Part 2: The Drama Triangle
This is part two of a three-part series on self-care and preventing practitioner burnout from faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC. Part One is available here. Jennafer is the co-author and co-instructor of the along with Nari Clemons, PT, PRPC.
Augh, I was so frustrated with myself. I fell for it again. Here’s the scenario: a patient came in suffering excruciating pain. She had been to see a pelvic health professional as well as various medical professionals and was unable to get relief and answers for her rectal pain. She was desperate and called me “her last hope.” Phrases used included, “I need you! Fix me! I hear you are a miracle worker! If you can’t help me no one can!” And just like that I took on the role of Rescuer.
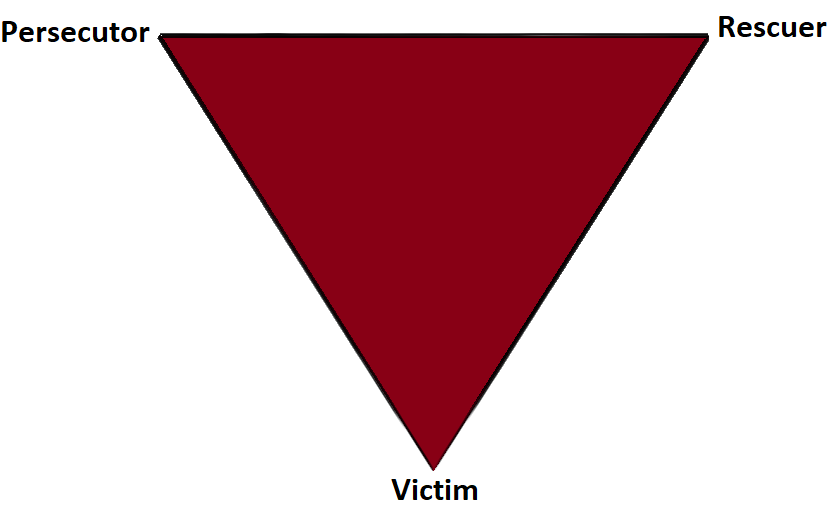
In 1968 a psychiatrist named Stephen Karpman developed a model of personal interaction that he called the Conflict Triangle. It has also become known as the Karpman Triangle, The Drama triangle or the Victim triangle. Per Wikipedia:
The Victim: The Victim's stance is "Poor me!" The Victim feels oppressed, helpless, hopeless, powerless and ashamed. They seem unable to make decisions, solve problems, take pleasure in life or achieve insight. The Victim, if not being persecuted, will seek out a Persecutor and also a Rescuer who may save the day, but may also perpetuate the Victim's negative feelings.
The Rescuer: The Rescuer's line is "Let me help you." A classic enabler, the Rescuer feels guilty if they don't rush to the rescue. Yet their rescuing has negative effects: It keeps the Victim dependent and gives the Victim permission to fail. The rewards derived from this rescue role are that the focus is taken off of the Rescuer. When they focus their energy on someone else, it enables them to ignore their own anxiety and issues. This rescue role is also pivotal because their actual primary interest is really an avoidance of their own problems disguised as concern for the victim’s needs.
The Persecutor: (a.k.a. Villain) The Persecutor insists, "It's your fault." The Persecutor is controlling, blaming, critical, oppressive, angry, authoritative, rigid, and superior.
 What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
What is interesting about this triangle is that the roles are constantly shifting. In full rescuer mode, I gladly took on this patient, intent on solving her problems. Over time, I saw that my consistent coaching for lifestyle change and self-care was falling on deaf ears. My patient was not following through with anything I asked of her; therefore my treatment plan was not working. The patient began to get frustrated with me. I then cast myself as the victim. She became my persecutor! While perhaps in her mind, I had failed as the rescuer, she was still the victim and I had become her persecutor. At the time, I did not have the skills to know how to navigate this situation in a positive or helpful way. Finally I sought the advice of my supervisor and my therapist to draw up a contract with this patient. The contract outlined each of our responsibilities. If either of us didn’t fulfill our responsibilities, the consequence would be ending our professional relationship. When she persisted, unwilling to do her part, I discharged her per our agreement.
I learned so much from this experience. Here are some things that I have implemented and may be helpful in your practice if you have similar challenges.
- In an initial visit with a new patient I explain that the patient and I make a team and we each have a role to play in reaching the patient’s goals.
- If someone says, “Fix me!” I say, “Think of me as your coach, I can show you how to help your body heal, but it’s your job to do the work.”
- When I hear, “Everyone says you are a miracle worker.” I say, “That is so kind, but it doesn’t work that way. Healing is complicated and everyone has their own journey.”
- In this way, with baby steps, we can get OUT of the drama triangle and into healthy relationships with our patients and the people in our lives.
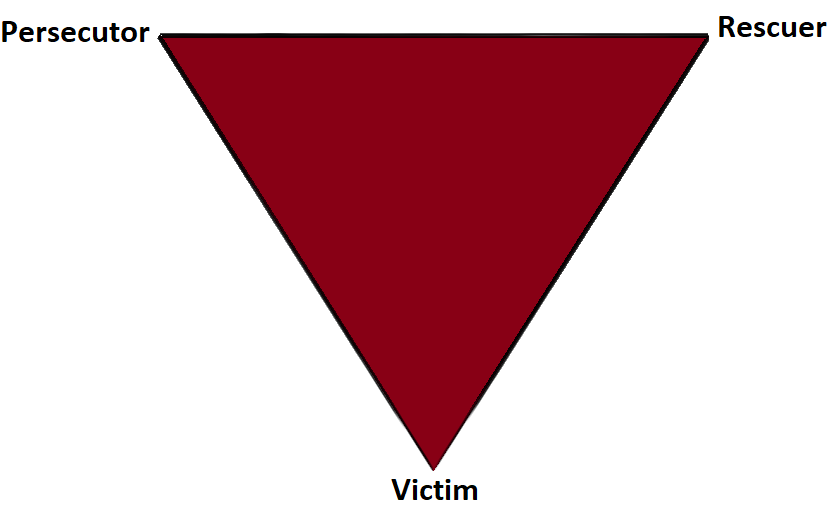
- Consider the Winner's Triangle published by Acey Choy in 1990.
In her blog NextMeCoaching, Jessica Vader coaches on turning Drama and Control into a Winning situation.
The three roles in the Winner’s Triangle.
Vulnerable – a victim should be encouraged to accept their vulnerability, problem solve, and be more self-aware.
Assertive – a persecutor should be encouraged to ask for what they want, be assertive, but not punishing.
Caring – a rescuer should be encouraged to show concern and be caring, but not over reach and problem solve for others.
If you struggle with professional and personal boundaries, you are not alone, and you can get support. Consider talking with your supervisor, a counselor, reading a good book on the subject, and or taking Boundaries, Mediation and Self Care, a course offering through Herman and Wallace that was designed to help pelvic health professionals stay healthy and inspired while equipping therapists with new tools to share with their patients.
We hope you will join us for Boundaries, Mediation and Self Care this November 9-11, 2019 in San Diego, CA.
Look forward to my next blog where saying no takes an unexpected turn.
The number of individuals who identify as transgender is growing each year. The Williams Institute estimated in 2016 that 0.6% of the U.S. population or roughly 1.4 million people identified as transgender (Flores, 2016). This was a 50% increase from a 2011 survey which estimated only 0.3% or 700,000 people identified as transgender (Gates, 2011). Though these numbers are growing each year, due to increased visibility and social acceptance, it is presumed that these numbers are underreported due to inadequate survey methods, stigma/fear associated with “coming out” and deficient definitions of the multitude of options for gender identity (Flores, 2016).

Though organizations such as WPATH have attempted to standardized care, the patient experience and reception of quality care are significantly lacking. In 2015 the National Center for Transgender Equality performed a groundbreaking survey of 27,215 respondents with the aim to “understand the lives and experiences of transgender people in the United States and the disparities that many transgender people face” (“About,”n.d., para. 1). This survey revealed that 33% of individuals who saw a health care provider had at least one negative experience related to being transgender (National Center for Transgender Equality, 2015). Negative experiences included; being refused treatment, verbal harassment, physically or sexually assault, and teaching the provider about transgender people in order to get appropriate care (National Center for Transgender Equality, 2015). Alternatively, 23% of respondents did not see a doctor when they needed to because of fear of being mistreated as a transgender person (National Center for Transgender Equality, 2015). Though these statistics are staggering and affronting there is hope for a better future.
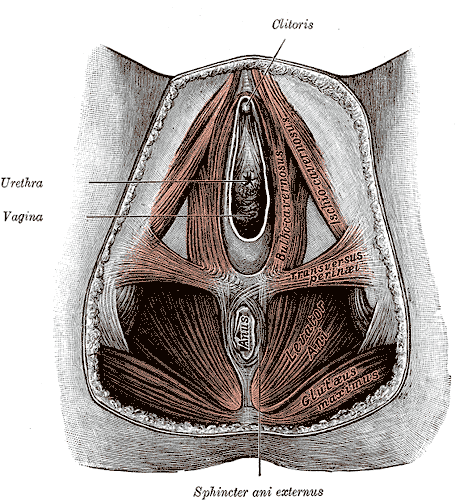
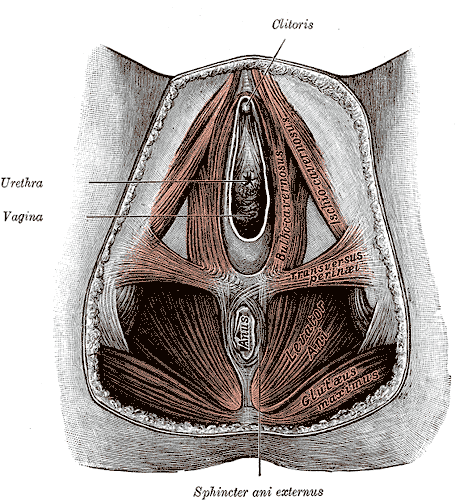
Research for the care of these patients, specifically related to pelvic floor physical therapy, is on the rise. In the Annals of Plastic Surgery, an article was published with the purpose to capture incidence and severity of pelvic floor dysfunction pre-surgery, monitor any progression of symptoms with standardized outcome measures and highlight the role of physical therapy in the treatment of patients undergoing vaginoplasty (Manrique, et al., 2019). While in the Journal of Obstetrics & Gynecology a retrospective case series similarly focused on physical therapy pre and post-operatively highlighting dilator selection and success, pelvic floor dysfunction including bowel and bladder as well as reported abuse history (Jiang, Gallagher, Burchill, Berli, & Dugi, 2019). Through articles such as these clinicians can expect an uptick in calls questioning if they treat these patients. This begs the question of, "How can you best prepare?"
The answer is simple, attend continuing education. It is where you can not only learn evidence-based evaluation and treatment but also connect with other providers and mentors that care for these patients. In 2020 Herman & Wallace will be offering a continuing education course that serves this exact purpose. Keep your eyes on next years offerings, as spaces will surely fill quickly.
About. (n.d.). Retrieved May 15, 2019, from http://www.ustranssurvey.org/about
Dora Richter. (2019, May 09). Retrieved May 15, 2019, from https://en.wikipedia.org/wiki/Dora_Richter
Jiang, D. D., Gallagher, S., Burchill, L., Berli, J., & Dugi, D. (2019). Implementation of a Pelvic Floor Physical Therapy Program for Transgender Women Undergoing Gender-Affirming Vaginoplasty. Obstetrics & Gynecology,133(5), 1003-1011. doi:10.1097/aog.0000000000003236
Manrique, O. J., Adabi, K., Huang, T. C., Jorge-Martinez, J., Meihofer, L. E., Brassard, P., & Galan, R. (2019). Assessment of Pelvic Floor Anatomy for Male-to-Female Vaginoplasty and the Role of Physical Therapy on Functional and Patient-Reported Outcomes. Annals of Plastic Surgery,82(6), 661-666. doi:10.1097/sap.0000000000001680
National Center for Transgender Equality. (2015). Annual report of the U.S. Transgender Survey. Retrieved May 15, 2019, from https://transequality.org/sites/default/files/docs/usts/USTS-Executive-Summary-Dec17.pdf
Wpath. (n.d.). Standards of Care version 7. Retrieved May 15, 2019, from https://www.wpath.org/publications/soc
Faculty member Nari Clemons, PT, PRPC recently created a two-course series on the manual assessment and treatment of nerves. The two courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are a comprehensive look at the nervous system and the various nerve dysfunctions that can impact pelvic health. The Pelvic Rehab Report caught up with Nari to discuss these new courses and how they will benefit pelvic rehab practitioners.

What is "new" in our understanding of nerves? Are there any recent exciting studies that will be incorporated into this course?
The course is loaded with a potpourri of research regarding nerves and histological and morphological studies. There are some fascinating correlations we see with nerve restrictions, wherever they are in the body. Frequently the nerves are compressed in fascial tunnels or areas of muscular overlap, then the nerve, wherever the location, frequently has local vascular axonal change, which increases the diameter of the nerve and prohibits gliding without pain. This causes local guarding and protective mechanisms. Changing pressure on the nerve can change that axonal swelling and allow gliding without pain.
New pain theory also supports that much of pain perception is the body perceiving danger or injury to a nerve. By clearing up the path of the nerve and mobilizing it, we can decrease the body's perception of nerve entrapment and thus create change in pain levels.
What do you hope practitioners will get out of this series that they can't find anywhere else?
I hope they will leave the course able to treat the nerves of the region, which is essentially the transmission pathway for most pelvic pain. I don't know of other courses that have this emphasis.
You've recently split your nerve course in two. Why the split?
I didn't want this class to be a bunch of nerve theory without the manual intervention to make change. After running the labs in local study groups, we found it took more time for people's hands to learn the language, art, and techniques of nerve work. To truly do the work justice and for participants to have a firm grasp of the manual techniques without being rushed, we found it takes time, and I wanted to honor that, as well as treating enough of the related factors and anatomy to make real and lasting change for patients.
How did you decide to divide up content?
Basically, we divided them up by anatomical origin:
The lumbar course covers the nerves of the lumbar plexus, the abdominal wall when treating diastasis, and treatment of the inguinal canal (obturator nerve, femoral nerve, iliohypogastric, ilioinguinal, genitofemoral nerves). Also, the lumbar nerves have more effect in the anterior hip, anterior pelvis, and abdominal wall.
The sacral nerve course covers all the nerves of the sacral plexus (pudendal, sciatic, gluteal/cluneal, posterior femoral cutaneous, sciatic, and coccygeal nerves), as well as subtle issues in the sacral base and subtle coccyx derangement work as well as the relationship with the uterus and sacrum, to take pressure off the sacral plexus. The sacral nerves have more effect in the posterior and inferior pelvis and into the posterior leg and gluteals.
What are the main stories that either course tells?
Both courses tell the story of getting closer to the root of the pain to make more change in less time. Muscles generally just respond to the message the nerve is sending. Yet, by treating the nerve compression directly, we are getting much closer to the root of the issue and have more lasting results by changing the source of abnormal muscle tone. Rather than an intellectual exercise of discourse on nerves, we devote ourselves to the art of manual therapy to change the restrictions on the pathway of the nerve and in the nerve itself.
If someone went to the old nerve course, what's the next best step for them?
The first course was initially all the lumbar nerves with a dip into the pudendal nerve. They would want to take the sacral nerve course, as those nerves were not covered in the first round.
Anything else you would like to share about these courses?
Sure. Essentially, we will take each nerve and do the following:
- Thoroughly learn the path of the nerve
- Fascially clear the path of the nerve
- Manually lengthen supportive structures and tunnels that surround the nerve.
- Directly mobilize the nerve
- Glide the nerve
- Learn manual local regional integration techniques for the nerve after treatment
- Receive handouts for and practice home program for strengthening and increasing mobility in the path of the nerve
Join Nari at one of the following events to learn valuable evaluation and treatment techniques for sacral and lumbar nerves
Upcoming sacral nerve courses:
Sacral Nerve Manual Assessment and Treatment - Winfield, IL
Oct 11, 2019 - Oct 13, 2019
Sacral Nerve Manual Assessment and Treatment - Tampa, FL
Dec 6, 2019 - Dec 8, 2019
Upcoming lumbar nerve courses:
Lumbar Nerve Manual Assessment and Treatment - Phoenix, AZ
Jan 11, 2019 - Jan 13, 2019
Lumbar Nerve Manual Assessment and Treatment - San Diego, CA
May 3, 2019 - May 5, 2019
Pain with sitting is a common complaint that patients may present to the clinic with. While excess sitting has been shown to be detrimental to the human body, sitting is part of our everyday culture ranging from sitting at a meal, traveling in the car, or doing work at a desk. Often, physical therapists disregard the coccyx or tailbone as the possible pain generator, simply because they are fearful of assessing it, have no idea where it is, or have never learned about it being a pain generator in their education.
Coccydynia is the general term for “pain over the coccyx.” Patients with coccydynia will complain of pain with sitting or transitioning from sit to stand. Despite the coccyx being such a small bone at the end of the spine, it serves as a large attachment site for many important structures of interest that are important in pelvic floor support and continence: ¹
- Anterior: Levator ani muscles, Sacrococcygeal ligament
- Lateral: Coccygeal muscles, Sacrospinous ligament, Sacrotuberous ligament, Glute maximus muscle fibers
- Inferiorly: Iliococcygeus
 Along with serving as a major attachment site for the above structures it provides a support for weightbaring in the seated position and provides structural support for the anus. Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall, or an internal trauma like a difficult childbirth. 1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulting in coccyx pain were from use of instruments such as a forceps delivery or vacuum assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction. ¹ When assessing a patient with coccyx pain, it is also of the upmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retrorectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign, and if excision is necessary. Sometimes these masses can be felt as a bulge on rectal examination. 4,5
Along with serving as a major attachment site for the above structures it provides a support for weightbaring in the seated position and provides structural support for the anus. Women are five times more likely to develop coccydynia than men, with the most common cause being an external trauma like a fall, or an internal trauma like a difficult childbirth. 1,2 In a study of 57 women suffering from postpartum coccydynia, most deliveries that resulting in coccyx pain were from use of instruments such as a forceps delivery or vacuum assisted delivery. A BMI over 27 and having greater than or equal to 2 vaginal deliveries resulted in a higher rate of coccyx luxation during birth. ³ Other causes of coccyx pain can be non traumatic such as rapid weight loss leading to loss of cushioning in sitting, hypermobility or hypomobility of the sacrococcygeal joint, infections like a pilonidal cyst, or pelvic floor muscle dysfunction. ¹ When assessing a patient with coccyx pain, it is also of the upmost importance to rule out red flags, as there are multiple cases cited in the literature of tumors such as retrorectal tumors or cysts being the cause of coccyx pain. These masses must be examined by a doctor to determine if they are malignant or benign, and if excision is necessary. Sometimes these masses can be felt as a bulge on rectal examination. 4,5
A multidisciplinary approach including physical therapy, ergonomic adaptations, medications, injections, and, possibly, psychotherapy leads to the greatest chance of success in patients with prolonged coccyx pain. 1 Special wedge shaped sitting cushions can provide relief for patients in sitting and help return them to their social activities during treatment. Physical therapy includes manual manipulation and internal work to the pelvic floor muscles to alleviate internal spasms and ligament pain. Intrarectal coccyx manipulation can potentially realign a dislocated sacrococcygeal joint or coccyx. 1 Taping methods can be used as a follow up to coccyx manipulation to help hold the coccyx in the new position and allow for optimal healing. Often coccyx pain patients have concomitant pathologies such as pelvic floor muscle dysfunction, sacroilliac or lumbar spine pain, and various other orthopedic findings that are beneficial to address. When conservative treatments fail, injections or a possible coccygectomy may be considered.
Luckily conservative treatment is successful in about 90% of cases. ¹ All of the above conservative tools will be taught in the upcoming Coccyx Pain Evaluation and Treatment course on April 23-24th, 2016 in Columbia, MO taught by Lila Abbate PT, DPT, OCS, WCS, PRPC. By learning how to treat coccyx pain appropriately, you will be a key provider in solving many unresolved sitting pain cases that are not resolved with traditional orthopedic physical therapy.
1. Lirette L, Chaiban G, Tolba R, et al. Coccydynia: An overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner Journal. 2014; 14:84-87.
2. Marinko L, Pecci M. Clinical Decision Making for the Evaluation and Management of Coccydynia: 2 Case Reports. JOSPT. 2014; 44(8): 615
3. Maigne JY, Rusakiewicz F, Diouf M. Postpartum coccydynia: a case series study of 57 women. Eur J Phys Rehabil Med. 2012; 48 (3): 387-392.
4. Levine R, Qu Z, Wasvary H. Retrorectal Teratoma. A rare cause of pain in the tailbone. Indian J Surg. 2013; 75(2): 147-148.
5. Suhani K, Ali S, Aggarwal L, et al. Retrorectal cystic hamartoma: A problematic tail. J Surg Tech Case Rep. 2104; 6(2): 56-60.
Scientists at the National University of Ireland in Maynooth reported the detection of a protein, Pellino3 that may stop Crohn's disease from developing. The Irish Times article, University breakthrough in fight against Crohn's disease, described the benefit as diagnostic: [Researchers] will now use the protein as a basis for new diagnostic for Crohn's and as a target in designing drugs to treat the illness.
Researchers noticed that levels of Pellino3 are dramatically reduced in Crohn's disease patients. Prof. Paul Moynagh, who led the researchers, believes that identifying Pellino3s role in Crohn's disease may lead to better treatments for other inflammatory bowel diseases.
In the United States, more than a half-million people suffer from Crohn's disease and more than a million suffer from some type of inflammatory bowel disease. Symptoms often include abdominal pain and diarrhea. These symptoms are often debilitating and even life-threatening. There is neither a known cause nor cure for Crohn's disease.
Therapy has been known as one of the few treatments that can reduce symptoms and even lead to remission.
Hopefully, this discovery will lead to further advancements in treating Crohn's disease: The findings by Prof Moynagh and his team have the potential to impact positively on many lives.
Reports in the media of research on mindfulness keep reminding us that mindfulness has positive effects on a wide variety of conditions. In the world of pelvic rehabilitation, which is broad when we consider the scope of the patient populations and diagnoses that we treat, we can find benefits from mindfulness to include bladder dysfunction, pain, and even bowel dysfunction. When specifically addressing bowel dysfunction, there are many studies that promote the benefits of mindfulness on bowel health, including the following research findings for the following topics:
Colitis
In 53 patients diagnosed with ulcerative colitis (UC), some were randomized into a control group or a treatment arm that consisted of instruction in mindfulness-based stress reduction (MBSR). While mindfulness-based stress reduction did not, in this study, affect the flare-ups of patients with moderately severe ulcerative colitis, the MBSR “…had a significant positive impact on the quality of life…” when compared to patients in the control group. So even though the use of mindfulness did not appear to affect the disease, the patients utilizing mindfulness perceived a higher quality of life even during a flare of their colitis. (Jedel et al., 2014)
Irritable Bowel Syndrome (IBS)
In another study, 36 people (24 diagnosed with irritable bowel syndrome (IBS) and 12 healthy subjects in control group) were studied. The patients who had IBS were divided into equal groups and were treated with either CBT (cognitive behavioral therapy) or MBT (mindfulness-based treatment.) The authors conclude that mindfulness-based therapy “…is an effective method to decrease symptoms of patients with IBS…” and that it was more effective than CBT at the 2 month follow-up. (Zomorodi et al., 2014)
Irritable Bowel Disease (IBD)
In reference to the importance of addressing mind, body and spirit for patients who have inflammatory bowel disease, this article discusses the benefits of addressing the psychosocial impacts of gastrointestinal disorders, as the disorders are “…best understood by a combination of genetic, physical, physiological, and psychological factors.” (Jedel et al., 2012)
Functional Gastrointestinal (GI) Disorders
Although a recent analysis of studies on gastrointestinal disorders calls for improvement in methodological quality of the research, the article concludes that “…mindfulness-based interventions may be useful in improving FGID [functional gastrointestinal disorders] symptom severity and quality of life with lasting effects…” (Aucoin et al., 2014)
From these few studies we can see that mindfulness is an accepted and potentially helpful adjunct in improving patient symptoms and quality of life in those who have bowel dysfunction. Mindfulness is a tool that every therapist should have in the toolbox for offering to patients who can complete this self-care activity as part of a home program. If you’d like to learn more about how to effectively instruct in mindfulness, you still have time to register for the Caroline McManus continuing education course on Mindfulness Based Pain Treatment, taking place January 16-17 in Silverdale, Washington, on the beautiful peninsula.
Aucoin, M., Lalonde-Parsi, M. J., & Cooley, K. (2014). Mindfulness-Based Therapies in the Treatment of Functional Gastrointestinal Disorders: A Meta-Analysis. Evidence-Based Complementary and Alternative Medicine, 2014.
Jedel, S., Hankin, V., Voigt, R. M., & Keshavarzian, A. (2012). Addressing the mind, body, and spirit in a gastrointestinal practice for inflammatory bowel disease patients. Clinical Gastroenterology and Hepatology, 10(3), 244-246.
Jedel, S., Hoffman, A., Merriman, P., Swanson, B., Voigt, R., Rajan, K. B., ... & Keshavarzian, A. (2014). A randomized controlled trial of mindfulness-based stress reduction to prevent flare-up in patients with inactive ulcerative colitis. Digestion, 89(2), 142-155.
Zomorodi, S., Abdi, S., & Tabatabaee, S. K. R. (2014). Comparison of long-term effects of cognitive-behavioral therapy versus mindfulness-based therapy on reduction of symptoms among patients suffering from irritable bowel syndrome. Gastroenterology and Hepatology from bed to bench, 7(2), 118.
Depression and anxiety can limit ability to care for one’s self, limit ability to care for a new baby or developing fetus, and can cause mood swings, impaired concentration, and sleep disturbance. Disorders of depression and anxiety are common in the perinatal period (immediately before and after birth) with depression rates around 20% and perinatal anxiety present in about 10% of women. These mood disorders greatly diminish quality of life for mother and baby. Medication may be effective, however, side effects are often unknown, and potentially adverse for the perinatal patient. Many women worry that using medication to treat these disorders may harm the fetus, negatively affect mother child bonding, and poorly influence child development. As health care providers, being aware of alternative treatments for depression and anxiety is essential. Having alternative treatments can allow our patients to combat these common perinatal problems which will improve quality of life, improve bonding between baby and mother and improve the overall perinatal experience. In the general population, positive mental and physical health benefits have been continually demonstrated by yoga participants in current research. Can yoga be an effective, alternative treatment to help perinatal patients improve mental health and well-being?
 A recent 2015 systematic literature review published in the Journal of Holistic Nursing reviewed 13 studies to examine existing empirical literature on yoga interventions and yoga’s effects on pregnant women’s health and well-being. The conclusion of the review found that yoga interventions were generally effective at reducing depression and anxiety in perinatal women and the decrease in depression and anxiety was noted regardless of the type of outcome measure used and results were optimized when the study was 7 weeks or longer. Other positive secondary findings noted with the regular yoga participation in the perinatal participants were: improvements in pain, anger, stress, gestational age at birth, birth weight, maternal-infant attachment, power, optimism, and well-being. What is yoga and what form of it may help battle perinatal depression and anxiety?
A recent 2015 systematic literature review published in the Journal of Holistic Nursing reviewed 13 studies to examine existing empirical literature on yoga interventions and yoga’s effects on pregnant women’s health and well-being. The conclusion of the review found that yoga interventions were generally effective at reducing depression and anxiety in perinatal women and the decrease in depression and anxiety was noted regardless of the type of outcome measure used and results were optimized when the study was 7 weeks or longer. Other positive secondary findings noted with the regular yoga participation in the perinatal participants were: improvements in pain, anger, stress, gestational age at birth, birth weight, maternal-infant attachment, power, optimism, and well-being. What is yoga and what form of it may help battle perinatal depression and anxiety?
Yoga by definition is a Hindu philosophy that teaches a person to experience inner peace by controlling the mind and body. Merriam-Webster defines yoga as a system of exercises for attaining bodily or mental control and well-being. All styles of yoga include some combination of physical poses, breathing techniques, and meditation-relaxation techniques. Hatha yoga is the most common form completed in the United States and consists modernly of various postures, breathing, and meditation. In the 13 reviewed studies, all interventions consisted of different forms of yoga and the overall conclusion of the systematic review was the decrease in depression and anxiety was significant no matter the form of yoga completed. Physical and emotional issues such as hormonal changes, sleep deprivation, inability to handle new tasks, self-worth, and body issues, during the perinatal period can contribute to increased anxiety and depression. As health care providers we need to have alternative treatments to help our perinatal patients’ battle depression and anxiety. Yoga is a promising alternative to medication to help decrease depression and anxiety. Additionally it may be helpful for management of pain, anger, stress, gestational age at birth, birth weight, maternal-infant attachment, power, optimism, and well-being.
Interested in learning more about how you can apply therapeutic yoga in your practice? Check out "Yoga as Medicine for Pregnancy this April in Washington, DC!
Sheffield, K. M., & Woods-Giscombé, C. L. (2015). Efficacy, Feasibility, and Acceptability of Perinatal Yoga on Women’s Mental Health and Well-Being A Systematic Literature Review. Journal of Holistic Nursing, 0898010115577976.
In a previous post on The Pelvic Rehab Report, Sagira Vora, PT, MPT, WCS, PRPC explored the impact that pelvic floor exercises can have on arousal and orgasm in women. Today we hear part two of the conversation, and learn what factors can impact a woman's ability to achieve orgasm.
 “An orgasm in the human female is a variable, transient peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary, rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
“An orgasm in the human female is a variable, transient peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary, rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
Wow, that sounds like paradise! The question is--how to get there? Many of our cohorts and many our female patients have not experienced this or orgasm happens for them rarely. Findings from surveys and clinical reports suggest that orgasm problems are the second most frequently reported sexual problems in women. Some of the reasons cited for lack of orgasm are orgasm importance, sexual desire, sexual self-esteem, and openness of sexual communication with partner by Kontula el. al. in 2016. Rowland found that most commonly-endorsed reasons were stress/anxiety, insufficient arousal, and lack of time during sex, body image, pain, inadequate lubrication.
One factor that comes up consistently, is the ability of women to focus on sexual stimuli. This point has been brought up by various studies and presented in different ways. Chambless talks about mindfulness training and improvements in orgasm ability noted equally in women who practiced mindfulness vs. women who engaged in Kegels and mindfulness. Rosenbaum and Padua note in their book, The Overactive Pelvic Floor, “women who do not have a low-tone pelvic floor and who seek to enhance sexual arousal and more frequent orgasms have not much to gain from pelvic floor muscle training. Actually, a relaxed pelvic floor and mindful attention to sexual stimuli and bodily sensations seem a more effective means of enhancing sexual arousal and orgasm.” Various studies specifically studying the effect of mindfulness training have demonstrated both improved arousal and orgasm ability in women who practiced mindfulness. Brotto and Basson found their treatment group, which consisted of 68 otherwise healthy women, who underwent mindful meditation, cognitive behavioral training and education, improved in sexual desire, sexual arousal, lubrication, sexual satisfaction, and overall sexual functioning.
Cognitive-behavioral therapy appears to play a significant role in improving sexual function in women. Meston et. al. notes, “cognitive behavioral therapy for anorgasmia focuses on promoting changes in attitudes and sexually relevant thoughts, decreasing anxiety, and increasing orgasmic ability and satisfaction. To date there are no pharmacological agents proven to be beneficial beyond placebo in enhancing orgasmic function in women.”
Alas, there are no magic pills to create the above described “state of altered consciousness,” allowing women a sense of “well-being and contentment.” However, mindfulness training and cognitive behavioral therapy are both accessible and attainable for women who want to improve their ability to enjoy this much desired state. Many Pelvic floor therapist incorporate cognitive behavioral and mindfulness approaches in their practice.
The studies above mention pain as one of the factors for inability to experience arousal and orgasm. Hucker and Mccabe even noted that their mindfulness treatment group demonstrated significant improvements in all domains of female sexual response except for sexual pain. Dealing with sexual pain is a daily battle pelvic floor therapist face each day. So, how do women with sexual pain dysfunction differ from women who are experiencing sexual dysfunction but not pain? Let’s explore this in our next blog…
Chambless DL, Sultan FE, Stern TE, O’Neill C, Garrison S. Jackson A. Effect of pubococcygeal exercise on coital orgasm in women. J Consult CLin Psychol. 1984; 52:114-8
Bratto LA, Basson R. Group mindfulness-based therapy significantly improves sexual desire in women Behav Res Ther. 2014 Jun; 57:43-5
Hucker A. Mccabe MP. Incorporating Mindfulness and Chat Groups Into an Online Cognitive Behavioral Therapy for Mixed Female Sexual Problems. J Sex Res. 2015;52(6):627-33
Kontula O., Mettienen A. Determinants of female sexual orgasms. Socioaffect Neurosci Psychol. 2016 Oct 25;6:31624. doi: 10.3402/snp.v6.31624. eCollection 2016
Meston CM1, Levin RJ, Sipski ML, Hull EM, Heiman JR. Women’s orgasm. Annu Rev Sex Res. 2004;15:173-257. Review
Rosenbaum, Talli Y., Padoa, Anna. The overactive Pelvic floor. 1st ed. 2016
Roland DL, Cempel LM, Tempel AR. Women’s attributions on why they have difficulty reaching orgasm. J. Marital Therapy. 2018 Jan 3:0
In a previous post on The Pelvic Rehab Report Sagira Vora, PT, MPT, WCS, PRPC shared that "cognitive-behavioral therapy appears to play a significant role in improving sexual function in women". Today, in part three of her ongoing series on sex and pelvic health, Sagira explores how sexual pain affects sexual dysfunction in women.
 After having explored what allows for women to have pleasurable sexual experiences including pain-free sex and mind-blowing orgasms, we now turn towards our cohort that have pain with sex and intimacy. How does this group differ from women who do not have pain with sex? Are there some common factors with this group of women, and perhaps understanding these factors may help the pelvic floor therapist render more effective and successful treatment?
After having explored what allows for women to have pleasurable sexual experiences including pain-free sex and mind-blowing orgasms, we now turn towards our cohort that have pain with sex and intimacy. How does this group differ from women who do not have pain with sex? Are there some common factors with this group of women, and perhaps understanding these factors may help the pelvic floor therapist render more effective and successful treatment?
There are few studies exploring sexual arousal in women with sexual pain disorders. However, their findings are remarkable. Brauer and colleagues found that genital response, as measured by vaginal photoplethysmography and subjective reports, was found to be equal in women with sexual pain vs. women who did not have pain, when they were shown oral sex and intercourse movie clips. This and other studies have shown that genital response in women with dyspareunia is not impaired. Genital response in women with dyspareunia is however, effected by fear of pain. When Brauer and colleagues subjected women with dyspareunia to threat of electrical shock (not actual shock) while watching an erotic movie clip they found that women with dyspareunia had much diminished sexual response including diminished genital arousal. But Spano and Lamont found that genital response was diminished by fear of pain equally in women with sexual pain and women without sexual pain.
Fear of pain also resulted in increased muscle activity in the pelvic floor. However, this increase was noted in women with pain and women without sexual pain equally and was noted with exposure to sexually threatening film clips as well as threatening film clips without sexual content. The conclusion, then, from these results is that the pelvic floor plays a role in emotional processing and tightening, or overactivity is a protective response noted in all women regardless of sexual pain history.
The one difference that was noted was with women who had the experience of sexual abuse. For them, pelvic floor overactivity was noted when watching sexually threatening as well consensual sexual content. Women without sexual abuse history did not have increased pelvic floor activity when watching consensual sexual content.
In summary, evidence supports the hypothesis that women with sexually adverse experiences tend to have impaired genital response when in consensual sexual situations, however, women who do not have sexual abuse histories and but have sexual pain tend to have appropriate genital response. Both groups, however, have increased pelvic floor muscle activity in consensual sexual situations. This increase in pelvic floor muscle activity leads to muscle pain, reduced blood flow, reduced lubrication, increased friction between penis and vulvar skin and hence leads to pain.
This brings us to our next questions, how does the cohort that has had adverse sexual experiences present? How do women with history of sexual trauma process sexual experiences? How does the pelvic floor present or respond to consensual sexual situations when a woman has been abused in the past? Please tune in to the next blog for answers…
Blok BF, Holstege G. The neuronal control of micturition and its relation to the emotional motor system. Prog Brain Res. 1996; 107:113-26
Brauer M, Laan E, ter Kuile MM. Sexual arousal in women with superficial dyspareunia. Arch Sex Behav. 2006; 35:191-200
Brauer M, ter Kuile MM, Janssen S, Lann E. The effect of pain-related fear on sexual arousal in women with superficial dyspareunia. Eur J Pain: 2007; 11:788-98
Spano L, Lamont JA. Dyspareunia: a symptom of female sexual dysfunction. Can Nurse 1975;71:22-5
Episiotomy is defined as an incision in the perineum and vagina to allow for sufficient clearance during birth. The concept of episiotomy with vaginal birth has been used since the mid to late 1700’s and started to become more popular in the United States in the early 1900’s. Episiotomy was routinely used and very common in approximately 25% of all vaginal births in the United States in 2004. However, in 2006, the American Congress of Obstetricians and Gynecologists recommended against use of routine episiotomies due to the increased risk of perineal laceration injuries, incontinence, and pelvic pain. With this being said, there is much debate about their use and if there is any need at all to complete episiotomy with vaginal birth.
 What are the negative outcomes of episiotomy?
What are the negative outcomes of episiotomy?
The primary risks are severe perineal laceration injuries, bowel or bladder incontinence, pelvic floor muscle dysfunction, pelvic pain, dyspareunia, and pelvic floor laxity. Use of a midline episiotomy and use of forceps are associated with severe perineal laceration injury. However, mediolateral episiotomies have been indicated as an independent risk factor for 3rd and 4th degree perineal tears. If episiotomy is used, research indicates that a correctly angled (60 degrees from midline) mediolateral incision is preferred to protect from tearing into the external anal sphincter, and potentially increasing likelihood for anal incontinence.
What are the indications for episiotomy, if any?
This remains controversial. Some argue that episiotomies may be necessary to facilitate difficult child birth situations or to avoid severe maternal lacerations. Examples of when episiotomy may be used could include shoulder dystocia (a dangerous childbirth emergency where the head is delivered but the anterior shoulder is unable to pass by the pubic symphysis and can result in fetal demise.), rigid perineum, prolonged second stage of delivery with non reassuring fetal heart rate, and instrumented delivery.
On the other side of the fence, many advocate never using an episiotomy due to the previously stated outcomes leading to perineal and pelvic floor morbidity. In a recent cohort study in 2015 by Amorim et al., the question of “is it possible to never perform episiotomy with vaginal birth?” was explored. 400 women who had vaginal deliveries were assessed following birth for perineum condition and care satisfaction. During the birth there was a strict no episiotomy policy and Valsalva, direct pushing, and fundal pressure were avoided, and perineal massage and warm compresses were used. In this study there were no women who sustained 3rd or 4th degree perineal tears and 56% of the women had completely intact perineum. 96% of the women in the study responded that they were satisfied or very satisfied with their care. The authors concluded that it is possible to reach a rate of no episiotomies needed, which could result in reduced need for suturing, decreased severe perineal lacerations, and a high frequency of intact perineum’s following vaginal delivery.
Are episiotomies actually being performed less routinely since the 2006 American Congress of Obstetricians and Gynecologists recommendation?
Yes, a recent study in the Journal of the American Medical Association by Friedman, it showed that the routine use of episiotomy with vaginal birth has declined over time likely reflecting an adoption of the American Congress of Obstetricians and Gynecologists recommendations. This is ideal, as it remains well established that episiotomy should not be used routinely. However, indications for episiotomy use remain to be established. Currently, physicians use clinical judgement to decide if episiotomy is indicated in specific fetal-maternal situations. If one does receive an episiotomy then a mediolateral incision is preferred. The World Health Organization’s stance is that an acceptable global rate for the use of episiotomy is 10% or less of vaginal births. So the question still remains, (and of course more research is needed) to episiotomy or not to episiotomy?
Amorim, M. M., Franca-Neto, A. H., Leal, N. V., Melo, F. O., Maia, S. B., & Alves, J. N. (2014). Is It Possible to Never Perform Episiotomy During Vaginal Delivery?. Obstetrics & Gynecology, 123, 38S.
Friedman, A. M., Ananth, C. V., Prendergast, E., D’Alton, M. E., & Wright, J. D. (2015). Variation in and Factors Associated With Use of Episiotomy. JAMA, 313(2), 197-199.
Levine, E. M., Bannon, K., Fernandez, C. M., & Locher, S. (2015). Impact of Episiotomy at Vaginal Delivery. J Preg Child Health, 2(181), 2.
Melo, I., Katz, L., Coutinho, I., & Amorim, M. M. (2014). Selective episiotomy vs. implementation of a non episiotomy protocol: a randomized clinical trial. Reproductive health, 11(1), 66.