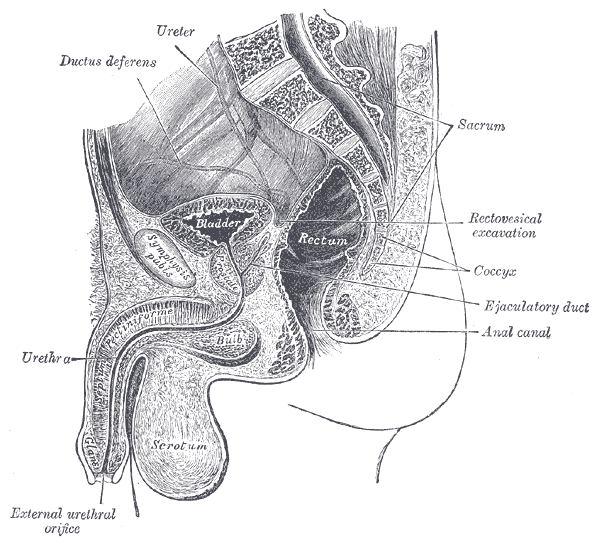
Erectile dysfunction (ED) is a debilitation complication of radical prostatectomy, which is a treatment for prostate cancer. ED is caused by a variety of causes, diabetic vasculopathy, smoking, high blood pressure, high cholesterol, psychological issues, peripheral vascular disease and medication; we will focus on post-prostatectomy ED and the role of penile rehabilitation in its management.
Post-prostatectomy-related Erectile dysfunction
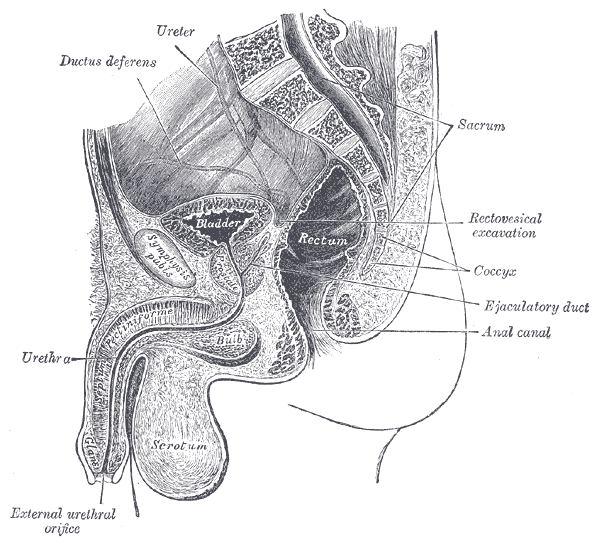 Radical prostatectomy can result in nerve injury to the penis. Moreover, significant fibrotic changes take place in the corpus cavernosum of the penis postoperatively. It takes approximately 1-2 years for erectile function to return after radical prostatectomy. This is a period of “neuropraxia,” during which there is transient cavernosal nerve dysfunction. However, a prolonged “flaccid state” might lead to irreversible damage to the cavernous tissue 1.
Radical prostatectomy can result in nerve injury to the penis. Moreover, significant fibrotic changes take place in the corpus cavernosum of the penis postoperatively. It takes approximately 1-2 years for erectile function to return after radical prostatectomy. This is a period of “neuropraxia,” during which there is transient cavernosal nerve dysfunction. However, a prolonged “flaccid state” might lead to irreversible damage to the cavernous tissue 1.
Research on penile hemodynamics in these patients have shown that venous leakage is also implicated in its pathophysiology. An injury to the neurovascular bundles likely leads to smooth muscle cell death, which then leads to irreversible veno-occlusive disease.
There is a potential role of hypoxia in stimulating growth factors (TGF-beta) that stimulate collagen synthesis in cavernosal smooth muscle. Prostaglandin E1 (PGE1) was found to suppress the effect of TGF-β1 on collagen synthesis.
Role of Penile Rehabilitation
The goal of Penile Rehabilitation is to limit and reverse ED in post-prostatectomy patients. The idea is to minimize fibrotic changes during the period of “penile quiescence” after nerve-sparing radical prostatectomy. Several approaches have been tried, including PGE1 injection, vacuum devices, and phosphodiesterase type 5 (PDE-5) inhibitors.
Mulhall and coworkers followed 132 patients through an 18-month period after they were placed in “rehabilitation” or “no rehabilitation” groups after radical prostatectomy, and 52% of those undergoing rehabilitation (sildenafil + alprostadil) reported spontaneous functional erections, compared with 19% of the men in the no-rehabilitation group 2.
Prostaglandin E1 (PGE1)
Alprostadil is a vasodilatory prostaglandin E1 that can be injected into the penis or placement in the urethra in order to treat ED. Montorsi, et al. studied the use of intracorporeal injections of alprostadil starting at 1 month after bilateral nerve-sparing radical prostatectomy and reported a higher rate of spontaneous erections after 6 months compared with no treatment 3. Gontero, et al. investigated alprostadil injections at various time points after non–nerve-sparing radical prostatectomy and found that 70% of patients receiving injections within the first 3 months were able to achieve erections sufficient for intercourse, compared with 40% of patients receiving injections after the first 3 months 4.
Vacuum constriction device (VCD)
VCD is an external pump that is used to get and maintain an erection. Raina, et al evaluated the daily use of a VCD beginning within two months after radical prostatectomy, and reported that after 9 months of treatment, 17% of patients using the device had return of natural erections sufficient for intercourse, compared with 11% of patients in the nontreatment group 4.
PDE-5 Inhibitors
PDE-5 inhibitors (such as Sildenafil) are the first-line treatment for ED of many etiologies. Several studies have shown that the use of PDE-5 inhibitors might lead to an overall improvement in endothelial cell function in the corpus cavernosum. Chronic use of oral PDE-5 inhibitors suggest a beneficial effect on endothelial cell function. Desouza, et al. concluded that daily sildenafil improves overall vascular endothelial cell function. However, Zagaja, et al. found that men taking oral sildenafil within the first 9 months of a nerve-sparing procedure did not have any erectogenic response 4.
Overall, accumulating scientific literature is suggesting that penile rehabilitation therapies have a positive impact on the sexual function outcome in post-prostatectomy patients. It must be noted that these methods do not cure ED and should be used with caution.
1Penson DF, McLerran D, Feng Z, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005;173:1701-1705.
2Mulhall J, Land S, Parker M, et al. The use of an erectogenic pharmacotherapy regimen following radical prostatectomy improves recovery of spontaneous erectile function. J Sex Med. 2005; 2:532-540.
3Montorsi F, Guazzoni G, Strambi LF, et al. Recovery of spontaneous erectile function after nerve-sparing radical retropubic prostatectomy with and without early intracavernous injections of alprostadil: results of a prospective, randomised trial. J Urol. 1997;158:1408-1410.
4Gontero P, Fontana F, Bagnasacco A, et al. Is there an optimal time for intracavernous prostaglandin E1 rehabilitation following non- nerve sparing radical prostatectomy? Results from a hemodynamic prospective study. J Urol. 2003;169:2166-2169.
Earlier diagnosis is clearly a huge need for patients with pelvic floor dysfunction. Many patients suffer with their symptoms for years before even hearing the words “pelvic floor,” or realizing that a pelvic floor physical therapist may be able to help. For interstitial cystitis, one large survey article found fewer than 10% of patients with the condition had been correctly diagnosed with IC, even after years of symptoms and visits with multiple doctors.
Even after being diagnosed, patients still don’t learn about how the pelvic floor can be causing or exacerbating their symptoms. In one study of our interstitial cystitis patients, 46% learned about the importance of the pelvic floor on their own and sought out treatment independently, while nearly half felt they were referred by their physician to physical therapy far too late, as a ‘last resort.’ This is despite the fact that many of these patients had seen five or more physicians and physical therapy is considered the most proven treatment for IC by the American Urological Association.
Physicians, orthopedic physical therapists, other practitioners, and patients themselves need a simple, proven way to identify pelvic floor dysfunction to help patients find pelvic floor physical therapy earlier in their medical journey.
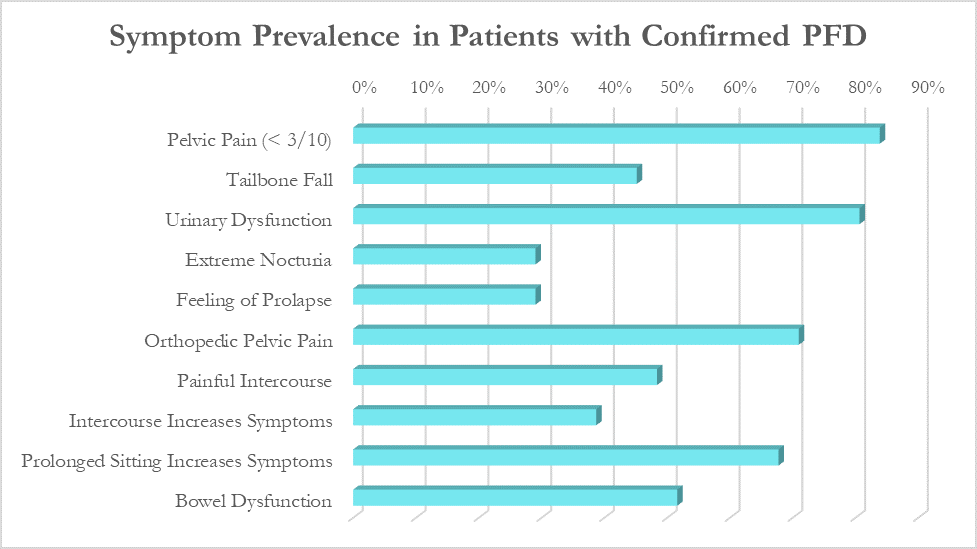
In a large survey of our patients with confirmed pelvic floor dysfunction, we examined what symptoms and medical history was most closely correlated with pelvic floor dysfunction. Any screening questionnaire would ideally be able to identify a wide variety of pelvic floor dysfunction, including patients with chronic pelvic pain, pelvic organ prolapse, orthopedic pain with a pelvic floor component (low back, hip, groin), urinary urgency/frequency, and/or bowel dysfunction.
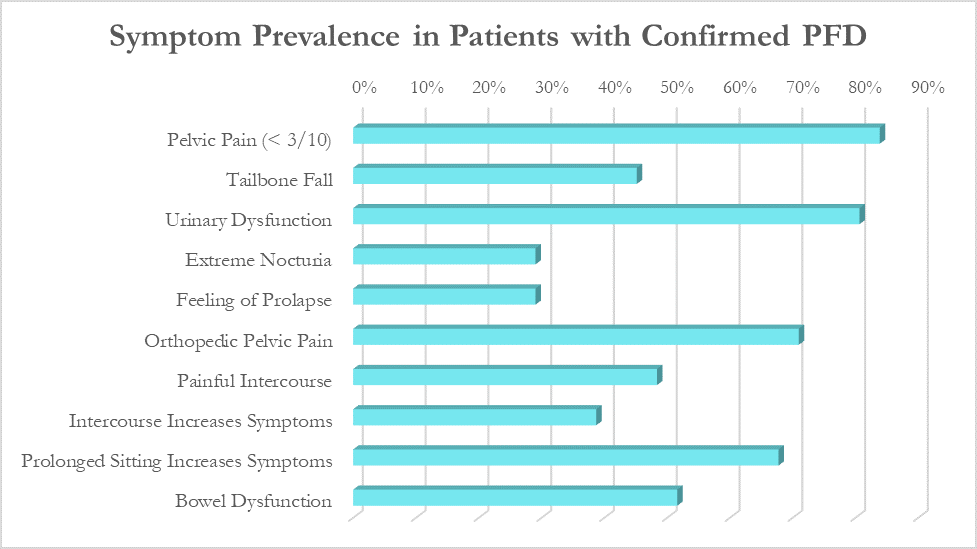
While these patients all had different medical diagnoses, many symptoms were common across the patient population. The most common were pelvic pain (84%), urinary urgency, frequency, or incontinence (81%), orthopedic pelvic pain (71%) and symptoms that worsen with prolonged sitting (68%).
Based on the survey results, we created the Cozean Pelvic Dysfunction Screening Protocol to screen for pelvic floor dysfunction and published the results in the International Pelvic Pain Society (2017). The goal was to correctly identify more than 80% of the patients with pelvic floor dysfunction (sensitivity). For ease of use by both practitioners and patients, the questions were phrased so they could be answered with a simple ‘yes/no’ (as a check box). If patients answers ‘yes’ to 3 or more of the questions, pelvic floor dysfunction is highly likely.
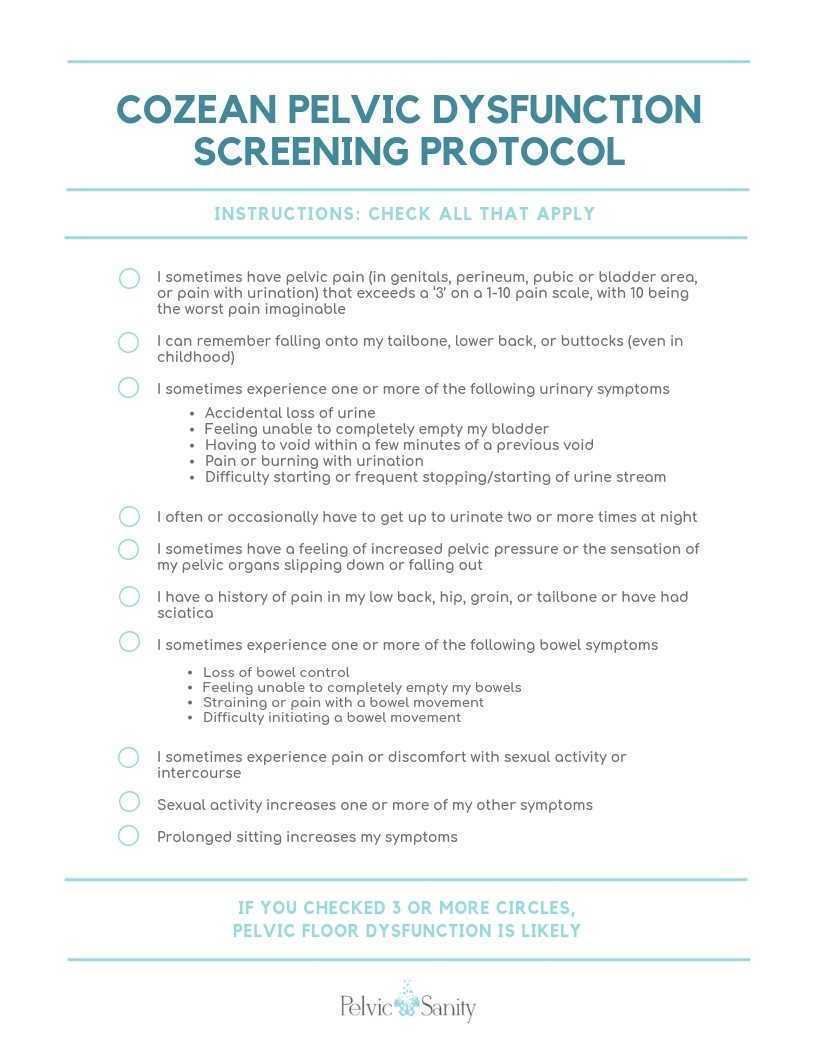 Document available for download at https://docs.wixstatic.com/ugd/d1026c_42a0fda8e5644930950d754619586614.pdf
Document available for download at https://docs.wixstatic.com/ugd/d1026c_42a0fda8e5644930950d754619586614.pdf
Testing the Model
In a model like this, we would expect a normal (bell-shaped) distribution curve of answers from patients with pelvic floor dysfunction. Some patients will score on the high end, others on the low, and the majority would be clustered in the middle. This is what we observe with use of the questionnaire, as seen by the trendline in the blow graph. Most patients with confirmed pelvic floor dysfunction cluster in scores between 3 and 7, with a few scoring at 8 or higher. Less than one out of ten patients with pelvic floor dysfunction score below a 2 on the questionnaire and would not be captured by this measure.
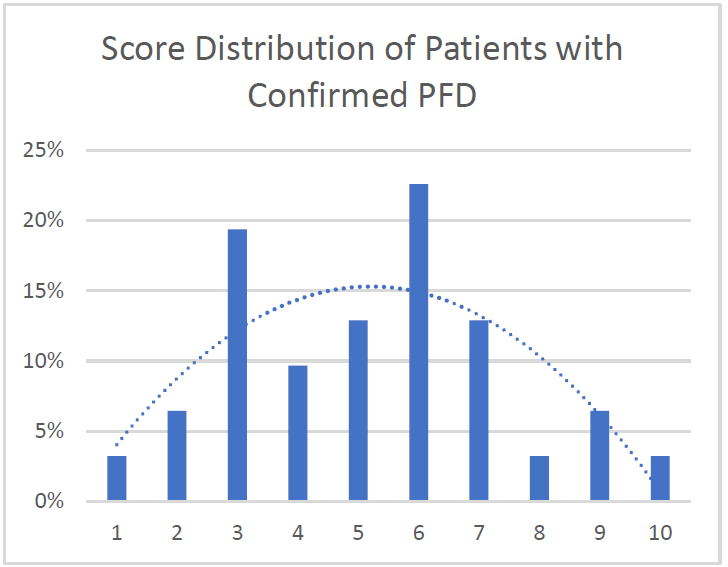
Specificity: 91%. More than 90% of patients with confirmed pelvic floor dysfunction were correctly identified by this screening protocol. Additional testing is required on a general population without PFD to determine the specificity of the questionnaire.
Average: 5.2. Of patients with confirmed PFD, the average score according to this screening protocol was 5.2 with a median score of 5 and a mode of 6. This is in line with what would be expected with a normal distribution curve.
We hope this 10-question survey is able to help patients with pelvic floor dysfunction be diagnosed earlier - whether by their physician, other physical therapists, or themselves – and seek pelvic floor physical therapy earlier in their medical journey. Please feel free to use the printable version of this protocol with your patients or in working with local practitioners.
Nicole Cozean will be teaching the course Interstitial Cystitis: Holistic Evaluation and Treatment in Princeton, NJ from April 6-7, 2019.
 Nicole Cozean is the founder of PelvicSanity physical therapy, in Orange County, California. Nicole was named the 2017 PT of the Year, is the first physical therapist to serve on the ICA Board of Directors, and is the award-winning and best-selling book The Interstitial Cystitis Solution (2016). She is an adjunct professor at her alma mater, Chapman University and teaches continuing education courses through the prestigious Herman & Wallace Institute.
Nicole Cozean is the founder of PelvicSanity physical therapy, in Orange County, California. Nicole was named the 2017 PT of the Year, is the first physical therapist to serve on the ICA Board of Directors, and is the award-winning and best-selling book The Interstitial Cystitis Solution (2016). She is an adjunct professor at her alma mater, Chapman University and teaches continuing education courses through the prestigious Herman & Wallace Institute.
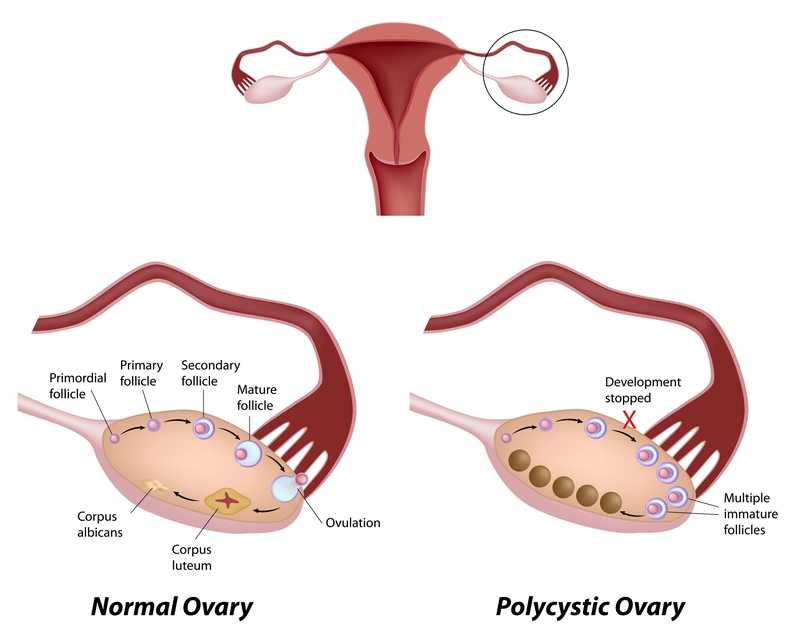
Few patients discuss polycystic ovary syndrome (PCOS) in orthopedic manual therapy, but one lady left a lasting impression. She was adopted and did not know her family’s medical history or her genetics. At 18, she had a baby as a result of rape. At 34, she was married and diagnosed with POCS. She struggled with infertility, anxiety, obesity, and hypertension. Although I saw her for cervicalgia, the exercise aspect of her therapy had potential to impact her overall well-being and possibly improve her PCOS symptoms.
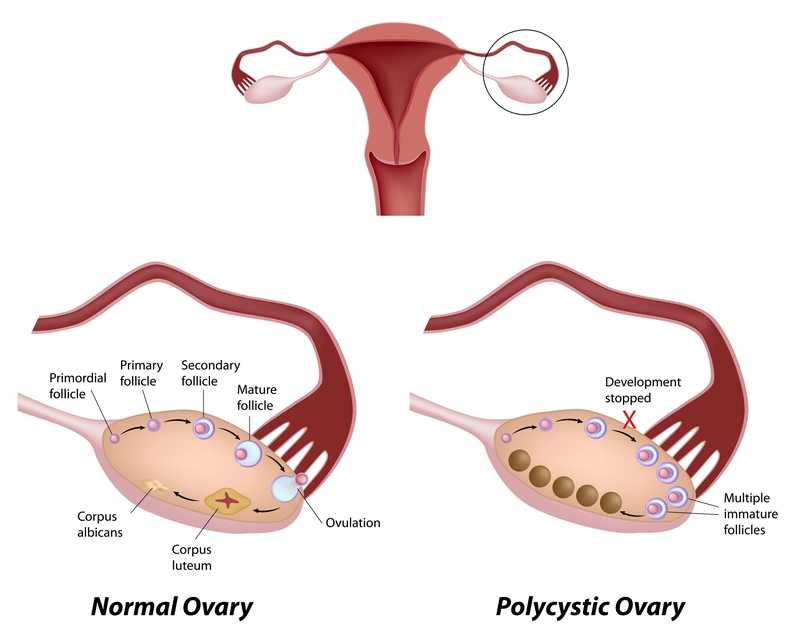 Pericleous & Stephanides (2018) reviewed 10 studies that considered the effects of resistance training on PCOS symptoms. Some of these symptoms include the absence of or a significant decrease in ovulation and menstruation, which can lead to infertility; obesity, which in turn can affect cardiovascular health and increase the risk of diabetes, insulin resistance, and metabolic syndrome; and, mental health problems. Research has shown resistance training benefits include lowering body fat, improving insulin resistance and glucose metabolism, and increasing insulin sensitivity in type II diabetes. Although it has been documented that obesity and insulin resistance can exacerbate PCOS symptoms, resistance training is not a common recommendation in healthcare settings for patients with PCOS . Studies have shown diet and exercise are essential to improve cardiac and respiratory health and body makeup in patients with PCOS, as the combination improves the Follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), ovulation, testosterone levels, and weight loss. One systematic review found that weight loss can improve PCOS symptoms without consideration of diet; however, most other studies find intake of various macronutrients (protein, fat, carbohydrates) may lead to different results, and the effects of resistance training can only be optimized with appropriate dietary changes. These authors concluded caloric consumption and macronutrient habits must be considered in conjunction with resistance training to determine the greatest impact on improving PCOS symptoms.
Pericleous & Stephanides (2018) reviewed 10 studies that considered the effects of resistance training on PCOS symptoms. Some of these symptoms include the absence of or a significant decrease in ovulation and menstruation, which can lead to infertility; obesity, which in turn can affect cardiovascular health and increase the risk of diabetes, insulin resistance, and metabolic syndrome; and, mental health problems. Research has shown resistance training benefits include lowering body fat, improving insulin resistance and glucose metabolism, and increasing insulin sensitivity in type II diabetes. Although it has been documented that obesity and insulin resistance can exacerbate PCOS symptoms, resistance training is not a common recommendation in healthcare settings for patients with PCOS . Studies have shown diet and exercise are essential to improve cardiac and respiratory health and body makeup in patients with PCOS, as the combination improves the Follicle-stimulating hormone (FSH), sex hormone-binding globulin (SHBG), ovulation, testosterone levels, and weight loss. One systematic review found that weight loss can improve PCOS symptoms without consideration of diet; however, most other studies find intake of various macronutrients (protein, fat, carbohydrates) may lead to different results, and the effects of resistance training can only be optimized with appropriate dietary changes. These authors concluded caloric consumption and macronutrient habits must be considered in conjunction with resistance training to determine the greatest impact on improving PCOS symptoms.
Benham et al., (2018) also performed a recent systematic review to assess the role exercise can have on PCOS. Fourteen trials involving 617 females of reproductive age with PCOS evaluated the effect of exercise training on reproductive outcomes. The data published did not allow the authors to quantitatively assess the impact of exercise of reproductive in PCOS patients; however, their semi-quantitative analysis allowed them to propose exercise may improve regularity of menstruation, the rate of ovulation, and pregnancy rates in these women. Via meta-analysis, secondary outcomes of body measurement and metabolic parameters significantly improved after women with PCOS underwent exercise training; however, symptoms such as acne and hirsutism (excessive, abnormal body hair growth) were not changed with exercise. The authors concluded exercise does improve the metabolic health (ie, insulin resistance) in women with PCOS, but evidence is insufficient to measure the exact impact on the function of the reproductive system.
Increasing our knowledge about comorbidities such as PCOS, regardless of our practice setting, can help us provide better education to the patients we treat. Perhaps exercise compliance can increase when patients are told multiple long-term benefits, not just immediate symptom relief. More often than not, a patient’s 4-6 week interaction with us could motivate and promote healthy lifestyle changes.
Pericleous, P., & Stephanides, S. (2018). Can resistance training improve the symptoms of polycystic ovary syndrome? BMJ Open Sport — Exercise Medicine, 4(1), e000372. http://doi.org/10.1136/bmjsem-2018-000372
Benham, J. L., Yamamoto, J. M., Friedenreich, C. M., Rabi, D. M. and Sigal, R. J. (2018), Role of exercise training in polycystic ovary syndrome: a systematic review and meta‐analysis. Clin Obes, 8: 275-284. doi:10.1111/cob.12258
Suggested newly published resource for readers…
Teede, H. J., Misso, M. L., Costello, M. F., Dokras, A., Laven, J., Moran, L., … Yildiz, B. O. (2018). Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Human Reproduction (Oxford, England), 33(9), 1602–1618. http://doi.org/10.1093/humrep/dey256
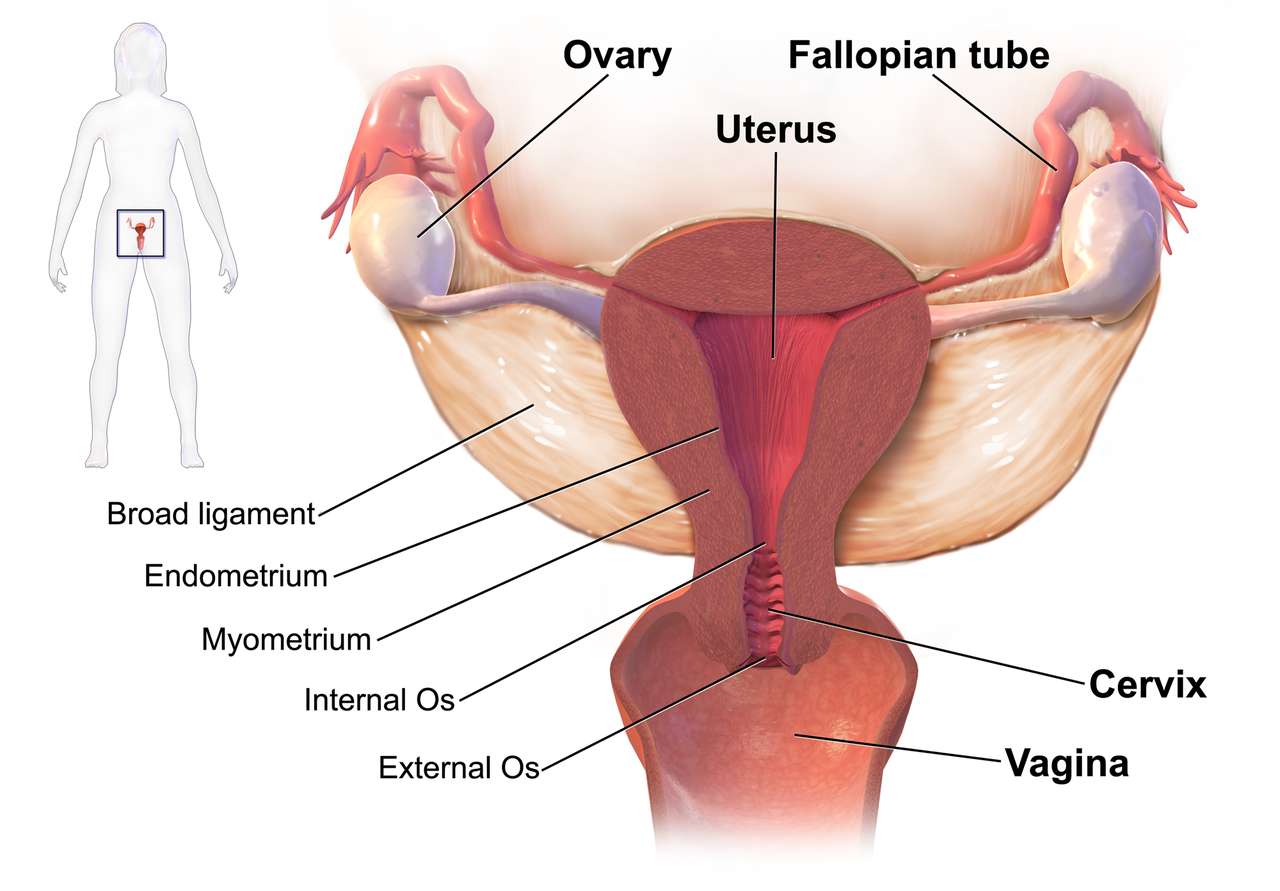
September is Gynae Cancer Awareness Month – but how aware are we as clinicians of the signs and symptoms, the epidemiology and the sequalae of treatment afterwards? As pelvic rehab specialists, we have the privilege of helping women live well after cancer treatment ends, both on a ‘local’ pelvic area (bladder, bowel, sexual and pelvic pain management strategies) but also on a more ‘global’ level – dealing with issues such as cancer related fatigue, bone health and cardiovascular concerns.
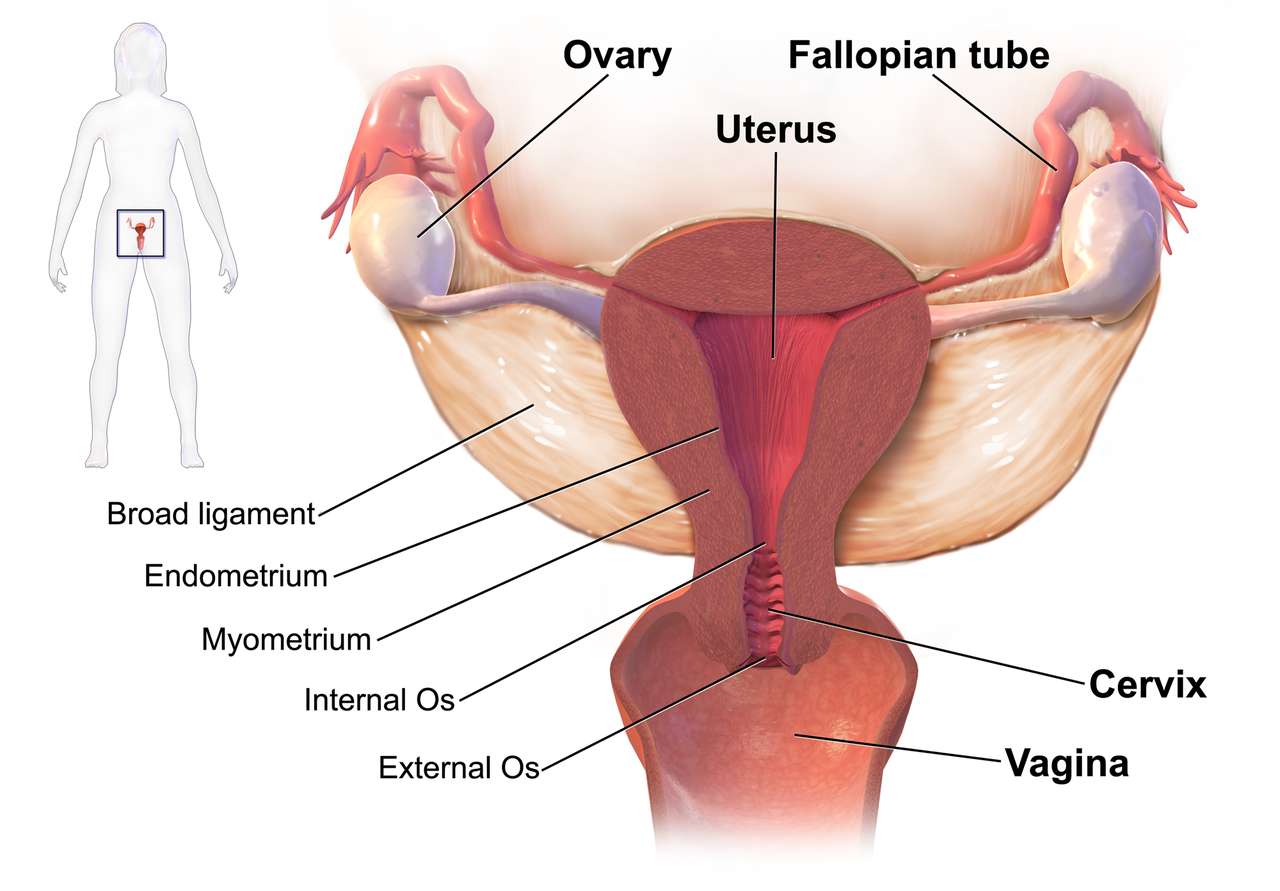 We know that women who are diagnosed with cancer of the vulva, vagina, cervix, endometrium or ovaries are treated with a combination of surgery, radiation or chemotherapy. However, with improving treatment and better survival rates, there is evidence that a variety of pelvic health concerns may arise for these women, both during and after treatment. (Hazewinkel et al 2010). For example, urinary incontinence is reported in 80% of women treated for endometrial cancer, with more severe symptoms and impact on quality of life in those who had adjuvant radiation (Erekson et al 2009) In Malone’s 2017 paper, ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’, the author notes that ‘…there is currently a lack of knowledge regarding the effects of PFD on QoL in this cohort. Patients do not always report these problems to their health care providers and clinicians may underestimate symptoms…In the context of having survived cancer, PFD may be seen as relatively trivial. However, in the context of resuming normal living, the symptoms experienced by the survivors may be significant’.
We know that women who are diagnosed with cancer of the vulva, vagina, cervix, endometrium or ovaries are treated with a combination of surgery, radiation or chemotherapy. However, with improving treatment and better survival rates, there is evidence that a variety of pelvic health concerns may arise for these women, both during and after treatment. (Hazewinkel et al 2010). For example, urinary incontinence is reported in 80% of women treated for endometrial cancer, with more severe symptoms and impact on quality of life in those who had adjuvant radiation (Erekson et al 2009) In Malone’s 2017 paper, ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’, the author notes that ‘…there is currently a lack of knowledge regarding the effects of PFD on QoL in this cohort. Patients do not always report these problems to their health care providers and clinicians may underestimate symptoms…In the context of having survived cancer, PFD may be seen as relatively trivial. However, in the context of resuming normal living, the symptoms experienced by the survivors may be significant’.
This can present a clinical conundrum – often pelvic rehab therapists are nervous when working with a patient who has a current or previous gynecologic cancer diagnosis, but similarly oncology rehab specialists may have qualms about dealing with pelvic health issues, with the result that these women fall through the cracks and do not have their pelvic health issues managed properly (or at all). Theodore Roosevelt once said ‘No one cares how much you know, until they know how much you care’ and this is especially relevant for oncology pelvic rehab. Often you may be the first clinician to ask about bladder, bowel or sexual function or dysfunction. An understanding of the effects of cancer treatments on the pelvis is important but so too is the wealth of information you may already have about bladder, bowel and sexual health as well as neuroscience and pain education.
The most important thing is to ask these women about their pelvic health concerns – the National Coalition for Cancer Survivorship defined cancer survivorship as extending from ‘the time of diagnosis and for the balance of life’. An emphasis on quality of life has been emphasised – if we know that cancer survivors may not independently volunteer information about their pelvic floor dysfunction, it is our responsibility to ask the questions and comprehensively treat and advocate for these women, in order to help them live well after cancer treatment ends.
- Hazewinkel MH. Sprangers MA, Velden Jvd, Vaart CH, Stalpers LJ, Burger MP ‘Longterm cervical cancer survivors suffer from pelvic floor dysfunction symptoms: A cross-sectional matched cohort study’ Gynecol Oncol 2010;117(2):381-6
- Erekson EA, Sung VW, Disilvestro PA, Myers DL ‘Urinary symptoms and impact on quality of life in women after treatment for endometrial cancer’ Int Urogynecol J 2009;20(2):159-63
- Malone P, Danaher D, Galvin R, Cusack T ‘The patient’s voice: What are the views of women on living with pelvic floor problems following successful treatment for pelvic cancers?’ Physiotherapy Practice and Research 38(2017)93-102
The following is part two in a series documenting Deb Gulbrandson, PT, DPT's journey treating a 72 year old patient who has been living with multiple sclerosis (MS) since age 18. Catch up with Part one of the patient case study on the Pelvic Rehab Report here. Dr. Gulbrandson is a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method, and she helps teach The Meeks Method for Osteoporosis course.
On Maryanne’s second visit, she reported she had been doing her “homework” and didn’t have any questions. Just to be sure, we reviewed them and I had her demonstrate. In Decompression position, she was lying supine with her hands on her abdomen, a common mistake I see. Usually this is due to tightness in pec minor with protracted scapulae. Patients unknowingly resort to the path of least resistance to take the strain off of the muscles. I explained to her that we want to use gravity to gently lengthen those muscles and “widen” the collarbones to allow for improved alignment. With her shoulders abducted to approximately 30 degrees and palms up, I propped a couple of small towels under her forearms which allowed her shoulders to relax into a more posterior and correct position.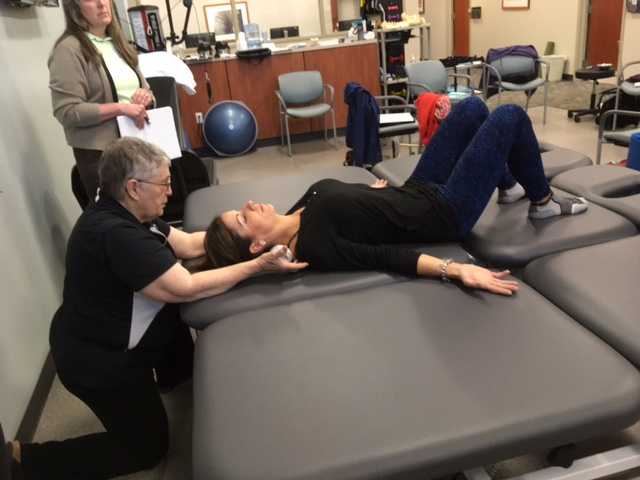
“Today we begin the Re-alignment routine,” I said, “starting with the Shoulder Press.” I showed her how to gently press the back of her shoulders down into the mat without arching her lumbar spine. “As you press your shoulders down, exhale through your mouth as if you’re fogging a mirror. This will help activate your core muscles to keep your back in good alignment. Hold for 2-3 seconds, and then relax. Repeat 3 times.” Maryanne looked at me as if I’d lost my mind. “Did you say do 3 reps?” she asked. “I do 2 sets of 20 reps at the gym,” she said with obvious pride in her voice. “Yes, that’s where we start, and there are a couple of reasons. First, these are very site specific exercises which focus on the exact areas that need strengthening. Exercises done in a gym setting are often more general and usually involve compensation. We are minimizing any compensation such as allowing your low back to arch. There is probably weakness in those upper back muscles as well as the tightness seen in your anterior chest muscles and we need to go slowly. Also, we are simultaneously stretching while we strengthen. Our society is so forward biased (we work on computers, drive cars, make beds, eat- it’s all forward, forward, forward), that the anterior muscles get tight and the upper back muscles get overstretched and weak. We need to reverse that pattern. Take a look at our younger population and their texting postures. Yikes! We will be layering on more exercises as your technique improves so you’ll be doing more than just 3 reps, I promise.”
After the Shoulder Press we proceeded with the Head Press, Leg Lengthener and Arm Lengthener, spending time to make sure her cervical spine stayed in neutral as she pressed her head down into the mat. Head Press (cervical retraction) performed in supine allow patients to have something to press against and helps inhibit the tendency to move into cervical extension. It can also be done standing against the wall with a small pillow or folded towels between the occiput and the wall.
We ended with Maryanne in standing at the kitchen sink to promote functional activities and weight bearing positions. I reminded her to do the Foot Press through the floor using the Triangle of Foot Support visual. This helped to elongate her spine. “Imagine a bungie cord running from the top back of your head to the ceiling” I said which further increased her standing height. “Now I want you to imagine a shelf running straight out from your breastbone with a glass of some very expensive fine drink sitting on it. Do not spill your libation! Oh, and one last thing Maryanne. Breathe!!!” At which point she collapsed into laughter and our session was over. “Busted”, she said.
As so many of our patients are shallow breathers, I found this research on the effects of mindful attention to the breath (MATB) on prefrontal cortical and amygdala activity especially informative and relevant to patient care. Twenty-six healthy volunteers with no prior meditation experience were introduced to MATB by an experienced meditation teacher and instructed to practice a 20-minute audio guided MATB meditation daily for 2 weeks.1 At the end of the 2-week training period, subjects underwent fMRI scanning while viewing distressing emotional images with MATB and with passive viewing (PV). Participants were shown aversive pictures or no pictures and were instructed to “Please focus your attention on your breath as you were instructed in the training” or “Please watch the picture without changing anything about your feelings.” Subjects indicated their current affect on a 7 point scale ranging from -3 (very negative) to +3 (very positive).
Breathing frequency significantly decreased during MATB compared to PV. Researchers controlled for this by including breathing frequency as a covariate in further behavioral and brain data analysis.
Analysis of affective ratings showed that participants felt significantly less negative affect when viewing distressing visual stimuli during MATB than PV. During negative visual stimuli, MATB significantly decreased bilateral amygdala activation compared to PV. Also, right amygdala activation decrease specifically correlated with successful emotional regulation. That is, those participants with greater reductions in right amygdala activation reported greater reductions in aversive emotions during the MATB. In addition, emotion-related functional connectivity increased between the prefrontal cortex and amygdala during the viewing of negative images and MATB.
It’s exciting to have some initial science behind the benefits of MATB. I teach all of my patients MATB and have found it rewarding to get feedback from participants in my courses about their integration of MATB into their own patient care. Patients with complex pain conditions can be challenging to treat, however sometimes a simple practice of taking 2 to 3 minutes prior to and/or at the end of a treatment to have a patient calmly focus on their breath with the mindful attitudes of acceptance, kindness and curiosity can help a person shift from tension and distress to calm and confidence. I look forward to presenting this and additional research on the impact of mindful meditation on brain structure and function in my upcoming course, Mindfulness-Based Pain Treatment, in Seattle, November 4 and 5. Hope to see you there!
1. Doll A, Holzel BK, Bratec SM, et al. Mindful attention to breath regulates emotions via increased amygdala-prefrontal cortex connectivity. Neuroimage. 2016;134:305-313.
 In July of this year, I was invited to present in Christchurch, New Zealand as part of a teaching tour that took in Singapore, Australia and Tasmania. The topic of my class was female pelvic pain, so we discussed Endometriosis, Vulvodynia, Sexual Health and many other sub-topics but we had several discussions about the effects of trauma on pelvic pain. For those who have visited Christchurch, it is a beautiful city but it is still reeling from a series of massive earthquakes, that started in September 2010. The most devastating was in February 2011, when 185 people were killed and 6600 people were injured. Everywhere you go in Christchurch, there are reminders – from the constant buzz of ongoing construction, to structures that are waiting demolition, like the beautiful old cathedral that was beside our hotel. Usually, when I teach, we do some ‘housekeeping’ announcements about fire drills and exits; in Christchurch it was ‘In the event of an earthquake…’. I wondered how the near constant reminders were affecting the inhabitants, so I read of how ‘…people called living with continual shaking, damaged infrastructure, insurance battles and unrelenting psychological stress ‘the new normal’. There are several ongoing research studies, looking at the effects of this trauma and how it is still having an effect on the people of Christchurch.
In July of this year, I was invited to present in Christchurch, New Zealand as part of a teaching tour that took in Singapore, Australia and Tasmania. The topic of my class was female pelvic pain, so we discussed Endometriosis, Vulvodynia, Sexual Health and many other sub-topics but we had several discussions about the effects of trauma on pelvic pain. For those who have visited Christchurch, it is a beautiful city but it is still reeling from a series of massive earthquakes, that started in September 2010. The most devastating was in February 2011, when 185 people were killed and 6600 people were injured. Everywhere you go in Christchurch, there are reminders – from the constant buzz of ongoing construction, to structures that are waiting demolition, like the beautiful old cathedral that was beside our hotel. Usually, when I teach, we do some ‘housekeeping’ announcements about fire drills and exits; in Christchurch it was ‘In the event of an earthquake…’. I wondered how the near constant reminders were affecting the inhabitants, so I read of how ‘…people called living with continual shaking, damaged infrastructure, insurance battles and unrelenting psychological stress ‘the new normal’. There are several ongoing research studies, looking at the effects of this trauma and how it is still having an effect on the people of Christchurch.
If you’ve attended Pelvic Floor Level 1 with Herman & Wallace, you’ll remember we quote a study from Van der Welde about the effects of perceived danger on muscle activity in the upper trapezius and pelvic floor muscles. We also discuss the work of Levine, of ‘Waking the Tiger’ fame, who explores the somatic effects of trauma in our bodies – and how trauma, much like pain, is whatever we say it is.
I became intrigued with the topic, so I was delighted to hear that Lauren Mansell has created a course to deal exactly with this topic. I was even more delighted when she sat down for a chat with me to explore the nuances of trauma awareness, boundary setting and self-care for therapists, especially pelvic therapists, who work with those who have experienced trauma of any kind.
I hope you find this conversation as interesting as I did! Here is our conversation:
1. ‘Vaginismus, a Component of a General Defensive Reaction. An Investigation of Pelvic Floor Muscle Activity during Exposure to Emotion-Inducing Film Excerpts in Women with and without Vaginismus’ van der Velde, J & Laan, Ellen & Everaerd, W. (2001)
2. ‘Waking The Tiger’ by Peter A. Levine (1997)
The following case study comes from faculty member Deb Gulbrandson, PT, DPT, a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method. Join Dr. Gulbrandson in The Meeks Method for Osteoporosis on September 22-23, 2018 in Detroit, MI!
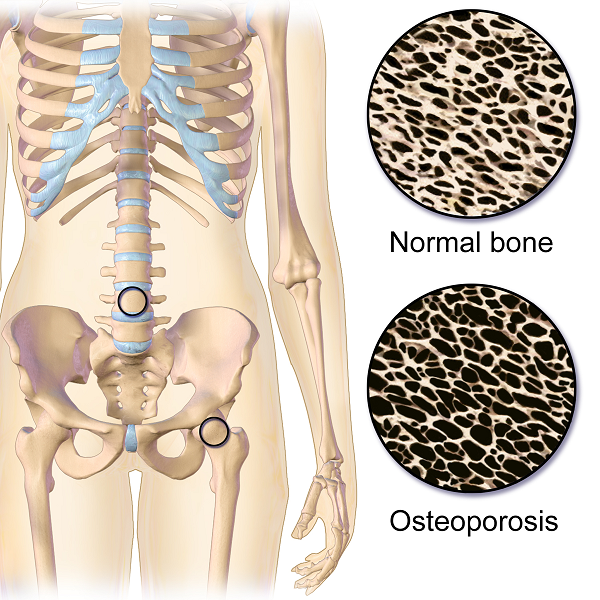
The first sight I had of my new patient was watching her being wheeled across the parking lot by her husband. A petite 72-year-old, I could see her slouched posture in the wheelchair. With the double diagnosis of osteoporosis and Multiple Sclerosis (MS) it didn’t look good. However, “Maryanne“ greeted me with a wide grin and a friendly, “I’m so excited to be here. I’ve heard good things about this program and can’t wait to get started.“
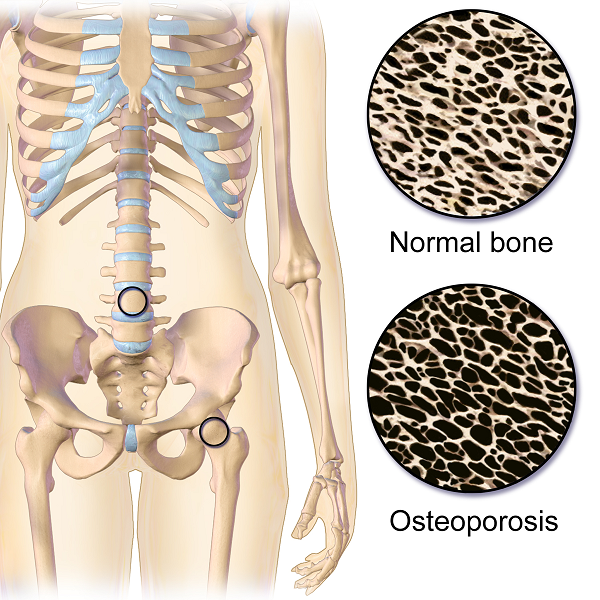 That’s what I find with my osteoporosis patients. They are highly motivated and willing to do the work to decrease their risk of a fracture. Maryanne was unusual in that she was diagnosed with MS at a very young age. She was 18 and had lived with the disease in a positive manner. She exercised 3X a week and had a caring, involved husband. They worked out at a local health club, taking advantage of the Silver Sneakers program. Maryanne was able to stand holding onto the kitchen counter but had stopped walking five years ago due to numerous falls. She performed standing transfers with her husband providing moderate to max assist. Her osteoporosis certainly put her at a high risk for fracture.
That’s what I find with my osteoporosis patients. They are highly motivated and willing to do the work to decrease their risk of a fracture. Maryanne was unusual in that she was diagnosed with MS at a very young age. She was 18 and had lived with the disease in a positive manner. She exercised 3X a week and had a caring, involved husband. They worked out at a local health club, taking advantage of the Silver Sneakers program. Maryanne was able to stand holding onto the kitchen counter but had stopped walking five years ago due to numerous falls. She performed standing transfers with her husband providing moderate to max assist. Her osteoporosis certainly put her at a high risk for fracture.
Even though she had been exercising on a regular basis, she was unfortunately doing many of the wrong exercises. Her workout consisted of sit-ups and crunches. She used the Pec Deck bringing her into scapular protraction and facilitating forward flexion. She was also stretching her hamstrings by long sitting reaching to touch her toes.
Spinal flexion is contraindicated in patients with osteoporosis. A landmark study done in 19841 divided a group of women with osteoporosis into 4 groups. One group performed extension based exercises, a second group did flexion. A third group used a combination of flexion and extension and the fourth was the control and did no exercises. Below are the results 1-6 years later.
- Extension Group: 16% incidence of fracture or wedging of vertebral bodies
- Flexion Group: 89% rate.
- Combination Extension/Flexion: 53% rate
- No Exercise Group: 67%
The results were astounding. Granted, it was a small study- 59 participants and it was done a long time ago. But this is a one study that no one wants to repeat, or volunteer for!
Several take home messages followed this study.
- Flexion is contra-indicated for individuals with osteoporosis.
- It’s better to do no exercise than the wrong exercise. The No Exercise group faired better than the Flexion group although at 67% it’s clear that many of our everyday activities- making beds, placing items on low shelves, and now computing and texting put us at risk.
Sadly, many individuals with osteoporosis are told by their physicians to start exercising.......but without any guidance they do what Maryanne did. Just start exercising. And putting themselves at greater risk.
Maryanne was also doing nothing to strengthen her back extensors and scapular area. After giving an overview of the vertebral bodies, pelvis, and hip joint with my trusty spine, I showed both my patient and her husband how forward flexion puts increased compression on the anterior aspect of the spine, particularly in the thoracic curve at T 7, 8, 9, the most common site of compression fractures. We started with Decompression, which is the beginning position for the Meeks method. Many therapists know this as hooklying. This position allows the spinous processes to press against the hard surface of the floor, opening up the anterior portion of the spine and providing tensile forces throughout the length of the spine. With the help of her husband, Maryanne could get down on the floor but I often advise patients who are unable to safely transfer to the floor to lay across the end of their bed. This is less cushy than lying longways where they sleep. Adding a yoga mat or a quilt on top to give more firmness improves the effect.
Supine is the least compressive of all positions; sitting is the most compressive. While Decompression may not seem like much of an exercise it is vital to reduce the effects of gravity and compression on the spine.
We addressed sitting posture by firming up the base of her wheelchair as well as recommending transferring into other chairs and positions frequently throughout the day. Spending time sitting towards the edge of a firm chair in what we call Perch Posture and practicing Foot Presses into the floor created improved alignment in her spine as well as isometrically activating glutes, abs, quads. Using the Foot Press is an example of Newtons 3rd Law, “For every action there’s an equal and opposite reaction” so by pressing her feet down she actually lengthened her torso and head. We also discussed discontinuing the contraindicated exercises in her workout routine and I assured her that the Meeks method would progressively challenge her core (the reason everyone thinks they should do sit-ups) and target the right muscles to help strengthen her bones. We use site specific exercises to target certain muscles that pull on the bone and increase bone strength.2
With instructions to Decompress several times daily to reduce compression on the spine along with the other adjustments made, I felt Maryanne was on her way to reducing her risk of fracture and increasing the quality of her life. She thanked me profusely for the education and the exercise of that session. We both look forward to the next one.
1. Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil. 1984 Oct;65(10):593-6.
2. Frost HM1. Wolff's Law and bone's structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994;64(3):175-88.
Managing a medical crisis such as a cancer diagnosis can be overwhelming for an individual. Faced with choices about medical options, dealing with disruptions in work, home and family life often leaves little energy left to consider sexual health and intimacy. Maintaining closeness, however, is often a goal within a partnership and can aid in sustaining a relationship through such a crisis. The research is clear about cancer treatment being disruptive to sexual health, yet intimacy is a larger concept that may be fostered even when sexual activity is impaired or interrupted. Last year, when I was asked to speak to the Pacific NW Prostate Cancer Conference about intimacy, I was pleasantly surprised to find a rich body of literature about maintaining intimacy despite a diagnosis of prostate cancer.
 Sexual health and sexuality is a social construct affected by many factors including mood, stress, depression, self-image, physiology, psychology, culture, relational and spiritual factors (Beck et al., 2009; Weiner & Avery-Clark, 2017) Prostate cancer treatment can change relational roles, finances, work life, independence, and other factors including hormone levels.(Beck et al., 2009) Exhaustion (on the part of the patient and the caregiver), role changes, changes in libido and performance anxiety can create further challenges. (Beck et al., 2009; Hawkins et al., 2009; Higano et al., 2012) Recovery of intimacy is possible, and reframing of sexual health may need to take place. Most importantly, these issues need to be talked about, as renegotiation of intimacy may need to take place after a diagnosis or treatment of prostate cancer. (Gilbert et al., 2010)
Sexual health and sexuality is a social construct affected by many factors including mood, stress, depression, self-image, physiology, psychology, culture, relational and spiritual factors (Beck et al., 2009; Weiner & Avery-Clark, 2017) Prostate cancer treatment can change relational roles, finances, work life, independence, and other factors including hormone levels.(Beck et al., 2009) Exhaustion (on the part of the patient and the caregiver), role changes, changes in libido and performance anxiety can create further challenges. (Beck et al., 2009; Hawkins et al., 2009; Higano et al., 2012) Recovery of intimacy is possible, and reframing of sexual health may need to take place. Most importantly, these issues need to be talked about, as renegotiation of intimacy may need to take place after a diagnosis or treatment of prostate cancer. (Gilbert et al., 2010)
If the patient brings up sexual health, or we encourage the conversation, there are many research-based suggestions we can provide to encourage recovery of intimacy, several are listed below.
- Manage general health, fitness, nutrition, sleep, anxiety and stress
- Redefine sex as being beyond penetration, consider other sexual practices such as massage/touch, cuddling, talking, use of vibrators, medication, aids such as pumps (Usher et al., 2013)
- Participate in couples therapy to understand partners’ needs, address loss, be educated about sexual function (Wittman et al., 2014; Wittman et al., 2015)
- Participate in “sensate focus” activities (developed by Masters & Johnson in 1970’s as “touch opportunities”) with appropriate guidance (Weiner & Avery-Clark 2017)
Within the context of this information, there is opportunity to refer the patient to a provider who specializes in sexual health and function. While some rehabilitation professionals are taking additional training to be able to provide a level of sexual health education and counseling, most pelvic health providers do not have the breadth and depth of training required to provide counseling techniques related to sexual health- we can, however, get the conversation started, which in the end may be most important.
In the men’s health course, we further discuss sexual anatomy and physiology, prostate issues, and look at the research describing models of intimacy and what worked for couples who did learn to renegotiate intimacy after prostate cancer.
Beck, A. M., Robinson, J. W., & Carlson, L. E. (2009, April). Sexual intimacy in heterosexual couples after prostate cancer treatment: What we know and what we still need to learn. In Urologic oncology: seminars and original investigations (Vol. 27, No. 2, pp. 137-143). Elsevier.
Beck, A. M., Robinson, J. W., & Carlson, L. E. (2013). Sexual Values as the Key to Maintaining Satisfying Sex After Prostate Cancer Treatment : The Physical Pleasure–Relational Intimacy Model of Sexual Motivation. Archives of sexual behavior, 42(8), 1637-1647.
Gilbert, E., Ussher, J. M., & Perz, J. (2010). Renegotiating sexuality and intimacy in the context of cancer: the experiences of carers. Archives of Sexual Behavior, 39(4), 998-1009.
Hawkins, Y., Ussher, J., Gilbert, E., Perz, J., Sandoval, M., & Sundquist, K. (2009). Changes in sexuality and intimacy after the diagnosis and treatment of cancer: the experience of partners in a sexual relationship with a person with cancer. Cancer nursing, 32(4), 271-280.
Higano, C. S. (2012). Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer. Journal of Clinical Oncology, 30(30), 3720-3725.
Ussher, J. M., Perz, J., Gilbert, E., Wong, W. T., & Hobbs, K. (2013). Renegotiating sex and intimacy after cancer: resisting the coital imperative. Cancer Nursing, 36(6), 454-462.
Weiner, L., Avery-Clark, C. (2017). Sensate Focus in Sex Therapy: The Illustrated Manual. Routledge, New York.
Wittmann, D., Carolan, M., Given, B., Skolarus, T. A., An, L., Palapattu, G., & Montie, J. E. (2014). Exploring the role of the partner in couples’ sexual recovery after surgery for prostate cancer. Supportive Care in Cancer, 22(9), 2509-2515.
Wittmann, D., Carolan, M., Given, B., Skolarus, T. A., Crossley, H., An, L., ... & Montie, J. E. (2015). What couples say about their recovery of sexual intimacy after prostatectomy: toward the development of a conceptual model of couples' sexual recovery after surgery for prostate cancer. The journal of sexual medicine, 12(2), 494-504.
 Several weeks ago, I evaluated a patient who was referred to me from a fellow physical therapist. The patient was suffering from sacroiliac joint and low back pain. The patient is a 34-year-old nulliparous woman who is physically fit and participates in several outdoor activities. The therapist had fully evaluated the patient and did not find any articular issues within her spine or pelvis. What she did find was weakness in her local stabilizing muscles and tightness in her global stabilizing muscles. The therapist has an ample amount of clinical experience at treating low back and pelvic pain issues. She is adept at using different verbal cues, positions, and tactile cueing in order to help encourage proper activation of the local core muscles. However, the therapist knew the patient was not getting her local core muscles to fire properly. She didn’t know what else to do with this patient in order to get her to properly activate these muscles. She had tried numerous positions, verbal and tactile cueing without success.
Several weeks ago, I evaluated a patient who was referred to me from a fellow physical therapist. The patient was suffering from sacroiliac joint and low back pain. The patient is a 34-year-old nulliparous woman who is physically fit and participates in several outdoor activities. The therapist had fully evaluated the patient and did not find any articular issues within her spine or pelvis. What she did find was weakness in her local stabilizing muscles and tightness in her global stabilizing muscles. The therapist has an ample amount of clinical experience at treating low back and pelvic pain issues. She is adept at using different verbal cues, positions, and tactile cueing in order to help encourage proper activation of the local core muscles. However, the therapist knew the patient was not getting her local core muscles to fire properly. She didn’t know what else to do with this patient in order to get her to properly activate these muscles. She had tried numerous positions, verbal and tactile cueing without success.
Do you ever have patients where you feel stuck, who are not progressing as you would like them to in treatment? We all do! It is frustrating, isn’t it? The physical therapist called me and asked me to evaluate the patient using real-time ultrasound imaging. The therapist said “If the patient can just see what she is doing, she will then be able to learn how to work the muscles correctly.” She referred the patient to me so I could use ultrasound imaging within the treatment to better assess her activation strategies and use the imaging for biofeedback for with the patient. The patient was amazed with the ability to see what the different layers of muscles were doing. We found she was contracting her TA but only on her left side, and her deep multifidus was not firing at all. Using the ultrasound images, the patient was able to learn the proper way to activate her muscles. She is now working on a strengthening program for her local core muscles including her TA, pelvic floor, and multifidus. Within two treatments, the patient was able to fire her muscles in a different way and reports her back has felt better than it has in years!

The Pathway Ultrasound Imaging System, available from The Prometheus Group, is a portable ultrasound solution for pelvic rehab
I cannot emphasize enough how using ultrasound might change your practice! It not only can help you when you are stuck with a patient’s progress, but it can attract more patients to your practice. There are a lot of visual learners out there and access to visual images in therapy can influence progress and the results that are achieved. You not only can use the ultrasound to retrain the local core muscles for back and pelvic instability patients, but you can use it for incontinence patients, prolapse patients, and post prostatectomy patients as well. You can strengthen the pelvic floor without having to disrobe the patient each visit. How many men and women would appreciate that?
If you are interested in learning more about how you can use ultrasound in your practice, join me in August in New Jersey, or in November in California for Rehabilitative Ultrasound Imaging - Women's Health and Orthopedic Topics! See you there!