Vaginal wall thinning associated with menopausal changes can cause vaginal burning and pain, limitations in sexual function, and vaginal redness or even changes in discharge. Because these symptoms can mimic many other conditions such as pelvic floor muscle dysfunction or an infection, it is necessary for the pelvic rehabilitation therapist to be alert to identifying vaginal atrophy as an issue to rule out so that patients can access appropriate medical care when needed.
 Atrophic vaginitis (AV) is a condition of the vaginal walls associated with tissue thinning, discomfort, and inflammation. The tissue changes often extend into the vulvar area as well. Atrophic vaginitis may also be called vaginal atrophy, vulvovaginal atrophy, urogenital atrophy, or genitourinary syndrome of menopause. Although we tend to associate menopause with women who are in their 40’s or 50’s, any woman who has stopped having her menstrual cycles or who has had a significant reduction in her cycles may be at risk for vaginal atrophy. Any woman who has had a hysterectomy may also be at risk of this thinning of the vaginal walls. Common symptoms of vaginal wall thinning include vaginal dryness, tissue irritation, redness, itching, and a “burning” pain. Interruption in sleep, limitations in activities of daily living, and changes in mood and temperament have also been reported.
Atrophic vaginitis (AV) is a condition of the vaginal walls associated with tissue thinning, discomfort, and inflammation. The tissue changes often extend into the vulvar area as well. Atrophic vaginitis may also be called vaginal atrophy, vulvovaginal atrophy, urogenital atrophy, or genitourinary syndrome of menopause. Although we tend to associate menopause with women who are in their 40’s or 50’s, any woman who has stopped having her menstrual cycles or who has had a significant reduction in her cycles may be at risk for vaginal atrophy. Any woman who has had a hysterectomy may also be at risk of this thinning of the vaginal walls. Common symptoms of vaginal wall thinning include vaginal dryness, tissue irritation, redness, itching, and a “burning” pain. Interruption in sleep, limitations in activities of daily living, and changes in mood and temperament have also been reported.
One common pharmacological intervention for vaginal and vulvar atrophy is the topical application of hormone creams such as estrogen. A recent study examined the effects of low dose estrogen therapy on bacteria that populates the vaginal walls.Shen et al., 2016 This bacteria may be causal or correlated to vaginal health, and also appears related to estrogen levels. Sixty women diagnosed with atrophic vaginitis were treated with low dose estrogen therapy and followed for four weeks to assess the vaginal microbiotia via mid-vaginal swabs. Following are highlights from the linked study’s findings,
- Prior to treatment, in symptomatic postmenopausal women the Lactobacilli species were less abundant and made up 11.2% of the community, while in asymptomatic women, the communities were more than 50% lactobacilli
- Gardnerella was more abundant than Lactobacillus in women with atrophic vaginitis
- Overall diversity of bacterial communities between healthy women and those with atrophic vaginitis was not significantly different
- In response to treatment with estrogen, women with AV reported improved symptoms and decreased vaginal pH
- Serum estradiol improved on average from approximately 42 pmol/L to 168 pmol/L by week 2, with little change from week 2 to week 4
- Lactobacillus count was negatively correlated with symptoms (i.e., more Lactobacillis = less symptoms) and Gardnerella and Atopobium counts were positively correlated with symptoms
- There were variations noted in how each woman’s vaginal bacterial communities responded to the estrogen therapy in that some women had a dominance of other bacteria after 4 weeks even though their symptoms decreased
In conclusion, the authors stated that “…a Lactobacillus-dominated vaginal community may be considered as one of the signs of AV treatment success…” along with reduced symptoms and increased serum estradiol levels. Prior studies have recognized barriers to treatment that include lack of patient knowledge of vulvar and vaginal atrophy, failure to discuss associated symptoms with physicians, concerns about safety of treatments or poor symptom relief with prescribed interventions.Kingsburg et al., 2013 This leaves the pelvic rehabilitation provider in a excellent role of educating women in the signs and symptoms of atrophic vaginitis, observing the tissues for changes, and communicating with referring providers and prescribers if a concern is noted. Furthermore, failure to recognize the potential for vaginal atrophy and treating these tissues with manual therapy or exercise may injure or exacerbate the problem.
Interested in learning more? Keep an eye out for a Menopause Rehabilitation and Symptom Management course with Michelle Lyons!
Changes in the Vagina and Vulva. Retrieved June 27, 2016 from http://www.menopause.org/for-women/sexual-health-menopause-online/changes-at-midlife/changes-in-the-vagina-and-vulva
Kingsberg, S. A., Wysocki, S., Magnus, L., & Krychman, M. L. (2013). Vulvar and vaginal atrophy in postmenopausal women: findings from the REVIVE (REal Women's VIews of Treatment Options for Menopausal Vaginal ChangEs) survey. The journal of sexual medicine, 10(7), 1790-1799.
Shen, J., Song, N., Williams, C. J., Brown, C. J., Yan, Z., Xu, C., & Forney, L. J. (2016). Effects of low dose estrogen therapy on the vaginal microbiomes of women with atrophic vaginitis. Scientific reports, 6.
Vaginal Atrophy. Retrieved June 27, 2016 from http://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/home/ovc-20200167
Spending the past 5 years watching a lot of Disney Junior and reading Dr. Seuss, professional journal reading is generally reserved for the sanctuary of the bathroom. When patients ask if I’ve heard of certain new procedures or therapies, I try to sound intelligent and make a mental note to run a PubMed search on the topic when I get home. Making the effort to stay on top of research, however, makes you a more confident and competent clinician for the information-hungry patient and encourages physicians to respect you when it comes to discussing their patients.
A 2016 article in Translational Andrology and Urology, Lin et al., explored rehabilitation of men post radical prostatectomy on a deeper level, trying to prove that brain-derived neurotrophic factor (BDNF) promotes nerve regeneration. In many radical prostatectomies, even when the nerve-sparing approach is used, there is injury to the cavernous nerves, which course along the posterolateral portion of the prostate. Cavernous nerve injury can cause erectile dysfunction in 60.8-93% of males postoperatively. The authors discussed Schwann cells as being vital for maintaining integrity and function of peripheral nerves like the cavernous nerve. They hypothesized that BDNF, a member of the neurotrophin family that supports neuron survival and prevents neuronal death, activates the JAK/STAT (Janus kinase /signal transducer and activator of transcription) pathway in Schwann cells, thus facilitating axonal regeneration via secretion of cytokines (IL-6 and OSM-M). Through scientific experiment on a cellular level (please refer to the article for the specific details), the authors were able to confirm their hypothesis. Schwann cells do, in fact, produce cytokines that contribute to the regeneration of cavernous nerves.
From a different cellular perspective, Haahr et al., (2016) performed an open-label clinical trial involving intracavernous injection of “autologous adipose-derived regenerative cells” (ADRCs) in males experiencing erectile dysfunction (ED) after radical prostatectomy. Current treatments with PDE-5 inhibitors do not give satisfactory results, so the authors performed a human phase 1, single-arm trial to further the research behind the use of adipose-derived stem cells for ED. Some limitations included the study was un-blinded and had no control group. Seventeen males who had ED after radical prostatectomy 5-18 months prior to the study were followed for 6 months post intracavernosal transplantation. The primary outcome was safety/tolerance of stem cell treatment, and the secondary was improvement of ED. The single intracavernosal injection of freshly isolated autologous adipose-derived cells resulted in 8 of 17 men regaining erectile function for intercourse; however, the men who were not continent did not regain erectile function. The end results showed the procedure was safe and well-tolerated. There was a significant improvement in scores for the International Index of Erectile Function-5 (IIEF-5), suggesting this therapy may be a promising one for ED after radical prostatectomy.
In the clinic, we need to treat our patients to the best of our ability. Taking the Post-Prostatectomy Patient Rehabilitation course is vital if even just one patient enters your office seeking treatment. Keeping up on research (even that which seems too full of forgotten science) and learning new manual techniques and exercises can help us rise as clinicians prepared to optimize patients’ function.
Lin, G., Zhang, H., Sun, F., Lu, Z., Reed-Maldonado, A., Lee, Y.-C., … Lue, T. F. (2016). Brain-derived neurotrophic factor promotes nerve regeneration by activating the JAK/STAT pathway in Schwann cells. Translational Andrology and Urology, 5(2), 167–175. http://doi.org/10.21037/tau.2016.02.03
Haahr, M. K., Jensen, C. H., Toyserkani, N. M., Andersen, D. C., Damkier, P., Sørensen, J. A., … Sheikh, S. P. (2016). Safety and Potential Effect of a Single Intracavernous Injection of Autologous Adipose-Derived Regenerative Cells in Patients with Erectile Dysfunction Following Radical Prostatectomy: An Open-Label Phase I Clinical Trial. EBioMedicine, 5, 204–210. http://doi.org/10.1016/j.ebiom.2016.01.024
Yoga offers a compelling mind-body approach to maternal care that is forward thinking and aligns with the World Health Organization and Institute of Medicine’s recommendations for patient-centered care. But let’s take a look at WHY postpartum care MUST change in order to establish need for the entry of yoga into postpartum care.
Maternal Health Track Record
The United States and similarly developed countries have a very poor track record for postpartum care. The record is so poor that the problem in the US has been labeled a “human rights failure.”1
 On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
On its own, the US has the worst track record for not only postpartum care, but for maternal and infant mortality and first-day infant death rate in the developed world (Save the Children 2013). Between 1999-2008, global mortality rates decreased by 34% while the US’s rates doubled for mothers.1
Patient satisfaction also suffers under the current model of care, with many more mothers experiencing postpartum depression, a significant risk factor for both mother and baby during and after pregnancy.
The increase in mortality and poor outcomes can, in part, be attributed not to underuse, but overuse of medical intervention during pregnancy and birth. 2,3,4 Countries that have “access to woman-centered care have fewer deaths and lower health care costs”; and, hospital system reviews in the US show that reducing medical interventions are both reducing cost and improving outcomes.1,4,5
The notorious lack of accountability (reporting system) in maternal health care also plagues the US and suggests that maternal deaths are even higher than currently reported, leading to Coeytaux’s conclusion that the “United States is backsliding.”1
Improving Postpartum Outcomes with Integrated Physical Therapy Care
In After the Baby’s Birth, maternal health advocate Robin Lim writes,
"All too often, the only postpartum care an American woman can count on is one fifteen minute appointment with her doctor, six weeks after she has given birth. This six-week marker ends an arbitrary period within which she is supposed to have worked out most postpartum questions for herself. This neglect of postpartum women is not just poor healthcare, it is abusive, particularly to women suffering from painful physical and/or psychological disorders following childbirth."
Physical therapists can be instrumental change agents in improving current postpartum care, especially through the integration of contemplative sciences like yoga. Yoga can be the cornerstone of holistically-driven, person-centered care, especially in comorbid conditions such as pelvic pain and depression, where pharmacological side effects, stigma, can severely diminish adherence to biomedical interventions.6 Coeytaux, as well as other authors, clearly correlate the reduction of maternal mortality with improved postpartum care. The World Health Organization recommends that postpartum checkups should include screening for:
- Back pain
- Incontinence (stress)
- Hemorrhoids
- Constipation
- Fatigue
- Breast pain
- Perineal pain
- Depression
- Painful or difficult intercourse
- Headaches
- Bowel problems
- Dizziness or fainting
 A physical therapist is a vital team member in not only screening for many of the
A physical therapist is a vital team member in not only screening for many of the
listed problems above, but in managing them. It is important to note that other countries, like France, deliver high quality postpartum rehab care plus in-home visits, all while spending far less than the US on maternal care.
The World Health Organization, however, clarifies the vital importance of postpartum care delivery by making a significant recommendation for a paradigm shift in biomedical care.7
Yoga as a “Best Care Practice” for Postpartum Care
The WHO recommends the use of a biopsychosocial model of care, which yoga is ideally suited to provide via its ancient, multi-faceted person-centered philosophy. Medical Therapeutic Yoga is a unique method of combining evidence-based rehabilitation with yoga to emerge with a new paradigm of practice. MTY:
- Addresses the mother as a person, not as a condition or diagnosis.
- Empowers mothers with self-care strategies for systems-based, not just musculoskeletal or neuromuscular, change.
- Addresses all domains of biopsychosocial impairment.
- Teaches interdisciplinary partnership-based theory, which is integral to creative collaborative discourse and innovation in postpartum care.
- Equips clinicians with business service, website development, practice paradigm, and social media campaign tools to fully develop the new clinical niche of Professional Yoga Therapy practice.
- Promotes patient advocacy, health promotion, and public health education via mainstreaming yoga into rehabilitative and medical services.
- Provides the gender context for prescription that traditional yoga is lacking.
- Evolves yoga for use in prenatal and postpartum care.
Physical therapy screening and intervention in the postpartum is vital, but the addition of yoga can optimize postpartum care and has enormous potential to be a “Best Care Practice” for postpartum care in rehabilitation.
As a mind-body intervention, yoga during pregnancy can increase birth weight, shorten labor, decrease pre-term birth, decrease instrument-assisted birth, reduce perceived pain, stress, anxiety sleep disturbances, and general pregnancy-related discomfort and quality of life physical domains.8-9
In addition to the typical physical therapy intervention for postpartum physical therapy, the MTY paradigm provides:
- self-care strategies for psychoemotional health and social engagement, increasing self-efficacy, confidence, and self-worth,
- a concise container for clinical-decision through its algorithmic programming,
- psychoemotional and neuroendocrine intervention,
- nutritional counseling and resource utilization,
- energetic adjunct therapies steeped in Ayurvedic science,
- executive functioning and cognitive support,
- epigenetic effect, and
- inter- and intrarelational development.
Postpartum integrated physical therapy care can provide more comprehensive care than rehab alone because of its multi-faceted biopsychosocial structure and systems-based model of care. Ginger’s course, Yoga as Medicine for Labor, Delivery, and Postpartum provides evidence-based methodology for prenatal and postpartum practice that streamlines clinical decision-making and intervention through introduction of a yogic model of assessment.
To learn more about Ginger’s course, visit Yoga as Medicine for Labor, Delivery, and Postpartum
Coeytauz et al., Maternal Mortality in the US: A Human Rights Failure. Contraception Editorial, March 2011. http://www.arhp.org/publications-and-resources/contraception-journal/march-2011
Kuklina E, Meikle S, Jamieson D, et al. Severe obstetric morbidity in the US, 1998–2005. Obstet Gynecol. 2009;113:293–299.
Tita ATN, Landon MB, Spong CY, et al. Timing of elective cesarean delivery at term and neonatal outcomes. NEJM. 2009;360:111–120.
Clark SL, Belfort MA, Byrum SL, Meyers JA, Perlin JB. Improved outcomes, fewer cesarean deliveries, and reduced litigation: results of a new paradigm in patient safety. Am J Obstet Gynecol. 2008;199:e1–105.e7.Abstract | Full Text | Full-Text PDF (100 KB)
Oshiro BT. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009;113:804–811.
Buttner, M. M., Brock, R. L., O'Hara, M. W., & Stuart, S. (2015). Efficacy of yoga for depressed postpartum women: A randomized controlled trial. Complementary Therapies in Clinical Practice, 21(2), 94-100. doi:10.1016/j.ctcp.2015.03.003 [doi]
WORLD HEALTH ORGANIZATION., 2002. Towards a common language for functioning, disability and health : ICF. Geneva: World Health Organisation.
Curtis, K., Weinrib, A., & Katz, J. (2012). Systematic review of yoga for pregnant women: Current status and future directions. Evidence-Based Complementary and Alternative Medicine : ECAM, 2012, 715942. doi:10.1155/2012/715942 [doi]
Sharma, M., & Branscum, P. (2015). Yoga interventions in pregnancy: A qualitative review. Journal of Alternative and Complementary Medicine (New York, N.Y.), 21(4), 208-216. doi:10.1089/acm.2014.0033 [doi]
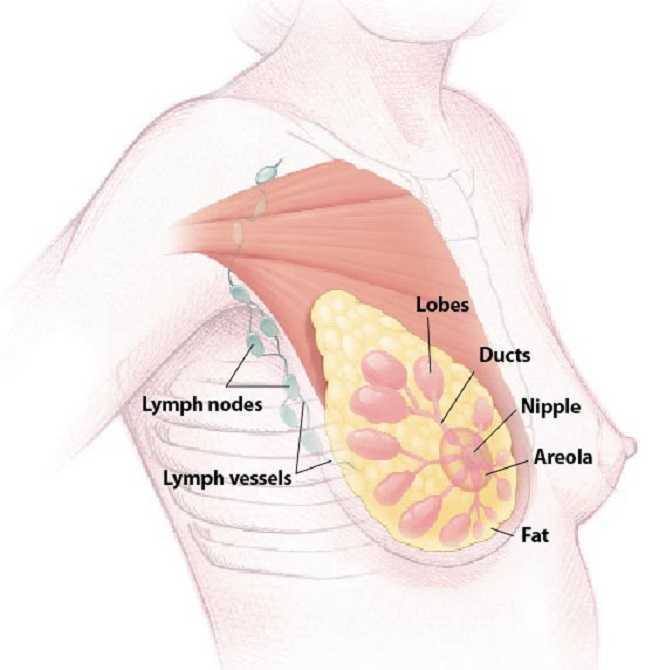
The American Society of Clinical Oncology convened their 2016 annual meeting over the weekend, and several of the presentations suggest new methods of preventing breast cancer recurrence.
Extended Hormone Therapy Reduces Recurrence of Breast Cancer
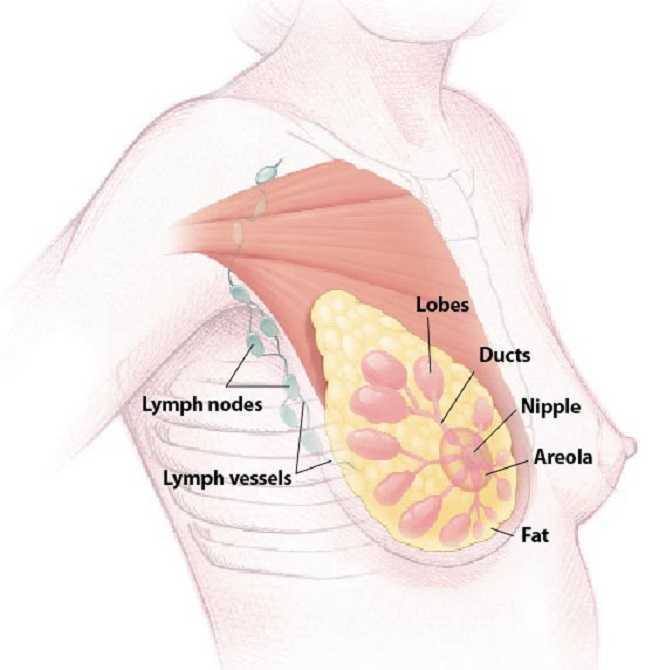 Breast cancer patients who are treated with aromatase inhibitor therapy are generally prescribed the the estrogen drugs for a five year course. A new study has suggested that by doubling the length of hormone therapy, the recurrence rate for breast cancer survivors drops by 34%. The study included 1,918 women who underwent five years of hormone therapy with the drug letrozole. After five years, half of the group switched to a placebo while the other half were given an additional five year treatment.
Breast cancer patients who are treated with aromatase inhibitor therapy are generally prescribed the the estrogen drugs for a five year course. A new study has suggested that by doubling the length of hormone therapy, the recurrence rate for breast cancer survivors drops by 34%. The study included 1,918 women who underwent five years of hormone therapy with the drug letrozole. After five years, half of the group switched to a placebo while the other half were given an additional five year treatment.
Drug Used to Treat Type 2 Diabetes May Increase Breast Cancer Survivability
The Univerisity of Pennsylvania School of Medicine has published results from two recent studies which document the effects of Metformin, a drug commonly used to treat type 2 diabetes, on breast cancer and endometrial hyperplasia. The study tracked outcomes for 1,215 patients who were diagnosed and surgically treated for breast cancer. Patients who began to use metformin after their diagnosis were found to have a 50% higher survivability rate than those who did not use metformin.
The timing of metformin use is extremely important when it comes to breast cancer survivability rates. The study also found that patients who used metformin prior to their diagnosis were more than twice as likely to die than those who never used the drug.
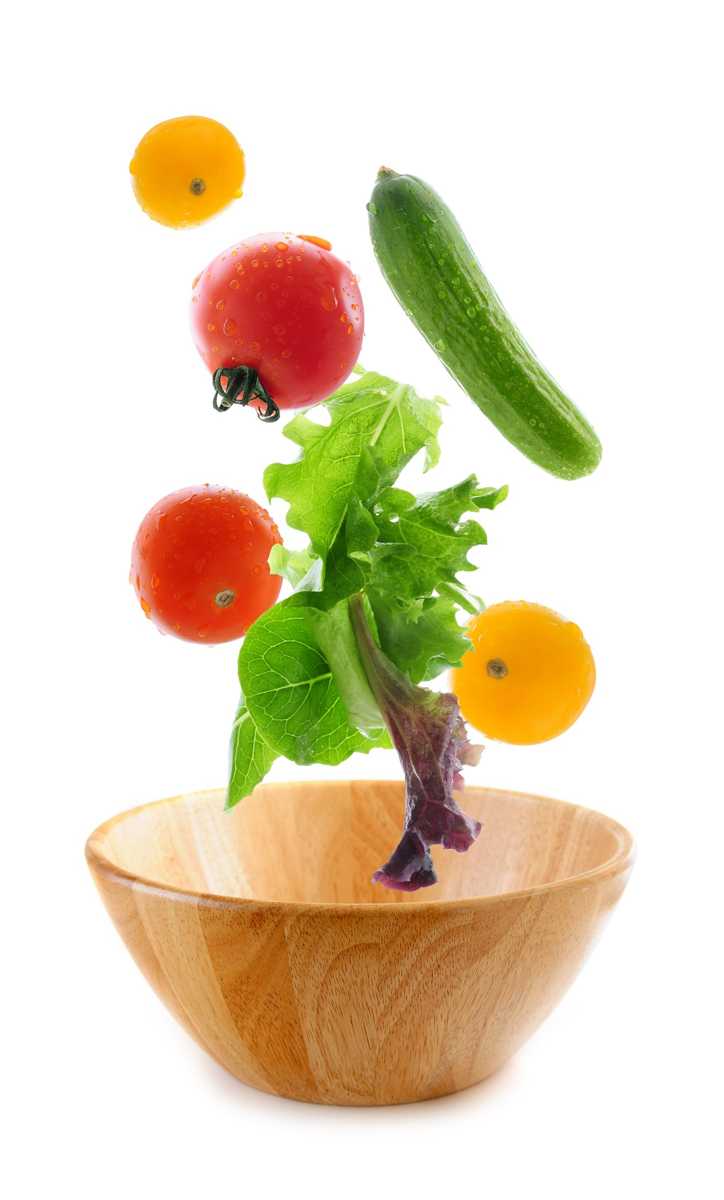
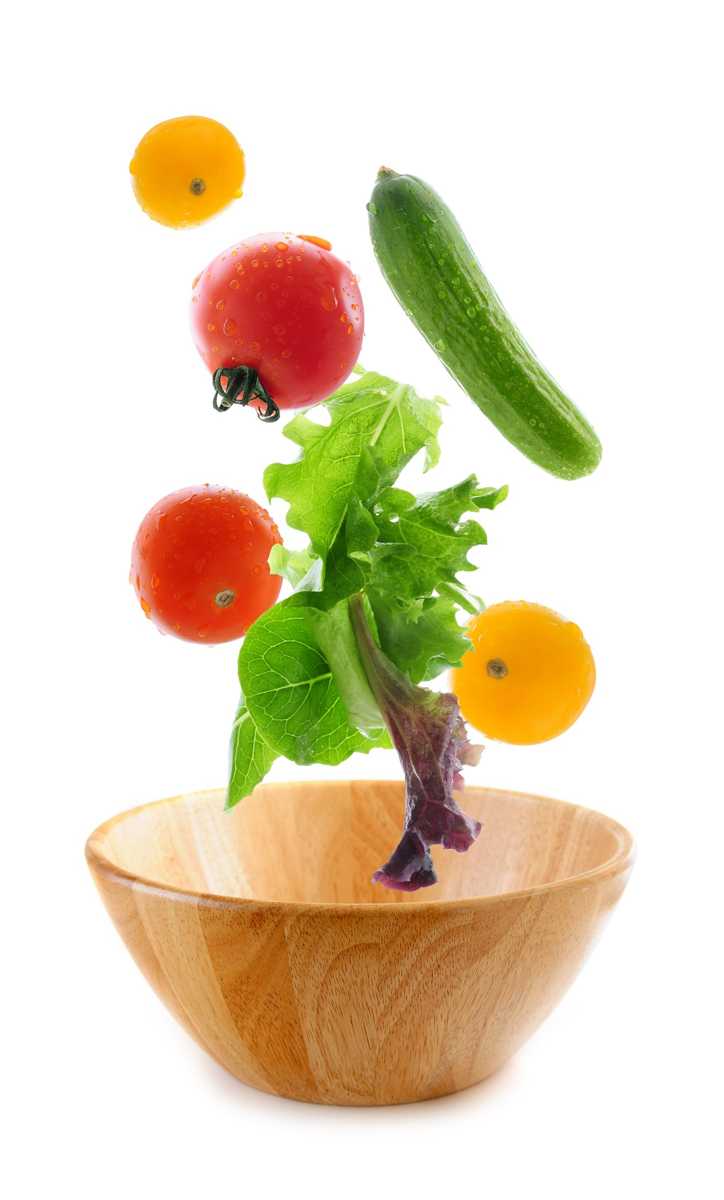
Research Suggests a "Mediterranian Diet" May Reduce Breast Cancer Recurrence
A study has indicated that a diet rich in vegetables, fish, and olive oil may decrease the odds of a breast cancer survivor experiencing a relapse or recurrence of their cancer. The study tracked 300 women with early-stage cancer and found that those who ate a normal diet were more likely to experience a breast cancer recurrence. The findings build upon previous research which indicated that a Mediterranean diet, and especially extra virgin olive oil, could reduce breast cancer risk by 68%.
Want to Learn More?
Susannah Haarmann, PT, CLT, WCS is the author and instructor of Physical Therapy Treatment for the Breast Oncology Patient, a course offered through the Herman & Wallace Institute. This continuing education course for medical practitioners offers a rehabilitation perspective for providers who work with oncology rehabilitation patients. Join Dr. Haarmann this in Stockton, CA on September 24-25 to learn evaluation and treatment techniques necessary to make an outpatient therapist an essential member of any oncology team.
1) Paul E. Goss, et al. J Clin Oncol 34, 2016 (suppl; abstr LBA1)
https://www.asco.org/about-asco/press-center/news-releases/ten-years-hormone-therapy-reduces-breast-cancer-recurrence
2) Yun Rose Li. University of Pennsylvania, American Society of Clinical Oncology Annual Meeting 2016
http://www.eurekalert.org/pub_releases/2016-06/uops-ddm060316.php
3) http://www.scienceworldreport.com/articles/41404/20160606/mediterranean-diet-prevent-breast-cancer-recurring.htm
When a 472 pound gentleman recently arrived for an evaluation for low back pain, he came to the clinic for me to help him, not deride him about his weight (which he complained all his doctors have already done). He claimed he had lost 120 pounds but gained back 50, and his low back was extremely painful with transitional movements and daily function. Undoubtedly, this man’s body was a battlefield for inflammation, and no matter how much manual therapy or exercise I implemented, nutrition education seemed vital. Instead of just chatting about baseball or the weather, competently sharing what we’ve studied and learned in continuing education courses is warranted in our practice.
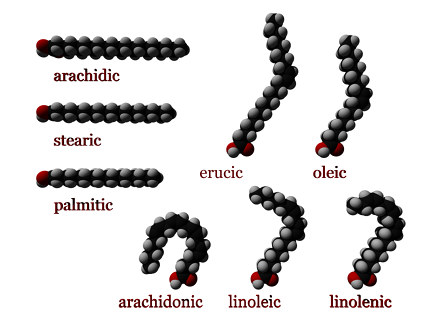 In a 2016 review Klek reveals the most current evidence regarding Omega-3 Fatty Acids in nutrition delivered intravenously. Although physical therapists do not decide the ingredients for patients’ parenteral nutrition, the article thoroughly explains the essential benefits of fatty acids. Aside from being important structural components of cell membranes and precursors of prostaglandins and cholesterol, fatty acids regulate gene expression and adjust pathways of cells regarding inflammation and cell-mediated immune responses. Ultimately, fatty acids modulate metabolic processes in the body, whether locally, in a particular region, or at remote sites. Omega-3 fatty acids have been shown to inhibit synthesis of triglycerides by the liver, prevent cardiovascular disease, reduce cancerous cell growth, and even affect the development of rheumatoid arthritis and Chrohn’s disease. This article not only sheds light on parenteral nutrition for post-surgical, oncology, critically ill, and even pediatric patients but also educates the healthcare professional on the impact fatty acids have on the patients we treat.
In a 2016 review Klek reveals the most current evidence regarding Omega-3 Fatty Acids in nutrition delivered intravenously. Although physical therapists do not decide the ingredients for patients’ parenteral nutrition, the article thoroughly explains the essential benefits of fatty acids. Aside from being important structural components of cell membranes and precursors of prostaglandins and cholesterol, fatty acids regulate gene expression and adjust pathways of cells regarding inflammation and cell-mediated immune responses. Ultimately, fatty acids modulate metabolic processes in the body, whether locally, in a particular region, or at remote sites. Omega-3 fatty acids have been shown to inhibit synthesis of triglycerides by the liver, prevent cardiovascular disease, reduce cancerous cell growth, and even affect the development of rheumatoid arthritis and Chrohn’s disease. This article not only sheds light on parenteral nutrition for post-surgical, oncology, critically ill, and even pediatric patients but also educates the healthcare professional on the impact fatty acids have on the patients we treat.
In 2015, Haghiac et al. performed a randomized double-blind controlled clinical trial to determine if Omega-3 fatty acid supplementation could reduce inflammation in pregnant woman who are obese. Although the study began with 36 subjects in each group, only 24 women in the experimental group receiving 4 capsules a day of Omega-3 fatty acid (total of 2000mg) and 25 of the women taking 4 placebo capsules a day completed the supplementation over the 25 weeks up until delivery. The authors referenced the findings that low grade inflammation becomes exacerbated in obese pregnant women. While an excess of Omega-6 fatty acids practically promotes inflammation via eicosanoid (hormone) production, a healthy balance of Omega-3 fatty acids lessens inflammatory and immunosuppressive eicosanoid production. This study demonstrated an improvement in inflammation in the women who took the Omega-3 fatty acid as evidenced by a decrease in the expression of inflammatory genes in adipose tissue and placenta as well as reduced plasma C-reactive protein (CRP) at delivery.
Being able to control or reduce inflammation on a cellular level through nutrition could promote an exciting cycle of positive events for obese patients. Decreased inflammation in the body could decrease pain, which could allow and even promote increased activity and likely boost metabolism to equip them to battle obesity. The “Nutrition Perspectives for the Pelvic Rehab Therapist” course should spark the interest of any therapist wanting to guide patients not only on movement and function but also on the appropriate nutrition that best facilitates the body’s ability to heal and perform.
To learn more about nutrition and it's effects on pelvic rehabilitation, check out Nutrition Perspectives for the Pelvic Rehab Therapist this month in Lodi, CA.
Klek, S. (2016). Omega-3 Fatty Acids in Modern Parenteral Nutrition: A Review of the Current Evidence. Journal of Clinical Medicine, 5(3), 34. http://doi.org/10.3390/jcm5030034
Haghiac, M., Yang, X., Presley, L., Smith, S., Dettelback, S., Minium, J., … Hauguel-de Mouzon, S. (2015). Dietary Omega-3 Fatty Acid Supplementation Reduces Inflammation in Obese Pregnant Women: A Randomized Double-Blind Controlled Clinical Trial. PLoS ONE, 10(9), e0137309. http://doi.org/10.1371/journal.pone.0137309
 The following guest post comes to us from Angie Johnson, a physical therapist with Kaiser Permanente in Portland, OR.
The following guest post comes to us from Angie Johnson, a physical therapist with Kaiser Permanente in Portland, OR.
Did you know that the pelvic floor muscles are actually quite thin? “Pelvic floor muscles are able to produce enough force to overcome changes in intra-abdominal pressure during less rigorous activities of daily living,“ but in activities such as coughing and jumping, “intra-abdominal pressure clearly exceeds the maximum force generated by pelvic floor muscles alone.”1 But we know that people are continent of urine during these activities, so it begs to question what structures help support the pelvic floor during high force events?
In our journey of pelvic rehabilitation and evidence-based medicine, researchers have determined that contributors to pelvic floor function include trunk stabilization2 and co-contraction of the abdominal wall (especially transverse abdominus)3,4. But this is only the beginning of the story. To add to this picture, new research, recently published in the Journal of Women’s Health Physical Therapy (January/April 2016) validates what we as practitioners already know; hip muscles play a crucial role in optimal pelvic floor functioning.
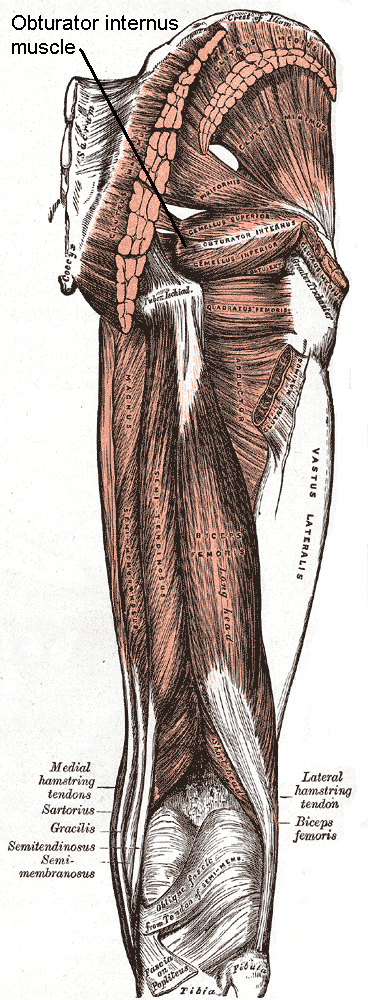
Knowledge of the anatomy of the pelvic floor and hip musculature helps to give us more understanding of the continence mechanism during high force activity. Obturator internus, which can be easily palpated through the vaginal wall “acts to externally rotate the hip. Interesting, this muscle actually shares a fascial attachment with the pelvic floor muscles.”
Researchers from a team at San Diego State University asked the very pertinent question: If you strengthen obturator internus do you strengthen the pelvic floor muscles too? To answer this question, they conducted a randomized control trial of 40 nulliparous women, aged 18-35, who were assigned to a hip exercise or control group. Both hip external rotator strength and pelvic floor muscle strength (via the Peritron™ perineometer) were measured in all of the women. The exercise group was then asked to perform clamshell exercises, isometric wall external rotation and “monster walks” as their specific hip exercises. The prescription of the exercises were 3 sets of 10 repetitions 3 days per week for 12 weeks. One session each week was supervised in the laboratory to ensure proper execution.
After the 12 weeks, the exercise group had an increase in hip external rotation strength, but also in pelvic floor muscle peak pressure. That was without any specific pelvic floor strengthening exercises at all. Strengthen the hips by doing these three exercises, and pelvic floor strength increases!! This is exciting and fantastic news for us as pelvic floor therapists and a good message to convey to our patients.
The results of this study are preliminary, but if you are treating pelvic floor weakness, hip external rotation strengthening exercises in addition to the traditional kegel strengthening exercises are a must. Go ahead – let’s all get hippie!
Tuttle LJ, DeLozier ER, Harter KA et al. The Role of the Obturator Internus Muscle in Pelvic Floor Function. Journal of Women’s Health Physical Therapy. 2016; 40, 1 pg 15-19
Sapsford R. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther 2004;9(1):31-42
Sapsford RR, Hodges PW, Ricahrdson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neruourol Urodyn 2001;20(1):3-12
Sapsord RR, Hodges PW. Contraction of the pelvic floor muscles during abdominal maneuvers. Arch Phys Med REhabil. 2001;82(8):1081-1088
“…visceral manual therapy can produce immediate hypoalgesia in somatic structures segmentally related to the organ being mobilized…”
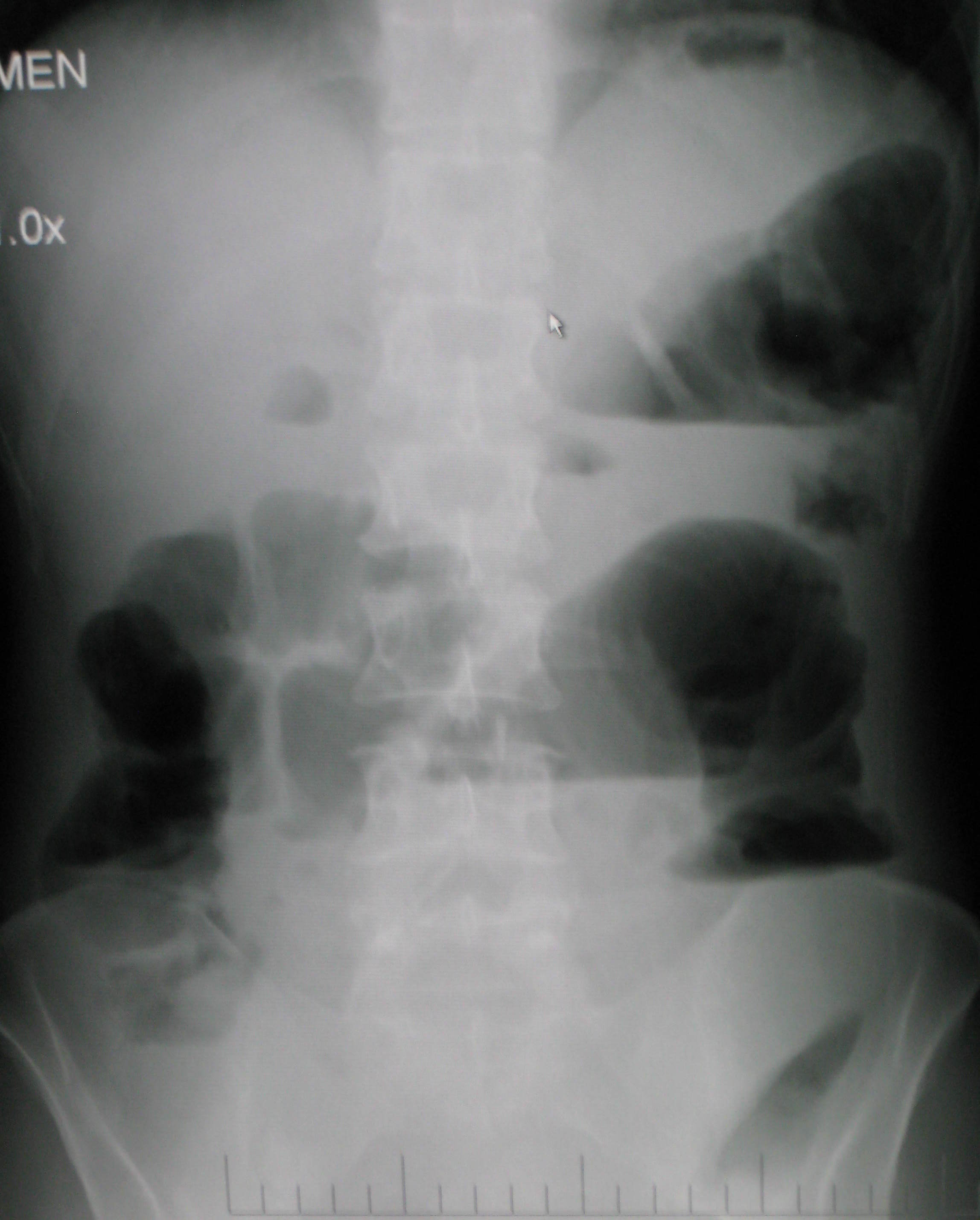
This statement is taken from an article written by MCSweeney and colleagues published in the Journal of Bodywork and Movement Therapies in 2012. The authors, who state that there is a lack of research that explains underlying mechanisms for visceral mobilization, aimed to determine if visceral mobilization could produce local and/or systemic effects towards hypoalgesia. The measurement of hypoalgesia, defined by the IASP as “diminished pain in response to a normally painful stimulus,” was assessed by use of a hand-held manual digital pressure algometer for pressure pain threshold (PPT). Sixteen asymptomatic subjects were recruited from an osteopathic school and were treated on separate occasions with a visceral mobilization of the sigmoid colon, a sham intervention of manual contact on the abdomen, and a control of no intervention. Six females (mean age 23.7) and ten males (mean age 27.7) completed the single-blinded, randomized study.

The clinical practice relevance was difficult to determine, however, this study used new techniques to determine that there is an immediate and measurable effect on the body. While therapists who treat with visceral mobilization and other soft tissue techniques know that the interventions have helped their patients, having further experimental and clinical validation of the value of these techniques is critical. If you are interested in learning more about fascial approaches to easing pain and improving function in your patients, check out the courses offered by faculty member Ramona Horton.
Ramona will be teaching her Mobilization of the Myofascial Layer: Pelvis and Lower Extremities course three times this year, with the next event in Nashua, NH June 3-5. Her Mobilization of Visceral Fascia: The Urinary System course is available three times as well, next in Kirkland, WA on June 24-26. If you're ready for the advanced course, and some wine tasting(!), check out Mobilization of Visceral Fascia: The Reproductive System of Men and Women on October 14-16 in Medford, OR.
McSweeney, T. P., Thomson, O. P., & Johnston, R. (2012). The immediate effects of sigmoid colon manipulation on pressure pain thresholds in the lumbar spine. Journal of bodywork and movement therapies, 16(4), 416-423.
In Megan Pribyl’s course on Nutrition Perspectives for the Pelvic Rehab Therapist, she discusses a wide variety of useful topics specific to nutrition and pelvic health. In her lecture on “Nutritional Homeostasis”, Megan counsels against missing an underlying eating disorder when working with a patient who has bowel issues. Work by Abraham and Kellow (2013) is cited, and in their article published in BMC Gastroenterology, the authors concur that many patients who have functional gastrointestinal complaints may also have disordered eating. How then, can we tell these patients apart, and get patients the most appropriate care? First let’s look at their research.
 Patients who were admitted to a specialty unit for those with eating disorders in Australia were studied and were found to have conditions such as anorexia nervosa, bulimia nervosa, polycystic ovarian syndrome, treated celiac disease, and treated bipolar depression. All of the 185 patients completed the Rome II Modular Questionnaire to identify symptoms consistent with functional gastrointestinal (GI) dysfunction. They also completed the Eating and Exercise Examination which collected data about behaviors including objective binge eating, self-induced vomiting, laxative use and excessive exercise.
Patients who were admitted to a specialty unit for those with eating disorders in Australia were studied and were found to have conditions such as anorexia nervosa, bulimia nervosa, polycystic ovarian syndrome, treated celiac disease, and treated bipolar depression. All of the 185 patients completed the Rome II Modular Questionnaire to identify symptoms consistent with functional gastrointestinal (GI) dysfunction. They also completed the Eating and Exercise Examination which collected data about behaviors including objective binge eating, self-induced vomiting, laxative use and excessive exercise.
Esophageal discomfort (heartburn and chest pain of non cardiac origin) was associated with excess exercise (more than 5 days/week). Self-induced vomiting was identified primarily in the patients diagnosed with bulimia. One interesting finding the researchers noted is that for patients who have disorder eating, pelvic floor symptoms that are not associated with functional constipation are a prominent feature. This data begs the question, how can we best screen for disordered eating in patients who present with bowel dysfunction that otherwise may fit with the symptoms and presentation of patients who do not have disordered eating?
Our first step may be to include important conditions and symptoms on our written or computer-based intake forms. Is “disordered eating” or bulimia, anorexia-nervosa included on your intake forms for patients? What about symptoms like heartburn, laxative use, or vomiting? (As an important aside, I always remember being surprised by a patient who had urinary incontinence when she told me that she leaked with vomiting. She had gone through a gastric bypass surgery and would vomit several times per week as a reaction to difficulty digesting food. There may be a few good reason therefore to include vomiting on a checklist.) As pelvic rehab providers, we can understand how frequent vomiting may lead to dehydration, intrabdominal and intrapelvic pressure, potential pelvic floor dysfunction, or how disordered eating may lead to other bowel dysfunctions such as constipation and/or fecal incontinence. If we also hold space for eating issues to be a concern, we may find that asking some valuable questions provides more information.
If you would like to learn more about nutrition and the pelvic health connections, you still have time to sign up for Megan Pribyl’s nutrition course which takes place in Lodi, California this June!.
Abraham, S., & Kellow, J. E. (2013) "Do the digestive tract symptoms in eating disorder patients represent functional gastrointestinal disorders?" BMC gastroenterology, 13(1), 1.
If an infomercial played in pre-op waiting rooms explaining all the possible side effects or problems a patient may encounter after surgery, I wonder how many people would abort their scheduled mission. As if having an abdominal or pelvic surgery were not enough for a patient to handle, some unfortunate folks wind up with small bowel obstruction as a consequence of scar tissue forming after the procedure. Instead of having yet another surgery to get rid of the obstruction, which, in turn, could cause more scar tissue issues, studies are showing manual therapy, including visceral manipulation, to be effective in treating adhesion-induced small bowel obstruction.
 Amanda Rice and colleagues published a paper in 2013 on the non-surgical, manual therapy approach to resolve small bowel obstruction (SBO) caused by adhesions as evidenced in two case reports. One patient was a 69 year old male who had 3 hernia repairs and a laparotomy for SBO with resultant abdominal scarring and 10/10 pain on the visual analog scale. The other patient was a 49 year old female who endured 7 abdominopelvic surgeries for various issues over the course of 30 months and presented with 7/10 pain and did not want more surgical intervention for SBO. Both patients received 20 hours of intensive manual physical therapy over a period of 5 days. The primary focus was to reduce adhesions in the bowel and abdominal wall for improved visceral mobility, but treatment also addressed range of motion, flexibility, and postural strength. The female patient reported 90% improvement in symptoms, with significant decreases in pain during bowel movements or sexual intercourse, and the therapist noted increased visceral and myofascial mobility. Both patients were able to avoid further abdominopelvic surgery for SBO, and both patients were still doing well at a one year follow up.
Amanda Rice and colleagues published a paper in 2013 on the non-surgical, manual therapy approach to resolve small bowel obstruction (SBO) caused by adhesions as evidenced in two case reports. One patient was a 69 year old male who had 3 hernia repairs and a laparotomy for SBO with resultant abdominal scarring and 10/10 pain on the visual analog scale. The other patient was a 49 year old female who endured 7 abdominopelvic surgeries for various issues over the course of 30 months and presented with 7/10 pain and did not want more surgical intervention for SBO. Both patients received 20 hours of intensive manual physical therapy over a period of 5 days. The primary focus was to reduce adhesions in the bowel and abdominal wall for improved visceral mobility, but treatment also addressed range of motion, flexibility, and postural strength. The female patient reported 90% improvement in symptoms, with significant decreases in pain during bowel movements or sexual intercourse, and the therapist noted increased visceral and myofascial mobility. Both patients were able to avoid further abdominopelvic surgery for SBO, and both patients were still doing well at a one year follow up.
In 2016, a prospective, controlled survey based study by Rice et al., determined the efficacy of treating SBO with a manual therapy approach referred to as Clear Passage Approach (CPA). The 27 subjects enrolled in the study received this manual therapy treatment for 4 hours, 5 days per week. The CPA includes techniques to increase tissue and organ mobility and release adhesions. The therapist applied varying degrees of pressure across adhered bands of tissue, including myofascial release, the Wurn Technique for interstitial spaces, and visceral manipulation. The force used and the time spent on each area were based on patient tolerance. The SBO Questionnaire considered 6 domains (diet, pain, gastrointestinal symptoms, medication, quality of life, and pain severity) and was completed by 26 of the subjects pre-treatment and 90 days after treatment. The results revealed significant improvements in pain severity, overall pain, and quality of life. Suggestive improvements were noted in gastrointestinal symptoms as well as tissue and organ mobility via improvement in trunk extension, rotation, and side bending after treatment. Overall, the authors conclude the manual therapy treatment of SBO is a safe and effective non-invasive approach to use, even for the pediatric population with SBO.
Myofascial release and visceral manipulation can disrupt the vicious cycle of adhesions causing small bowel obstruction after abdominopelvic surgical “invasion.” Learning specific techniques we may never have thought of can make a huge impact on certain patient populations. Quality of life for our patients often depends on how willing we are to increase our own knowledge and skill base.
Rice, A. D., King, R., Reed, E. D., Patterson, K., Wurn, B. F., & Wurn, L. J. (2013). Manual Physical Therapy for Non-Surgical Treatment of Adhesion-Related Small Bowel Obstructions: Two Case Reports . Journal of Clinical Medicine, 2(1), 1–12. PubMed Link
Rice, A. D., Patterson, K., Reed, E. D., Wurn, B. F., Klingenberg, B., King, C. R., & Wurn, L. J. (2016). Treating Small Bowel Obstruction with a Manual Physical Therapy: A Prospective Efficacy Study. BioMed Research International, 2016, 7610387. http://doi.org/10.1155/2016/7610387
I lived in Seattle during my pregnancies, where practicing yoga is almost as common as drinking coffee. I never accepted my friends’ invitations to partake in a perinatal yoga classes, mostly because I do not know how to do it, and I simply ran instead. My friends reaped the benefits of the meditation and strengthening involved when it came to delivering their babies. Researchers have been trying to measure the physical benefits from performing yoga during pregnancy, both for the mother and the fetus, and scientifically support the efficacy of participating in peripartum yoga.
 In a systematic review of studies regarding yoga for pregnant women, Curtis, Weinrib, and Katz (2012) explored the literature on yoga for pregnancy. Six studies were included in the review, only 3 of which were randomized controlled trials. The aspects of yoga included in the trials were postures, breathing practices, meditation, deep relaxation, counseling on lifestyle change, and chanting and anatomy information. The programs in the trials began either between 18-20 weeks gestation or between 26-28 weeks. The yoga was practiced either 3 times per week for 30-60 minutes or 60 minutes daily. Control groups included walking, standard prenatal exercise, or general nursing care. The literature review suggested improvements were noted regarding quality of life and self-efficacy, discomfort and pain during labor, and birth weight and preterm births. Due to the limited number of trials, only a general positive commendation of yoga during pregnancy could be made from this research.
In a systematic review of studies regarding yoga for pregnant women, Curtis, Weinrib, and Katz (2012) explored the literature on yoga for pregnancy. Six studies were included in the review, only 3 of which were randomized controlled trials. The aspects of yoga included in the trials were postures, breathing practices, meditation, deep relaxation, counseling on lifestyle change, and chanting and anatomy information. The programs in the trials began either between 18-20 weeks gestation or between 26-28 weeks. The yoga was practiced either 3 times per week for 30-60 minutes or 60 minutes daily. Control groups included walking, standard prenatal exercise, or general nursing care. The literature review suggested improvements were noted regarding quality of life and self-efficacy, discomfort and pain during labor, and birth weight and preterm births. Due to the limited number of trials, only a general positive commendation of yoga during pregnancy could be made from this research.
In 2015, Jiang et al. looked at 10 randomized controlled trials from 2004 to 2014 regarding yoga and pregnancy. The authors found consistent evidence showing a positive correlation between yoga intervention and lower incidence of prenatal disorders and small gestational age. Lower levels of stress and pain as well as higher relationship scores were noted with yoga. The studies showed yoga to be a safe and effective means of exercise during pregnancy, but the authors agreed further randomized controlled studies still need to be performed.
A 2015 randomized control trial by Rakhshani et al. examined the effect of yoga on utero-fetal-placental circulation during pregnancy considered high-risk. The yoga group consisted of 27 women who received standard care plus 60 minute yoga sessions 3 times per week and practice at home. The control group included 32 women who received standard care and walked 30 minutes in the morning and evening. The intervention began at the 13th week of gestation and concluded at the end of the 28th week. Yoga intervention involved yoga postures, relaxation and breathing exercises, and visualization with guided imagery. The authors conceded larger studies need to be performed to confirm the results of their randomized controlled trial; however, they concluded yoga visualization and guided imagery can significantly improve uteroplacental and fetoplacental circulation.
Although further studies are needed to make evidence-based claims regarding yoga during pregnancy, the general consensus deems yoga appropriate and safe. As with any exercise program, a tailored approach for each individual is prudent. Yoga includes many components, and current trials consistently indicate the visualization/imagery aspect is safe and beneficial during pregnancy, even when high risk. In retrospect, when I had placenta previa, perhaps I should’ve traded my running shorts for yoga pants!
Curtis, K., Weinrib, A., & Katz, J. (2012). Systematic Review of Yoga for Pregnant Women: Current Status and Future Directions. Evidence-Based Complementary and Alternative Medicine : eCAM, 2012, 715942.
Jiang Q, Wu Z, Zhou L, Dunlop J, Chen P. (2015). Effects of yoga intervention during pregnancy: a review for current status. American Journal of Perinatology. 32(6):503-14..
Rakhshani, A., Nagarathna, R., Mhaskar, R., Mhaskar, A., Thomas, A., & Gunasheela, S. (2015). Effects of Yoga on Utero-Fetal-Placental Circulation in High-Risk Pregnancy: A Randomized Controlled Trial. Advances in Preventive Medicine, 2015, 373041.