosis of pudendal neuralgia is essential and sometimes falls in our hands.
Labat, JJ., Riant, T., Robert, R., Amarenco, G., Lefaucheur, JP., Rigaud, J. (2008). Diagnostic criteria for pudendal neuralgia by pudendal nerve entrapment (Nantes criteria). Neurourology and Urodynamics. 27(4):306-10. doi: 10.1002/nau.20505.
Waxweiler, C., Dobos, S., Thill, V., Bruyninx, L. (2016). Selection criteria for surgical treatment of pudendal neuralgia. Neurourology and Urodynamics. doi:10.1002/nau.22988.
Ploteau, S., Cardaillac, C., Perrouin-Verbe, M. , Riant, T., & Labat, J. (2016). Pudendal Neuralgia Due to Pudendal Nerve Entrapment: Warning Signs Observed in Two Cases and Review of the Literature. Pain Physician. 19:E449-E454.
What's the evidence, and what's the answer?
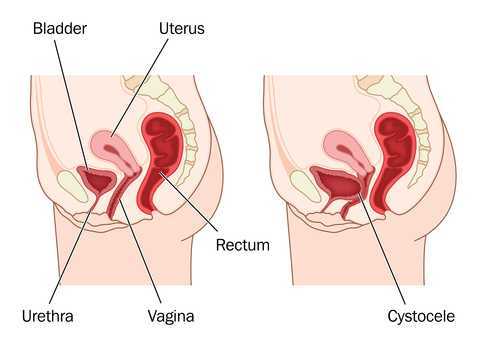
In getting ready to teach my Menopause course in Minneapolis next month, I always like to do a review of the evidence, to see what’s new, or what’s changed. What has changed over the past few years – more and more evidence to support the role of skilled rehab providers, using evidence based assessment techniques to gauge the grade of pelvic organ prolapse and assess the risk of levator avulsion. What hasn’t changed enough – the level of awareness of the benefits of pelvic rehab in managing, or in some cases even reversing, the effects and symptoms of prolapse.
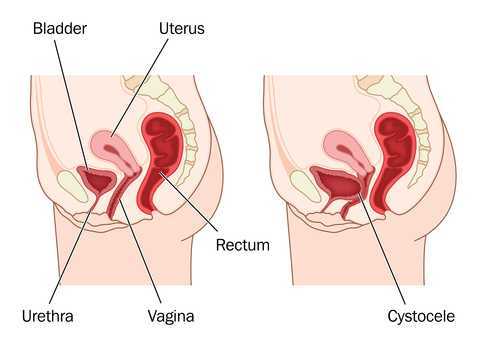 Dr Peter Dietz, from the University of Sydney, writes ‘…although clinical anecdote suggests some physiotherapists recognize other characteristics suggesting muscle dysfunction (e.g. holes, gaps, ridges, scarring) or pelvic floor dysfunction (e.g. width between medial edges of pelvic floor muscle) with palpation it is difficult to find any literature describing the techniques needed to do this or their accuracy or repeatability. Mantle (in 2004) noted that with training and experience a physiotherapist might be able to discern muscle integrity, scarring, and the width between the medial borders of the pelvic floor muscles, with palpation. It is not clear to what extent physiotherapists are able to do this reliably or how such characteristics are to be recorded.’
Dr Peter Dietz, from the University of Sydney, writes ‘…although clinical anecdote suggests some physiotherapists recognize other characteristics suggesting muscle dysfunction (e.g. holes, gaps, ridges, scarring) or pelvic floor dysfunction (e.g. width between medial edges of pelvic floor muscle) with palpation it is difficult to find any literature describing the techniques needed to do this or their accuracy or repeatability. Mantle (in 2004) noted that with training and experience a physiotherapist might be able to discern muscle integrity, scarring, and the width between the medial borders of the pelvic floor muscles, with palpation. It is not clear to what extent physiotherapists are able to do this reliably or how such characteristics are to be recorded.’
Dr Dietz describes a palpation technique to assess the integrity of the pubovisceral muscle insertion, by checking the gap between the urethra centrally and the pubovisceral muscle laterally. On levator contraction this gap should be little wider than your index finger, otherwise an avulsion injury is very likely.
There is another aspect of levator assessment that can yield important information on clinical examination. The size of the levator hiatus can be estimated by determining the sum of the genital hiatus (gh) and perineal body (pb) in the context of the ICS POP-Q examination. Gh + pb, ie., the distance between the external urethral meatus and the centre of the anus, when measured on maximal Valsalva with a simple ruler, is highly predictive of symptoms and signs of prolapse, and it is very strongly correlated with hiatal area on Valsalva (Khunda et al., 2011).
Using this research, in the lab sessions of the Menopause course, we will review these palpation and measurement skills to give therapists the skills they need to confidently assess risk of levator avulsion and its impact on pelvic organ prolapse, and to use this information to devise a functionally appropriate rehab program.
Come and join the conversation in my course, Menopause Rehabilitation and Symptom Management!
Khunda A1, Shek KL, Dietz HP., Am J Obstet Gynecol. 2012 Mar;206(3):246.e1-4. doi: 10.1016/j.ajog.2011.10.876. Epub 2011 Nov 7. Can ballooning of the levator hiatus be determined clinically?
How often have you heard that bedwetting was behavioral or caused by deep sleep and your child would outgrow it? 15% of children per year will “outgrow” bedwetting. What if your child is in the percentile at the end of that range?
Facts:

- Bedwetting affects 15% of girls and 22% of boys
- 5 - 7 Million US children
- Boys are 50% more likely than girls to wet the bed
- 10% of 6 year olds continue to wet
- Spontaneous cure rate 15% per year thereafter
- 1-3% of 18 year olds still wet their beds
- Less than 50% of all bedwetting children have bedwetting alone, without also experiencing daytime urinary leakage or constipation
- Bedwetting is genetic – if one parent was a bed wetter the child has a 40% chance of wetting the bed and if both parents were bedwetters the percentile goes up to 77%
Myths:
- Your child is lazy
- Your child is doing this to get attention
- Your child is just a deep sleeper
- You must wait to grow out of it
Research from the International Children’s Continence Society (ICCS) is a great resource for exploring the research on this topic and other pediatric voiding issues. www.i-c-c-s.org
What causes Bedwetting?
There are many philosophies discussed in the research. Here are some listed below:
- Hormone deficiency- our bladders empty about every 2-3 hours during the day however at night we can hold over 8 hours! This happens because our bodies produce an antidiuretic hormone when we sleep to slow kidney function and produce less urine to empty into the bladder. If this hormone is not being produced, the kidneys produce as much urine at night as they do during the day. In this case, it's good that the bladder empties out in our sleep, otherwise our bladders would be dangerously large and possibly reflux urine backward into the kidneys. Clearly not behavioral!!
- Dr. Steven Hodges has researched and written extensively on the topic of constipation causing pressure from the rectum against the bladder making it irritable during sleep. His research has supported the fact that once the bowel is cleaned out daily the bedwetting episodes diminish. See It’s No Accident by Dr. Hodges or visit https://www.bedwettingandaccidents.com for more information on this topic. Again, a physiological cause of bedwetting versus behavioral.
- Sleep Disturbance and Nasal Airway Obstruction. Dr. Neveus and colleagues reported that 43.5% of children with snoring or obstructive sleep apnea became dry after adenotonsillectomy. Dr. Kovacevic also found increases in antidiuretic hormone seen in responders post-operatively.
Take Home Message
- Active treatment for bedwetting should begin at age 6
- The impact of bedwetting is mainly psychological and may be severe
- Children with bedwetting have abnormal psychological test scores, however once the bedwetting is resolved the test scores return to normal
- “Treatment is not only justified but mandatory”
-ICCS Standardization document 2010
There is help!
At Physical Therapy Specialists we specialize in bedwetting, urinary leakage, constipation and other voiding issues in children. Let us eliminate the need for your family to suffer through this very treatable condition!
Al- Zaben FN, Sehlo MG. Punishement for bedwetting is associated with child depression and reduced quality of life. Child Abuse Negl. 2014
Hodges SJ, Colaco M. Daily enema regimen is superior to traditional therapies for nonneurogenic pediatric overactive bladder. Global Pediatric Health, 2016, 3: 1–4
Austin, P., Bauer, S.B., Bower, W., et al. The standardization of terminology of lower urinary tract function in children and adolescence: update report from the standardization committee of the international children’s continence society. J Urol (2014) 191.
Treatment response of an outpatient training for children with enuresis in a tertiary health care setting. J Pediatr Urol. 2012.
Hodges SJ,Anthony EY::aunrecognizedof. Urology.2012 Feb;79(2):421-4. doi: 10.1016/j.urology.2011.10.015. Epub 2011 Dec 14.
Kovacevic L, Wolfe-Christensen C, Lu H, Toton M, Mirkovic J, Thottam PJ, Abdulhamid I, Madgy D, Lakshmanan Y. Why does adenotonsillectomy not correct enuresis in all children with sleep disordered breathing? J Urol. 2014 May;191(5 Suppl):1592-6.
Nevéus T, Leissner L, Rudblad S, Bazargani F. Acta Paediatr. 2014 Jul 15. doi: 10.1111/apa.12749. [Epub ahead of print]Orthodontic widening of the palate may provide a cure for selected children with therapy-resistant enuresis.
Hodges, Steve J. It’s No Accident-Breakthrough solutions for your child’s wetting, constipation, UTI’s and other potty problems. © 2012. Lyons Press, Guilford, Connecticut.
My manual therapist husband once wrote a paper on the visceral referral pattern of the liver. Although he knows I injured my right shoulder shoveling snow a few years ago, whenever I have an exacerbation of shoulder pain, he likes to joke it is from my liver. (I would laugh if I had not acquired an affinity for red wine since having kids!) Sometimes pain in remote areas of our body really can be related to an organ in distress or simply “stuck” because of fascial restrictions around it. The kidneys in particular can refer pain into the low back and hips, and the bladder and ureters can provoke saddle area pain.

Tozzi, Bongiorno, and Vitturini (2012) looked into the kidney mobility of patients with low back pain. They used real-time Ultrasound to assess renal mobility before and after osteopathic fascial manipulation (OFM) via the Still Technique and Fascial Unwinding. The experimental group receiving OFM consisted of 109 people, and the control group receiving a sham treatment had 31 people, all with non-specific low back pain. For comparison, 101 subjects without back pain were also assessed with the ultrasound to determine a mean Kidney Mobility Score (KMS). The landmarks for measuring the renal mobility were the superior renal pole of the right kidney and the pillar of the right diaphragm, and they subtracted the distance at maximal inspiration (RdI) from that of maximal expiration (RdE). A significant difference was found in the KMS scores of asymptomatic versus symptomatic subjects with low back pain. Pre and post-RD values of the experimental group were significantly different from the control group. The short-form McGill Pain Questionnaire also demonstrated significant differences in the experimental versus control groups. The results of the study revealed a correlation between decreased renal mobility and non-specific low back pain and showed an improvement in renal mobility and low back pain after an osteopathic manipulation.
In 2016, Navot and Kalichman presented a case study of a 32 year old professional male cyclist with right hip and groin pain after an accident that caused a severe hip contusion and tearing of the tensor fascia latae and the gluteus medius muscles. A few rounds of physical therapy gave him partial relief of his pain in sitting and with cycling, and his hip range of motion only improved slightly. Despite no complaints of pelvic floor dysfunction, he was evaluated for involvement of the pelvic floor musculature and fascia. Pelvic Floor Fascial Mobilization was performed for 2 sessions, and the cyclist’s symptoms resolved completely. This case implied the efficacy of manual fascial release of the pelvic floor to reduce hip and groin pain.
When something seemingly orthopedic in nature does not respond with full resolution of symptoms from traditional physical therapy, the source of the pain may be deeper. Often times, we just need to ask the right questions to uncork the mystery of why a pain is lingering. No matter how skilled we are with our techniques, if we are not reaching the area in need, we are wasting our effort and our patients’ time and money. “Mobilization of Visceral Fascia: The Urinary System” is a course that provides a practitioner with the extra insight and tools to address potential sources of unresolved symptoms of low back, hip, and groin pain.
Tozzi, P., Bongiorno, D., and Vitturini, C. (2012) Low back pain and kidney mobility: local osteopathic fascial manipulation decreases pain perception and improves renal mobility. Journal of Bodywork and Movement Therapies. 16(3):381-91. doi: 10.1016/j.jbmt.2012.02.001
Navot, S and Kalichman, L. (2016). Hip and groin pain in a cyclist resolved after performing a pelvic floor fascial mobilization. Journal of Bodywork and Movement Therapies. 20(3):604-9. doi:10.1016/j.jbmt.2016.04.005
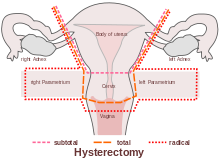
A recent systematic review by Bernard et al (2016) looked at the effects of radiation therapy on the structure and function of the pelvic floor muscles of patients with cancer in the pelvic area. Although surgery and chemotherapy are often used treatment approaches in the management of pelvic cancers, this paper specifically focused on radiation therapy: ‘… is often recommended in the treatment of pelvic cancers. Following radiation therapy, a high prevalence of pelvic floor dysfunctions (urinary incontinence, dyspareunia, and fecal incontinence) is reported. However, changes in pelvic floor muscles after radiation therapy remain unclear. The purpose of this review was to systematically document the effects of radiation therapy on the pelvic floor muscle structure and function in patients with cancer in the pelvic area.’
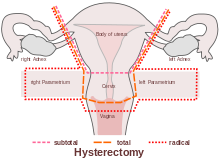 The paper concluded that ‘…There is some evidence that radiation therapy has detrimental impacts on both pelvic floor muscles' structure and function’ and that ‘A better understanding of muscle damage and dysfunction following radiation therapy treatment will improve pelvic floor rehabilitation and, potentially, prevention of its detrimental impacts.’
The paper concluded that ‘…There is some evidence that radiation therapy has detrimental impacts on both pelvic floor muscles' structure and function’ and that ‘A better understanding of muscle damage and dysfunction following radiation therapy treatment will improve pelvic floor rehabilitation and, potentially, prevention of its detrimental impacts.’
Pelvic floor therapists already working in the field of gynecologic oncology will be all too aware of the impacts clinically and functionally on pelvic cancer survivors’ quality of life. We are in a privileged position to provide an evidence based and solution focused approach to the pelvic health issues that are so often under-recognized, and frankly under-addressed for women undergoing treatment for pelvic cancers.
Whether it is advice on managing anal fissures (skin protection, down-training overactive pelvic floor muscles, achieving good stool consistency, teaching defecatory techniques) or dealing with dyspareunia (dilator or vibrator selection, choosing and using an appropriate lubricant, dealing with the ergonomic or orthopedic challenges that can be a barrier to returning to sexual function and enjoyment), pelvic rehab practitioners are probably the best clinicians for optimizing a return to both pelvic and global health during and after treatment for pelvic cancers.
But one of the biggest barriers we face is lack of awareness – on the part of the patients but also, unfortunately the lack of awareness in the medical and oncology community about the benefits of pelvic rehab. Happily this situation is improving – not only is the evidence base expanding from the researchers, but oncologists are recognizing that pelvic rehab is a key component of regaining quality and not just quantity of life after treatment ends. As Yang reported in his 2012 paper – pelvic floor rehab programs improve pelvic floor function (particularly urinary continence and sexual function) and overall quality of life in gynecologic cancer patients. And perhaps, most heartening of all, was his statement that "Pelvic Floor Rehab Physiotherapy is effective even in gynecologic cancer survivors who need it the most"
You can learn more about pelvic floor muscle rehabilitation for cancer patients by attending "Oncology and the Female Pelvic Floor: Female Reproductive and Gynecologic Cancers" on April 29-30, 2017 in Maywood, IL.
‘Effects of radiation therapy on the structure and function of the pelvic floor muscles of patients with cancer in the pelvic area: a systematic review.’ J Cancer Surviv. 2016 Apr;10(2):351-62. doi: 10.1007/s11764-015-0481-8. Epub 2015 Aug 28. Bernard, S. et al
‘Effect of a pelvic floor muscle training program on gynecologic cancer survivors with pelvic floor dysfunction: a randomized controlled trial.’ Gynecol Oncol. 2012 Jun;125(3):705-11. doi: 10.1016/j.ygyno.2012.03.045. Epub 2012 Apr 1. Yang EJ, et al
When my almost 4 year old still wets his bed in the middle of the night, my first reaction is frustration; but, I learned that gets us nowhere fast, so now I just roll with the punches. Usually the culprit is my stubborn son’s simple refusal to go the bathroom before bed. When enuresis is secondary to neurogenic disorders or anxiety disorders, caregivers need to have even more patience with children.
 Sturm and Cheng (2016) published a review on the management of neurogenic bladder in the pediatric population. Central nervous system (CNS) lesions including cerebral palsy, spinal cord injury, and spinal malformations, as well as pelvic tumors or anorectal malformations, can all affect normal lower urinary tract function. Children with neurogenic bladder often have the condition because of a CNS lesion. This can affect the bladder’s ability to store and empty urine, so early intervention is essential and focuses on maximizing bladder function and avoiding injury to the upper or lower urinary tracts. With older children, the goals are urinary continence and independent bladder management.
Sturm and Cheng (2016) published a review on the management of neurogenic bladder in the pediatric population. Central nervous system (CNS) lesions including cerebral palsy, spinal cord injury, and spinal malformations, as well as pelvic tumors or anorectal malformations, can all affect normal lower urinary tract function. Children with neurogenic bladder often have the condition because of a CNS lesion. This can affect the bladder’s ability to store and empty urine, so early intervention is essential and focuses on maximizing bladder function and avoiding injury to the upper or lower urinary tracts. With older children, the goals are urinary continence and independent bladder management.
Myelomeningocele surgical prenatal closure has had minimal effect on urinary tract function, and parents are encouraged to monitor urological changes because of the child’s risk for neurogenic bladder. Clean intermittent catheterization (CIC) has reduced the morbidity in patients with neurogenic bladder. Determining which children would benefit from initiation of CIC and when medical or surgical interventions should be implemented remains a challenge. Anticholinergics have proven effective on continence and bladder compliance either orally or, more recently, intravesical administration. Surgically, autologous augmentation using the ileum or colon has shown fatal complications like bowel obstruction and bladder rupture, particularly when bladder neck procedures are performed concurrently. Robotic versus open bladder neck reconstruction has been proving more favorable in recent studies. The authors concluded more research is needed for treatment, and the goals are preservation of the upper and lower urinary tracts, optimizing quality of life (Sturm and Cheng 2016).
Considering a different side of nerves, Salehi et al., (2016) studied the relationship between primary nocturnal enuresis and child anxiety disorders. They studied 180 children with primary nocturnal enuresis (referring to children >5 years old having no urine control 6 continuous months) and 180 healthy controls. A statistically significant difference was found between the two groups regarding the frequency of generalized anxiety disorder as well as panic disorder, school phobia, social and separation anxieties, maternal anxiety history, parental history of primary nocturnal enuresis and body mass index. The authors recommended any children with primary nocturnal enuresis should be assessed and treated for generalized anxiety disorder.
The seriousness of enuresis cannot be underestimated. When the cause is neurogenic, pharmacological or surgical intervention may be warranted and lifelong urologic management is needed, especially for a healthy transition into adulthood. As common as nocturnal bed wetting may be in school aged children, they should be monitored for the presence of any anxiety disorders that may be contributing to the disorder. Changing sheets may feel like a burden for parents, but the child with enuresis has a far greater weight to bear.
You can learn all about caring for pediatric patients by attending Pediatric Incontinence and Pelvic Floor Dysfunction with Dawn Sandalcidi, available twice in 2017.
Sturm, R. M., & Cheng, E. Y. (2016). The Management of the Pediatric Neurogenic Bladder. Current Bladder Dysfunction Reports, 11, 225–233. http://doi.org/10.1007/s11884-016-0371-6
Salehi, B., Yousefichaijan, P., Rafeei, M., & Mostajeran, M. (2016). The Relationship Between Child Anxiety Related Disorders and Primary Nocturnal Enuresis. Iranian Journal of Psychiatry and Behavioral Sciences, 10(2), e4462. http://doi.org/10.17795/ijpbs-4462
In this “quick fix” society, few people accept that musculoskeletal pain will require a commitment to following an exercise program for an extended period of time. If a hypomobile joint just needs to get moving and lubricated, one may get relief with a few manual therapy treatments and exercise sessions. However, if a joint is hypermobile (unstable) or degenerative and provokes a high level of pain, the rehab requires more time. The sacroiliac (SI) joint is one of those areas often requiring patients to work harder for the resolution of pain and dysfunction, but many seek surgical intervention instead.
 Polly et al. (2016) performed a randomized controlled trial of minimally invasive sacroiliac joint fusion (SIJF) with placement of a system of triangular titanium implants using a lateral transiliac approach versus non-surgical management (NSM) for SI dysfunction. Of the 148 subjects, 102 underwent SIJF and 46 had NSM. The NSM group received medication, physical therapy per American Physical Therapy Association guidelines, steroid injections and radiofrequency ablation of sacral nerve root lateral branches. The surgical group showed superior outcomes at a 2 year follow up, as clinical improvement per VAS pain score was 83.1% and ODI was 68.2%. The NSM group showed <10% improvement.
Polly et al. (2016) performed a randomized controlled trial of minimally invasive sacroiliac joint fusion (SIJF) with placement of a system of triangular titanium implants using a lateral transiliac approach versus non-surgical management (NSM) for SI dysfunction. Of the 148 subjects, 102 underwent SIJF and 46 had NSM. The NSM group received medication, physical therapy per American Physical Therapy Association guidelines, steroid injections and radiofrequency ablation of sacral nerve root lateral branches. The surgical group showed superior outcomes at a 2 year follow up, as clinical improvement per VAS pain score was 83.1% and ODI was 68.2%. The NSM group showed <10% improvement.
Sachs et al. (2016) studied outcomes of patients ≥3 years after SIJF for chronic (>5 years) SIJ dysfunction secondary to degenerative sacroiliitis or SIJ disruption. One hundred and seven patients participated in the study, and minimally invasive transiliac SIJF was definitively correlated with decreased pain, low disability scores, and improvements in activities of daily living performance. Sadly, these authors stated, “there is no high-quality evidence that physical therapy is effective in chronic SIJ pain.”
Even radiofrequency neurotomy or neural ablation revealed positive results for patients according to Reddy et al. (2016). The authors explored 14 patients’ responses 1 year after Simplicity radiofrequency (RF) of the lateral branches of S1-S3 in a retrospective review. Improvements in global health per SF12 as well as pain reduction were statistically significant.
Jonely et al. (2015) presented a case study of a woman with a 14-year history of SIJ pain whose symptoms persisted after 2 months of physical therapy. A multi-modal approach was then pursued with success, even at the 1 year follow up. The patient received 4 prolotherapy injections, SIJ manipulation into nutation, a pelvic girdle belt, and specific stabilization exercises. Over a 12-month period, the patient had 20 physical therapy sessions. Her Oswestry Disability score improved from 34% to 14% at 6 months and was 0% at 1 year. Numeric pain scale rating improved to 4/10 at 6 months and 0/10 at 1 year. The authors concluded a multimodal approach can be successful to manage SIJ dysfunction.
Clearly, if quality of life is so poor a person cannot function because of SIJ pain and therapy has failed, surgery may be the only choice. I exhaust all conservative measures before I cry “uncle” for a surgical fix. Despite a paucity of literature on manual therapy and sacroiliac treatment, I know there are clinicians successfully treating patients with SI dysfunction. Taking the Sacroiliac Joint Evaluation and Treatment can broaden your scope of understanding the SI joint and how to provide the most effective treatment, possibly preventing more invasive techniques for patients.
Polly, D. W., Swofford, J., Whang, P. G., Frank, C. J., Glaser, J. A., Limoni, R. P., … and the INSITE Study Group. (2016). Two-Year Outcomes from a Randomized Controlled Trial of Minimally Invasive Sacroiliac Joint Fusion vs. Non-Surgical Management for Sacroiliac Joint Dysfunction. International Journal of Spine Surgery, 10, 28. http://doi.org/10.14444/3028
Sachs, D., Kovalsky, D., Redmond, A., Limoni, R., Meyer, S. C., Harvey, C., & Kondrashov, D. (2016). Durable intermediate-to long-term outcomes after minimally invasive transiliac sacroiliac joint fusion using triangular titanium implants. Medical Devices (Auckland, N.Z.), 9, 213–222. http://doi.org/10.2147/MDER.S109276
Anjana Reddy, V. S., Sharma, C., Chang, K.-Y., & Mehta, V. (2016). “Simplicity” radiofrequency neurotomy of sacroiliac joint: a real life 1-year follow-up UK data. British Journal of Pain, 10(2), 90–99. http://doi.org/10.1177/2049463715627287
Jonely, H., Brismée, J.-M., Desai, M. J., & Reoli, R. (2015). Chronic sacroiliac joint and pelvic girdle dysfunction in a 35-year-old nulliparous woman successfully managed with multimodal and multidisciplinary approach. The Journal of Manual & Manipulative Therapy, 23(1), 20–26. http://doi.org/10.1179/2042618614Y.0000000086
After greeting a patient referred for temporomandibular joint dysfunction, the conversation began with an outpouring of emotion over a failed bladder sling surgery that left the woman with significant chronic pain, causing her to clench her jaw all the time. No matter what I was to find objectively with the examination, there was no doubt the treatment had to extend beyond joint mobilization, soft tissue work, and exercise. This woman clearly saw her cup as half empty, so filling her mind with a new approach to thinking about and dealing with her pain was essential for relieving her secondary jaw pain.
 Su et al. published a study called, “Pain Perception Can Be Modulated by Mindfulness Training: A Resting-State fMRI Study” (2016). The pain-afflicted group had 18 participants while the control group had 16. Brain behavior response of all subjects was measured per resting-state functional magnetic resonance imaging and 3 forms (Dallas Pain Questionnaire, Short Form McGill Pain Questionnaire-SFMPQ, and Kentucky Inventory of Mindfulness) before and after 6 weeks of mindfulness-based stress reduction treatment. Training consisted of mindfulness meditations such as a body scan, hatha yoga, walking and sitting meditation, and instruction on how to use the methods for pain management. After six 2.5-hour sessions/week and one 8-hour non-verbal session in the 4th week, the fMRI showed an increased connection from the anterior insular cortex (AIC) to the dorsal anterior midcingulate cortex (daMCC), and the SFMPQ scores were significantly improved in the pain-afflicted group. The authors suggested mindfulness training can change the brain connectivity responsible for our perception of pain.
Su et al. published a study called, “Pain Perception Can Be Modulated by Mindfulness Training: A Resting-State fMRI Study” (2016). The pain-afflicted group had 18 participants while the control group had 16. Brain behavior response of all subjects was measured per resting-state functional magnetic resonance imaging and 3 forms (Dallas Pain Questionnaire, Short Form McGill Pain Questionnaire-SFMPQ, and Kentucky Inventory of Mindfulness) before and after 6 weeks of mindfulness-based stress reduction treatment. Training consisted of mindfulness meditations such as a body scan, hatha yoga, walking and sitting meditation, and instruction on how to use the methods for pain management. After six 2.5-hour sessions/week and one 8-hour non-verbal session in the 4th week, the fMRI showed an increased connection from the anterior insular cortex (AIC) to the dorsal anterior midcingulate cortex (daMCC), and the SFMPQ scores were significantly improved in the pain-afflicted group. The authors suggested mindfulness training can change the brain connectivity responsible for our perception of pain.
Chadi et al.2016 performed a pilot study of female adolescents with chronic pain regarding the efficacy of mindfulness-based treatment. The experimental group (n=10) and the wait-list control group (n=9) consisted of girls between the ages of 13 and 18. For 8 weeks they met for a 90 minute session led by a psychiatry resident. Some of the mindfulness practices in this study included body scan, sitting and walking meditations, love and kindness meditations, mindful eating, compassion and deep listening, and breathing exercises. The wait-list control group also completed the 8-week program. Although all participants reported a positive change in the way they coped with pain, no statistically significant changes in quality of life, depression, anxiety, pain perception, and psychological distress were found. Significant salivary cortisol level improvements were observed (p<0.001) post mindful-based treatment session, indicating feasibility in pursuing further research with a larger randomized controlled trial.
Panahi and Faramarzi2016 studied mindfulness therapy effects on anxiety and depression for premenstrual syndrome (PMS). Sixty students (30 experimental, 30 control with no treatment) with mild to moderate PMS with depression underwent 8 weekly 120 minute sessions of mindfulness-based cognitive therapy (MBCT). Mean score improvements in depression, anxiety, and PMS were statistically significant from pre to post treatment for the subjects receiving MBCT. The authors stated MBCT psychotherapy could be considered beneficial for depression in mild to moderate PMS.
If jaw-clenching chronic pain owns a patient, he or she could benefit from managing the relationship through mindfulness. Our perception of pain is at the core of “whole body” treatment. The Mindfulness Based Pain Treatment course could help fill your patients’ as well as your own cup with healing.
If you're interested in learning more about mindfulness-based treatment techniques, Herman & Wallace offers three courses which you should consider. Mindfulness-Based Pain Treatment focuses on patient treatment, and the Mindfulness for Rehabilitation Professionals.
Su, I.-W., Wu, F.-W., Liang, K.-C., Cheng, K.-Y., Hsieh, S.-T., Sun, W.-Z., & Chou, T.-L. (2016). Pain Perception Can Be Modulated by Mindfulness Training: A Resting-State fMRI Study. Frontiers in Human Neuroscience, 10, 570. http://doi.org/10.3389/fnhum.2016.00570
Chadi, N., McMahon, A., Vadnais, M., Malboeuf-Hurtubise, C., Djemli, A., Dobkin, P. L., … Haley, N. (2016). Mindfulness-based Intervention for Female Adolescents with Chronic Pain: A Pilot Randomized Trial. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 25(3), 159–168.
Panahi, F., & Faramarzi, M. (2016). The Effects of Mindfulness-Based Cognitive Therapy on Depression and Anxiety in Women with Premenstrual Syndrome. Depression Research and Treatment, 2016, 9816481. http://doi.org/10.1155/2016/9816481
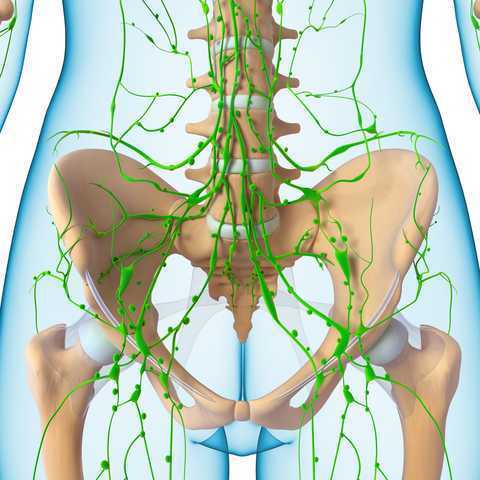
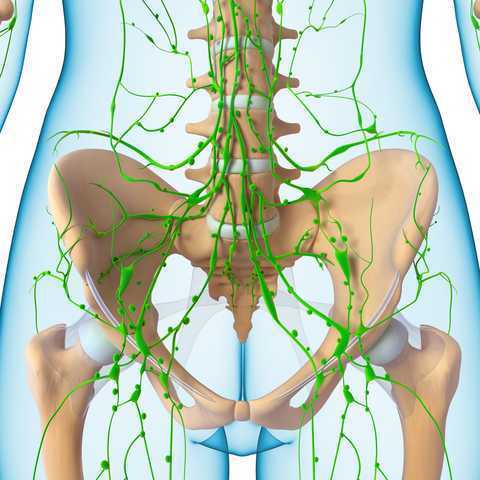 In 1998, faculty member Debora Chassé was asked to evaluate a patient with bilateral lower extremity lymphedema following repeated surgeries for cervical cancer. Her formal education did not cover this in school, so Dr. Chassé began to study peer-review research and consult with other clinicians about the diagnosis. Her journey down the rabbit hole began.
In 1998, faculty member Debora Chassé was asked to evaluate a patient with bilateral lower extremity lymphedema following repeated surgeries for cervical cancer. Her formal education did not cover this in school, so Dr. Chassé began to study peer-review research and consult with other clinicians about the diagnosis. Her journey down the rabbit hole began.
Dr. Chassé became a certified lymphedema therapist in 2000 and a certified Lymphology Association of North America therapist in 2001. She continued training by moving into osteopathy taking her into the direction of lymphatic vessel manipulation. In 2006 she began taking courses in pelvic pain and obstetrics with a focus on pelvic floor dysfunction. It was at this point that Dr. Chasse realized nobody was applying lymphatic treatment to women’s health and pelvic floor dysfunction. In 2009 she became a Board Certified Women’s Health Clinical Specialist in Physical Therapy and began traveling around the United States offering workshops in the area of lymphatic treatment.
Dr. Chassé’s approach is to incorporate all her varied skills in the clinic to produce the best patient outcomes. Debora explains that she is “…showing the similarities between pelvic pain and the lymphatic system. The treatment principles are the same, when you are treating both lymphedema or pelvic pain, you are working to reduce inflammation, pain and scarring.”
Another advantage of the lymphatic treatment approach is that it is more comfortable for the patient. “Most intravaginal techniques causes increased pain and inflammation. However, using lymphatic drainage intravaginally is well tolerated and decreases the intravaginal pain. The results are phenomenal!”
Dr. Chassé recollects her experience with a 21 year old female who suffered from chronic pelvic pain. By applying intravaginal lymphatic drainage techniques for 5 consecutive days, the patient experience a 4.83 reduction in pelvic girdle circumference and her intravaginal pain went from 8/10 to 2/10. The patient was amazed at how much better she felt. “My pants fit better, my energy level increased 25% and pain decreased more than 50%. I went from having 2-3 bad days per week to having 2-3 bad days per month, even when my work level increased. My feet no longer swell and I haven’t missed any classes since receiving this treatment.
In her course, “Lymphatics and Pelvic Pain: New Strategies”, Dr. Chassé seeks to train practitioners to utilize lymphatic drainage techniques when treating specifically pelvic pain. Participants will learn lymphatic drainage principles and techniques. They will learn how to clear pathways to transport lymph fluid and internal techniques which will have incredible impacts for patients.