Angie Mueller PT, DPT is the instructor of Low Pressure Fitness and Abdominal Massage for Pelvic Floor Care, a new course on the hypopressive technique and abdominal massage for pelvic health. Join Dr. Mueller on July 27-29 in Princeton, NJ to learn more!
One of the first things I do as a pelvic PT when helping a woman recover from pelvic or core dysfunction, is center her uterus. I believe the uterus is the center of a women- biomechanically, physiologically, and energetically. I have seen that when the uterus is out of position, everything else in the pelvis and core is largely impacted and functions less efficiently. This includes muscular, gastrointentinal, liver, bowel and bladder, hormonal and sexual function.
 The uterus is supported by several important ligaments, which extend from the uterus out to the pelvic bones, as well as to the organs surrounding it- bladder, bowel and intestines. So if this magnificent central organ is out of her “center”- leaning forwards or backwards, or tipped to on side or the other- this can lead to a myofascial imbalance in the pelvis and cause symptoms of pelvic floor dysfunction, pain, and hormonal imbalances.
The uterus is supported by several important ligaments, which extend from the uterus out to the pelvic bones, as well as to the organs surrounding it- bladder, bowel and intestines. So if this magnificent central organ is out of her “center”- leaning forwards or backwards, or tipped to on side or the other- this can lead to a myofascial imbalance in the pelvis and cause symptoms of pelvic floor dysfunction, pain, and hormonal imbalances.
In treating thousands of women with pelvic dysfunction, I have observed that a uterus which is leaning too far forward (anteflexed) is often associated with urinary incontinence, issues with bladder urgency and frequency, and bladder prolapse (cystocele). A uterus that is tipped backwards is often associated with constipation, hemorrhoids and bowel prolapse (rectocele). A uterus that is leaning left or right is often associated with hip dysfunction, sacroiliac joint dysfunction and lumbo-pelvic alignment issues. This leads to and hip and/or knee and/or back pain due to asymmetrical pulling of the internal abdomino-pelvic fascia, especially the uterosacral and cardinal ligaments, which affects pelvic and sacral bone alignment, and then knee and ankle tracking. So centering the uterus will balance the internal pelvic and abdominal fascia, and can significantly improves cases of back pain, hip pain, knee or ankle pain.
Ensuring our organs are in their best position for receiving blood, lymph, nerve and hormonal support is critical to their health and function! If any organ in the body, especially the uterus, is not in its optimal position to receive blood, nerve, lymphatic and hormonal circulation, its function will be impacted. Therefore a mal-positioned uterus can also lead to problems with the menstrual cycle, painful periods, and fertility. When assisting any woman through a rehabilitative process, I have found it critical to appreciate how her uterine position contributes to and impacts her overall pelvic and core health- from a musculoskeletal, biomechanical and physiological perspective.
I have found that the best pelvic therapy outcomes result from use of both passive and active techniques to center the uterus. The first step is passive positioning of the uterus, which is most efficiently accomplished through abdominal massage. Abdominal self massage should be done daily. Abdominal massage will help to release any myofascial and ligamentous restrictions that are leading to a mal-positioned uterus. Abdominal massage also greatly improves blood flow and lymphatic circulation to the gut and pelvic organs leading to improved digestion and organ detoxification. Once her uterus is centered by the massage, it is important to immediately implement an active technique that will keep the uterus centered. This active uterine positioning technique must trigger the appropriate posture and breath that will keep her uterus centered with movement and throughout the activities of the day.
The second step to positioning her uterus is active activation of abdomino-pelvic musculature and key fascial chains that elevate and center the pelvic organs. This is accomplished through one of the latest core neuro-reeducation techniques- Low Pressure Fitness®. The Low Pressure Fitness methodology involves a seamless progression of postures and poses that cause a reduction in pressure in the abdomen and trigger an automatic response from the core muscles- abdominals, pelvic floor, multifidus, diaphragm. Low Pressure Fitness uses a breathing technique known as Hypopressive Breathing to reduce intra-abdominal pressure and optimize organ position. The term Hypopressive means “low pressure”. Traditional exercise, core training, sports, and most of our everyday activities are Hyperpressive – they increase the pressure in the abdomen. When the pressure in the abdomen is not appropriately managed, pressure increases, and this causes the spine to compress and the organs (especially the uterus) to move downward and away from their optimal “centered” position. But when the hypopressive breath is triggered, the pressure in the abdomen is reduced, the spine decompresses, the core musculature is gently strengthened, all of the organs lift, and the uterus is centered.
When the uterus is centered, magic happens… the fascial tension in the pelvis balances out; the resting tone of the abdominal and pelvic muscles improve and become easier to strengthen; the blood flow and lymphatic circulation in the pelvis is improved and sexual function and fertility is enhanced; hormones are better regulated and monthly cycles regulate; bowel and bladder function is optimized; the waistline reduces; pain in the back, abdomen and hips is reduced and posture improves. When all of these wonderful things occur, it is directly associated with improved energy, mood, creativity and self confidence. So remember, centering the uterus, through both active and passive techniques, is key when treating any woman. Self abdominal massage followed up by Low Pressure Fitness® are the most powerful techniques I have found to center the uterus and resolve pelvic and core dysfunction in women of all ages and lifestyles.
Dr. Nicole Cozean was just awarded the IC/BPS Physical Therapist of the Year by the IC Network, one of the largest patient advocacy groups for interstitial cystitis! Today she shares her treatment approach for this complex dysfunction. Join Dr. Cozean in San Diego on April 28-29, 2018 to learn everything there is to know about interstitial cystitis.
Interstitial cystitis (IC) is a chronic pelvic pain condition characterized by pelvic pain and urinary urgency/frequency. IC is frequently accompanied by other symptoms1, including painful intercourse, low back or hip pain, nocturia, and suprapubic tenderness.
While pelvic floor physical therapy is the most proven treatment for interstitial cystitis, most patients require a multi-disciplinary approach for optimal results. The majority are forced to develop this holistic approach on their own, but one of the most valuable things a physical therapist can provide is assistance in creating their own unique treatment plan. The American Urological Association has released treatment guidelines for interstitial cystitis, and potential treatments fall into several different categories. It is important to note that most treatments aren’t effective for the majority of patients, so a trial-and-error approach is needed to find the right balance for each patient. Tracking symptoms with a weekly symptom log can be a powerful tool to optimize the individual treatment plan.

Summary of the AUA Guidelines for IC – Download Here
Oral Medications
Oral medications are primarily used to reduce pain.Anti-depressants can dampen the nervous system, decreasing the severity of pain reported. Anti-histamines have also been shown to be effective in reducing the pain and symptoms of interstitial cystitis, perhaps because of their ability to reduce inflammation and break the cycle of dysfunction-inflammation-pain (the DIP cycle). Some patients require opioid painkillers for adequate pain control.
Urinary tract analgesics can provide temporary pain relief for some patients, but cannot be taken consistently because they thicken the urine and strain the kidneys. Some patients find success using these medications (Azo, Pyridium, Uribel) during severe pain flares.
The only FDA-approved oral treatment for interstitial cystitis is Pentosan Polysulfate (PPS, Elmiron®). This is commonly prescribed to patients after an IC diagnosis, but has been shown to be effective in only 28-32% of patients. It also requires a long time (often 6-9 months) to build up in the system and take effect, and many patients stop taking the drug before they could see effect because of side effects (including hair loss) or cost. Unfortunately, many patients lose more than a year after their initial diagnosis waiting to see if Elmiron will work for them, when it is unlikely to provide complete relief.
Antibiotics should never be prescribed for IC in the absence of a confirmed infection.
Bladder and Medical Procedures
Bladder instillations deliver numbing medication directly to the bladder through a catheter and can provide temporary pain relief for some patients. If these are effective, they typically are repeated at least weekly as symptoms return. Some patients don’t tolerate the catheterization well, finding the procedure causes more pain than it prevents. Typical bladder instillations consist of Lidocaine, Heparin, or a combination of the two.
Another route of treatment works by artificially stimulating the nerves the innervate the bladder and pelvic floor.Percutaneous tibial nerve stimulation (PTNS) directs electrical impulses from the ankle up through the pelvic floor. This is an outpatient procedure typically performed weekly for a course of 12 weeks. A more permanent option is implanting a device under the skin of the buttock to target the sacral or pudendal nerve root directly.With this procedure, the patient is given a ‘trial run’ with an external device to see how it performs. If significant improvements are noted, the device can be permanently implanted.
Many patients see marked improvement in their symptoms with a home care program. Deep breathing or meditation can calm the nervous system and reduce the amplifying effect of an upregulated nervous system. A stretching regimen targeting the inner thighs, glutes, abdomen, and pelvic floor can relax muscles and reduce nerve irritation in the region. Self-massage can find and eliminate the trigger points that are causing symptoms. Home tools like a foam roller can address external trigger points, while patients can be taught internal self-release with the help of a tool like the PelviWand or another tool.
Elimination Diet
One of the most common misunderstandings about IC centers on the ‘IC Diet.’ In fact, there’s no such thing. While nearly 90% of IC patients report that diet influences their symptoms in some way, the scope and severity of dietary triggers varies greatly between patients. There are a few common culprits - coffee, tea, citrus fruits, artificial sweeteners, tomatoes, cranberry juice - but no guarantee that a patient will be sensitive to all (or any) of these. Many patients read about an ‘IC Diet’ online after receiving their diagnosis, and are convinced that they need to cut out a huge portion of their diet.
Instead, they should be doing an elimination diet focused on identifying their trigger foods.With this approach, they eliminate most of those common culprits and see how it affects their symptoms.If they notice an improvement, they can gradually add foods back into their diet, one at a time, until they see symptoms increase again. This allows patients to identify their specific trigger foods.
Our advice for IC patients is simple - avoid your trigger foods and eat healthy. It doesn’t have to be any more restrictive than that.
There are also several supplements that have shown benefit for patients, either in clinical trials or anecdotally. Prelief (calcium glycerophospate) is an antacid that may reduce the consequences of eating a trigger food. L-Arginine is a semi-essential amino acid that facilitates blood flow and vasodilation; in clinical trials it was shown to be effective for nearly 50% of patients in reducing pain and urinary symptoms. Aloe Vera pills are used by many patients, and thought to help replenish the bladder’s protective layer. Finally, a combination of supplements known as Cystoprotek is also a common supplement taken by IC patients, combining anti-inflammatory flavonoids with molecules that may reinforce the bladder lining.
Complementary and Alternative Medicine
Acupuncture has been shown to provide relief for pelvic pain patients2, with 73% of men with chronic prostatitis (either identical or closely related to IC) reporting improvement. These men received two treatments weekly for six weeks, focusing around the sacral nerve. Women with pelvic pain and painful intercourse have also reported improvements in pain with 10 sessions of acupuncture3.
Cognitive-Behavioral Therapy (CBT) has been shown to help reduce pain in conditions as diverse as cancer, low back pain, and pelvic pain. In pelvic pain, ten one-hour sessions of CBT was shown to provide significant benefit for nearly half of patients4. Supportive psychotherapy was also shown to have benefits for pelvic pain patients.
A multi-disciplinary approach provides the best results for patients. Physical therapists, who see our patients regularly, can be a great resource in suggesting additional treatment options. The American Urological Association IC Guidelines can be an important resource in guiding patients to other options and developing their unique treatment plan.
Information and Resources
For additional patient resources available for download, feel free to visit The IC Solution page.. In our upcoming course for clinicians treating interstitial cystitis (April 28-29, 2018 in San Diego), we’ll focus on the most important physical therapy techniques for IC, home stretching and self-care programs, and information to guide patients in creating a holistic treatment plan.
1. Cozean, N. "Pelvic Floor Physical Therapy in the Treatment of a Patient with Interstitial Cystitis, Dyspareunia, and Low Back Pain: A Case Report". Journal of Women's Health Physical Therapy. 2017
2. Chen R, Nickel JC. "Acupuncture ameliorates symptoms in men with chronic prostatitis/chronic pelvic pain syndrome"Urology. 2003 Jun;61(6):1156-9; discussion 1159.
3. Schlaeger, J, et al. "Acupuncture for the Treatment of Vulvodynia: A Randomized Wait‐List Controlled Pilot Study". Journal of Sexual Medicine. 30 January 2015. https://doi.org/10.1111/jsm.12830
4. Masheb, et al. "A randomized clinical trial for women with vulvodynia: Cognitive-behavioral therapy vs. supportive psychotherapy". PAIN® Volume 141, Issues 1–2, January 2009, Pages 31-40
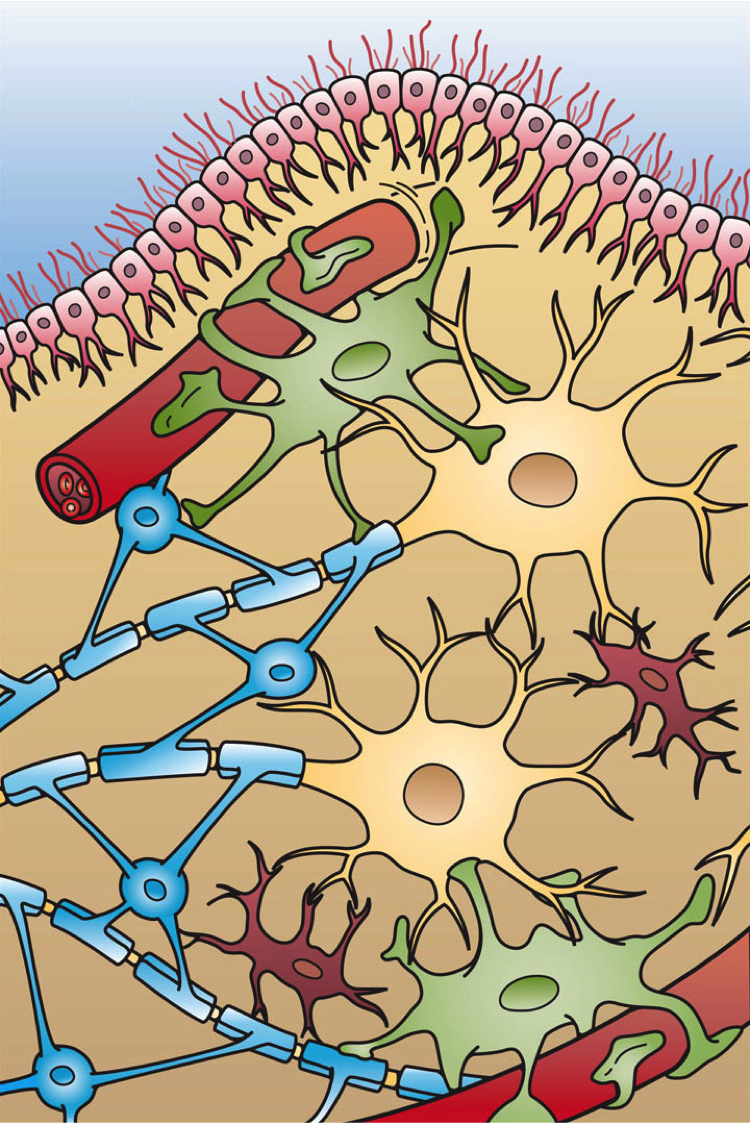
There has been a bit of buzz on the various news outlets and social media feeds about the “new organ” the interstitium. On March 27th an article appeared in Scientific Reports, an online peer-reviewed journal from the publishers of Nature. This work was presented by a team of researchers that utilized a new in vivo laser endomicroscopy technique that demonstrated this tissue is a matrix of collagen bundles and elastic fibers surrounded by fluid rather than the tightly packed layers of connective tissue that was previously observed on fixed slides . This submucosal layer was observed in the entire gastrointestinal tract, the urinary bladder, bronchus, dermis, bronchus and peri-arterial soft tissue and fascia. The authors state, “In sum, we describe the anatomy and histology of a previously unrecognized, though widespread, macroscopic, fluid-filled space within and between tissues, a novel expansion and specification of the concept of the human interstitium” Benias et al., 2018.
 The only thing ‘new’ is the way that this group of scientists observed the tissue that until now has primarily been studied ex vivo. I find it rather humorous to note that it is mainstream news that histologists in the 21st century just realized that there is a difference in the architecture of living versus dead tissue. They noted a significant change in the appearance of tissue slides that were chemically fixed in the traditional manner when compared to studies of in vivo structures as well as fresh frozen samples. The researchers noted this tissue in the dermis as well as urinary system, gastrointestinal system and respiratory system. This further supports one of my favorite talking points presented in the visceral mobilization courses “fascia is fascia is fascia is fascia.”
The only thing ‘new’ is the way that this group of scientists observed the tissue that until now has primarily been studied ex vivo. I find it rather humorous to note that it is mainstream news that histologists in the 21st century just realized that there is a difference in the architecture of living versus dead tissue. They noted a significant change in the appearance of tissue slides that were chemically fixed in the traditional manner when compared to studies of in vivo structures as well as fresh frozen samples. The researchers noted this tissue in the dermis as well as urinary system, gastrointestinal system and respiratory system. This further supports one of my favorite talking points presented in the visceral mobilization courses “fascia is fascia is fascia is fascia.”
As an instructor that presents entire courses around the importance of the fascial system within all structures of the body including the dermis, epimysium, all organs, and the adventitia of vessels, I am thrilled to see this layer of the fascial system receive recognition and garner the attention it deserves. However, to refer to the interstitium as a new undiscovered organ is to ignore the work of the International Fascia Research Congress as well as many other notable scientists. These researchers see the fascial system as the dynamic mesenchymal tissue that unites every cell in the body and allows for fluid and tissue movement.
French hand surgeon Dr. Jean-Claude Guimrberteau has documented this tissue utilizing microendoscopy on living subjects for the past 20 years. Dr Guimberteau created a brilliant DVD called Strolling Under the Skin, you can view an excerpt available on YouTube. Following the success of several videos, he went on to co-author the book Architecture of Human Living Fascia: The extracellular matrix and cells revealed through endoscopy.
Another brilliant researcher is Orthopedic Surgeon Dr. Carla Stecco. Her paper The Fascia: the forgotten structure is an excellent review of the three-dimensional continuity of the myofascia. Following multiple publications, she also authored the book The Functional Atlas of the Human Fascial System. Her work is limited to the myofascial layer and does not include the visceral fascia although she notes its presence in her published works. For those that would like to know more about this tissue, I highly recommend both of these authors. If you wish to explore how a physical therapist can utilize this information in clinical practice, join me for one of my courses on fascial manipulation. The fascial based treatment for pelvic dysfunction series includes:
- Mobilization of the Myofascial Layer: Pelvis and Lower Extremity
- Mobilization of Visceral Fascia: The Gastrointestinal System
- Mobilization of Visceral Fascia: The Urinary System
- Mobilization of the Visceral Fascia: The Reproductive System of Men and Women
Benias, P. C., Wells, R. G., Sackey-Aboagye, B., Klavan, H., Reidy, J., Buonocore, D., ... & Theise, N. D. (2018). Structure and Distribution of an Unrecognized Interstitium in Human Tissues. Scientific Reports, 8(1), 4947. https://:doi.org/10.1038/s41598-018-23062-6, 2018.
Stecco, C., Macchi, V., Porzionato, A., Duparc, F., & De Caro, R. (2011). The fascia: the forgotten structure. Italian journal of anatomy and embryology, 116(3), 127.
The Institute has welcomed occupational therapists since our founding in 2006. In addition, three OTs: Richard Sabel, MA, MPH, OTR, GCFP, Erica Vitek, MOT, OTR, BCB-PMD, PRPC, and Tiffany Ellsworth Lee MA, OTR, BCB-PMD all teach courses as members of our faculty. (Erica Vitek is also one of several OTs who holds certification as a Pelvic Rehabilitation Practitioner through H&W).
Recently, the Institute was contacted by an Occupational Therapist who has attended many of our courses, regarding a challenge she was experiencing obtaining CEUs in her state (Oregon) for courses on Pelvic Rehab and Biofeedback. In light of this, the Institute has been discussing with some of the occupational therapists on our faculty, as well as representatives of the BCIA and Marquette University, and how to spread awareness about and recognition of OT’s roles in pelvic rehab. Below, we’ve asked faculty member Erica to share a bit more about her journey and the role of the pelvic rehab occupational therapist.
 As an OT student, I had a professor who brought in practicing clinicians to discuss their unique roles out in the field. Pelvic health happened to be one of the topics of the day. I was completely intrigued by the clinician, who had such passion about the role of OT in pelvic health. It became clear that helping people with impaired basic bodily functions was imperative to fulfilling life roles and participation; it was OT. I knew from that moment that I wanted to help people deal with these challenging, private issues.
As an OT student, I had a professor who brought in practicing clinicians to discuss their unique roles out in the field. Pelvic health happened to be one of the topics of the day. I was completely intrigued by the clinician, who had such passion about the role of OT in pelvic health. It became clear that helping people with impaired basic bodily functions was imperative to fulfilling life roles and participation; it was OT. I knew from that moment that I wanted to help people deal with these challenging, private issues.
In my journey, I did not immediately start out in pelvic health, but instead in an acute care hospital that had a women’s health program with a strong interest in pelvic health. A very experienced OT and her team of 2 additional OTs were doing great work in that department already. The window of opportunity opened for me to mentor with that group and I eventually was able to begin to get my own referrals and develop a robust hospital-based outpatient practice. At that time, ALL of my experience had been with OTs doing this work and I was naïve to the fact that outside of my world, most of the clinicians doing this type of work were physical therapists (PT). I asked to join a highly trained and skilled group within my health system of all women’s health PTs. Overtime, I was able to demonstrate my level of competency within the group of PTs and contribute valuable things to our organization. Herman and Wallace Rehabilitation Institute was instrumental in my quest to demonstrate competency as they allowed OTs a clear pathway for enrollment in their coursework and application for the Pelvic Rehabilitation Practitioner Certification examination. I can be proud to have those credentials to my name.
My challenges in the area of pelvic health practice have thankfully been minimal, nearly nonexistent, and it has come to my awareness in recent weeks that this is not the case for OTs around the country trying to develop themselves as pelvic health practitioners. My original OT mentors reassured me with the AOTA’s published document titled Occupational Therapy Practice Framework: Domain & Process, detailed a clear place in the role of pelvic health. This document has gone through 3 revisions over the course of its first publication in 2002. The 2nd edition was published in 2008 and the 3rd edition in 2014. I’d like to cite a few important areas of the document that I find to be helpful in an OT’s quest to demonstrate our role in pelvic health rehabilitation.
I’d first like to quote the definition occupational therapy according to the 3rd edition, “occupational therapy is defined as the therapeutic use of everyday life activities (occupations) with individuals or groups for the purpose of enhancing or enabling participation in roles, habits, and routines in home, school, workplace, community, and other settings. Occupational therapy practitioners use their knowledge of the transactional relationship among the person, his or her engagement in valuable occupations, and the context to design occupation-based intervention plans that facilitate change or growth in client factors (body functions, body structures, values, beliefs, and spirituality) and skills (motor, process, and social interaction) needed for successful participation. Occupational therapy practitioners are concerned with the end result of participation and thus enable engagement through adaptations and modifications to the environment or objects within the environment when needed. Occupational therapy services are provided for habilitation, rehabilitation, and promotion of health and wellness for clients with disability- and non-disability-related needs. These services include acquisition and preservation of occupational identity for those who have or are at risk for developing an illness, injury, disease, disorder, condition, impairment, disability, activity limitation, or participation restriction. “
As we look closer at the framework and the definition of OT, there is clear evidence that the occupational therapist (OT) has a role in the treatment of pelvic health conditions. Importantly, occupations are defined by this document as “…various kinds of life activities in which individuals, groups, or populations engage, including activities of daily living (ADL), instrumental activities of daily living (IADLs), rest and sleep, education, work, play, leisure, and social participation.” The clearest examples of the OT’s role in pelvic health occupations within this section include: 1) ADL section: toileting and hygiene (continence needs, intentional control of bowel movements and urination) and sexual activity. 2) IADLs section: sleep participation (sustaining sleep without disruption, performing nighttime care of toileting needs). 3) Achieving full participation in work, play, leisure, and social activities, requires one to be able to maintain continence in a socially acceptable manner in which they can feel confident and comfortable to fulfill their roles and duties.
Client factors as defined in this document are “Specific capacities, characteristics, or beliefs that reside within the person and that influence performance in occupations. Client factors include values, beliefs, and spirituality; body functions; and body structures.” Client factors are further identified as affecting the performance skills and participation of the clients we work with. OT’s role per definition is to “facilitate change and growth in client factors”. In order to fully enhance our client’s performance skills/participation related to change and growth in client factors, OT’s have to examine the whole person, including pelvic health impairments, which have a negative influence on performance. Within client factors, the document defines body structures as, “Anatomical parts of the body, such as organs, limbs, and their components that support body function.” Within this category, one can refer to multiple items named that relate to the care that OTs provide in pelvic health rehabilitation, including but not limited to, structures related to the digestive, metabolic, and endocrine systems and structures related to the genitourinary and reproductive systems.
Since the first email from this individual in Oregon, we have been reached by several other OTs asking about similar challenges and questions about scope of practice. Because of our commitment to honoring the AOTA’s Practice Framework, and because we believe that the great patient need that exists can be better served by having trained OTs able to treat pelvic health conditions, the Institute is working with members of our faculty and professional network to advocate for recognition of OTs in pelvic rehab and resolve confusion about scope of practice. For those interested in further resources, please check out:
- Pelvic Floor Biofeedback
- The Women’s Health 4 OT Facebook Group
- The OTs for Pelvic Health Facebook Group
- Occupation Therapy in Postpartum Care Facebook Group
- Womens Health Occupational Therapy Australia Facebook Group
American Occupational Therapy Association. (2002). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 56, 609-639.
American Occupational Therapy Association. (2008). Occupational therapy practice framework: Domain and process (2nd ed.). American Journal of Occupational Therapy, 62, 625-683.
American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy, 68, S1-S48.
Using sEMG biofeedback to get real-time results
Tiffany Lee, MA, OTR, BCB-PMD and Jane Kaufman, PT, BCB-PMD are internationally board-certified clinicians in the treatment of pelvic floor muscle dysfunction through the Biofeedback Certification International Alliance. Combined, they have over fifty years of treatment experience using sEMG biofeedback. Their new course, “Biofeedback for Pelvic Floor Muscle Dysfunction”, will provide the nuts and bolts of this powerful tool so that clinicians can return to the clinic after this course with another component to their toolbox of treatment strategies.
 As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
So exactly what is biofeedback? Why should I consider this modality? Biofeedback provides a non-invasive opportunity for patients to see muscle function visualized on a computer screen in a way that allows for immediate feedback, simple representation of muscle function, and allows the patient and the clinician the opportunity to alter the physiological process of the muscle through basic learning strategies and skilled cues. Many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation is what helps patients really hone in on body awareness and connect all the dots. Here are a few comments that our patients have made; “I can now pay attention to my muscle while at work thanks to the visual of my muscle when sitting and standing”; “I needed to see my muscle to fully understand how to release the tension in it “; “I totally get what I need to do now that I have a clear picture of what you want”; “Seeing is believing”.
A 2017 study by Moretti, E., et al. is a great article that helps support the concept that measuring the pelvic floor electrical activity through a standard vaginal sensor is not always an option. For many patients, use of surface electrodes with peri-anal electrodes will provide the same reading and offer a more comfortable alternative for those patients who cannot use an internal sensor. This allows the clinician more opportunities to use this treatment modality with ease and assurance that the patient can learn from the visual representation of the muscle without fear of penetration from a sensor, and get great results!
In another study by Aysun Ozlu MD, et al. the authors conclude that biofeedback assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than home exercise program alone.
Herman & Wallace is offering a course for clinicians in Alexandria, Virginia this June that will answer all of your questions and concerns about this fabulous treatment tool: biofeedback! This course enables the clinician to learn and practice this valuable tool and gain knowledge about the benefits of this modality, so that treatment can begin immediately with ample opportunity for patient’s positive feedback and awareness of muscle function. Participants will experience being a biofeedback practitioner and patient (using a self-inserted vaginal or rectal sensor). Participants will be administering biofeedback assessments, analyzing and interpreting sEMG signals, conducting treatment sessions, and role-playing patient instruction/education for each diagnosis presented during the many hands-on lab experiences. Biofeedback is a powerful tool that can benefit your patient population, and add to your skill-set.
Moretti, E., Galvao de moura Filho, A., Correia de Almedia, J., Araaujo, C., Lemos, C. “Electromyographic assessment of women’s pelvic floor: What is the best place for a superficial sensor?” Neurology and Urodynamics; 2017; 9999:1-7.;
Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD, “Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence”
Advancing Understanding of Nutrition’s Role in…..Well….Everything
Gratitude filled my heart after being able to take part in the pre-conference course sponsored by the APTA Orthopedic Section’s Pain Management Special Interest Group this past February. For two days, participants heard from leaders in the field of progressive pain management with integrative topics including neuroscience, cognitive behavioral therapy, motivational interviewing, sleep, yoga, and mindfulness to name a few. It’s exciting to witness and participate in the evolution of integrative thinking in physical therapy. When it was my turn to deliver the presentation, I had prepared about nutrition and pain, I could hardly contain my passion. While so much of our pain-related focus is placed on the brain, I realized acutely the stone yet unturned is the involvement of the enteric nervous system (aka the gut) on pain and….well…everything.
Much appreciation is due to those on the forefront of pain sciences for their research, their insight, their tireless work to fill our tool boxes with pain education concepts. Neuroscience has made tremendous leaps and bounds as has corresponding digital media to help explain pain to our patients. One such brilliant 5-minute tool can be found on the Live Active YouTube channel.
What I love about this video is how intelligently (and artistically!) it puts into accessible language some incredibly complex processes. It even mentions lifestyle and nutrition as playing a role in what is commonly referred to as a maladaptive central nervous system.
"Maladaptive central nervous system"
Ok. I’ll admit, I struggle with the implications of this term. However, what doesn’t sit right with me is the concept of chronic or persistent pain being entirely in the brain as though the brain is a static entity. We know the brain to be plastic but often do not identify just how this is so.
 What about the role of our second brain…. the one with 200-600 million neurons that live in that middle part of our body (right next to / inside our pelvis)? Termed the enteric nervous system, this second brain both stores and produces neurotransmittersTurna, et.al., 2016, serves as the scaffolding of interplay between the ENS, SNS, and CNS. This ENS is home to the interface of “bugs, gut, and glial” which are “not only in anatomical proximity, but also influence and regulate each other…interconnected for mutual homeostasis.”Lerner, et.al., 2017 In fact, part of this process then directly impacts the brain. “Healthy brain function and modulation are dependent upon the microbiota’s [gut bugs] activity of the vagus nerve.”Turna, et.al., 2016. Further, “by direct routes or indirectly, through the gut mucosal system and its local immune system, microbial factors, cytokines, and gut hormones find their ways to the brain, thus impacting cognition, emotion, mood, stress resilience, recovery, appetite, metabolic balance, interoception and PAIN.”Lerner, et.al., 2017
What about the role of our second brain…. the one with 200-600 million neurons that live in that middle part of our body (right next to / inside our pelvis)? Termed the enteric nervous system, this second brain both stores and produces neurotransmittersTurna, et.al., 2016, serves as the scaffolding of interplay between the ENS, SNS, and CNS. This ENS is home to the interface of “bugs, gut, and glial” which are “not only in anatomical proximity, but also influence and regulate each other…interconnected for mutual homeostasis.”Lerner, et.al., 2017 In fact, part of this process then directly impacts the brain. “Healthy brain function and modulation are dependent upon the microbiota’s [gut bugs] activity of the vagus nerve.”Turna, et.al., 2016. Further, “by direct routes or indirectly, through the gut mucosal system and its local immune system, microbial factors, cytokines, and gut hormones find their ways to the brain, thus impacting cognition, emotion, mood, stress resilience, recovery, appetite, metabolic balance, interoception and PAIN.”Lerner, et.al., 2017
So, by process of logic, it requires little convincing to conclude that the food we eat or fail to eat directly impacts the health or dysfunction of this magnificently orchestrated system. One that directly and profoundly impacts our brain, our body, our being. And it’s a concept that our patients, our clients, ourselves, know in our gut to be true.
And it’s thanks to all the hard work of those who have come before us that we can share in the advancing understanding for the benefit of thousands who need your help, expertise and guidance. Please join me for Nutrition Perspectives for the Pelvic Rehab Therapist. The next course will be in Springfield, MO on June 23-24, 2018. Vital and clarifying information awaits you!
Live Active. (2013, Jan) Understanding Pain in less than 5 minutes, and what to do about it! https://www.youtube.com/watch?v=C_3phB93rvI Retrieved March 28, 2018.
Lerner, A., Neidhofer, S., & Matthias, T. (2017). The Gut Microbiome Feelings of the Brain: A Perspective for Non-Microbiologists. Microorganisms, 5(4). doi:10.3390/microorganisms5040066
Turna, J., Grosman Kaplan, K., Anglin, R., & Van Ameringen, M. (2016). "What's Bugging the Gut in Ocd?" a Review of the Gut Microbiome in Obsessive-Compulsive Disorder. Depress Anxiety, 33(3), 171-178. doi:10.1002/da.22454
Today's guest post comes to us from Kelly Feddema, PT, PRPC. Kelly practices pelvic floor physical therapy in the Mayo Clinic Health System in Mankato, MN, and she became a Certified Pelvic Rehabilitation Practitioner in February of 2014. To learn more about diastasis recti abdominis, consider attending Care of the Postpartum Patient!
It can be a struggle to treat patients with diastasis recti if they don't seek treatment early after giving birth. Many therapists may often find themselves thinking “if I only could have started them sooner.” Why does this condition often get missed at postpartum examinations? I personally deal with symptoms from an undiagnosed diastasis, and I'm a therapist! I didn’t really pay attention to it until I started down the road of becoming a pelvic floor therapist.
 Diastasis recti can be a difficult diagnosis to treat, as the patient may come to us when they are already one year postpartum, and not everyone agrees on the what are the best treatments. To crunch or not crunch? To use a brace or not to brace? It would be great if we had a similar healthcare system to France, where the norm is to have 10-20 postpartum rehabilitation visits with women after child birth. While therapy is available in the United States, women must ask for it.
Diastasis recti can be a difficult diagnosis to treat, as the patient may come to us when they are already one year postpartum, and not everyone agrees on the what are the best treatments. To crunch or not crunch? To use a brace or not to brace? It would be great if we had a similar healthcare system to France, where the norm is to have 10-20 postpartum rehabilitation visits with women after child birth. While therapy is available in the United States, women must ask for it.
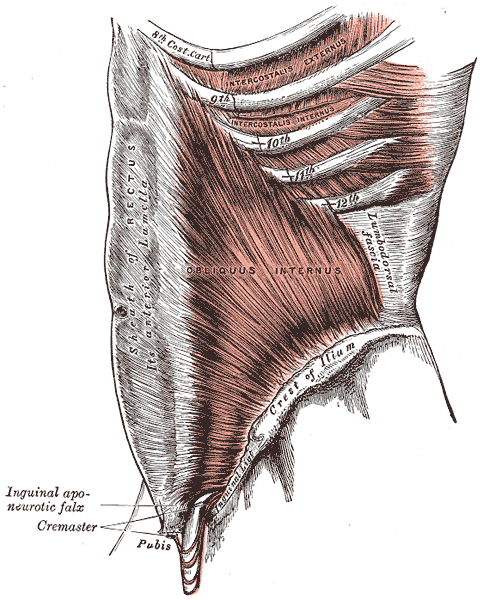
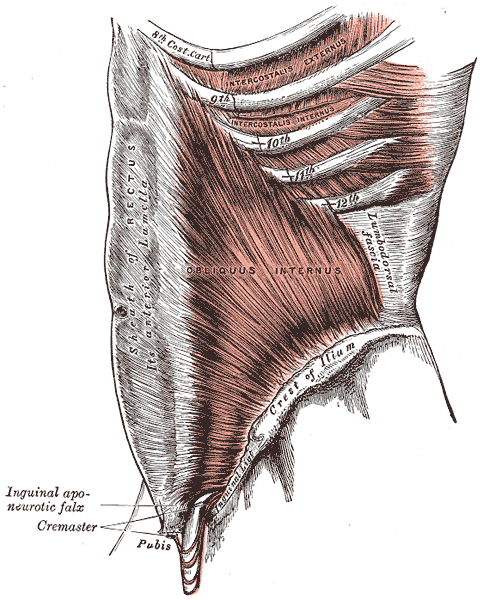
There are many programs out there from the more well-known Tupler Technique and Mutu programs to others that come up when searching for exercise ideas. The American Physical Therapy Association (APTA) has a basic program to work on isolating the transverse abdominis (TrA) muscle and then progressing movements in the legs while keeping the TrA activated.
Some research by Paul Hodges and Diane Lee from 2016 in the Journal of Orthopedic Sports Physical Therapy indicates that narrowing the inter-rectus distance with a TrA contraction might improve force transfer between the sides of the abdominals and in turn, improve abdominal mechanics.
Another study in Physiotherapy from December of 2014 by AG Pascoal, et.al. utilized ultrasound to determine the effect of isometric contraction of the abdominal muscles on inter-rectus distance in postpartum women. They found that the while the inter-rectus distance in postpartum women was understandably higher than controls, it significantly lowered during an isometric contraction of the abdominal muscles.
One year later, a study in the same journal by MF Sancho, et.al. had similar findings when studying women who had a vaginal delivery and women who had Cesarean deliveries. They found that abdominal crunch exercises were successful in reducing inter-rectus distance, but drawing-in exercises were not.
As with a lot of research, the findings lead to more questions and ideas to explore. I think it is safe to say that starting safe re-education of the muscles as early as possible is going to provide women the most benefit in reducing diastasis recti, and that will help to prevent further issues in the abdominal and pelvic region.
Sagira Vora, PT, MPT, WCS, PRPC practices in Bellevue, WA at the Overlake Hospital Medical Center, and she played a pivotal role in creating the Pelvic Rehabilitation Practitioner Certification examination. Today's post is part one of a multi-part series on pelvic rehabilitation and sexual health. Stay tuned for part two!
“Have mind-blowing sex: learn how to do your Kegels.” “Amazing orgasms, ladies do your Kegels!” These were just some of the headlines that greeted me as I researched what was being said in the popular media regarding pelvic floor exercises and improving sexual function in women. Some other wisdom from popular women’s magazines included advice on, “stopping the flow of urine,” to do your Kegels. We know how much we pelvic floor therapists love hearing that phrase!

I found a few recent and past studies that have tried to study pelvic floor exercises and sexual function in women.
In 1984, Chambless et.al. studied a small group of women who were able to achieve orgasm through intercourse less than 30% of time. Strength gains in the pubococcygeus muscles were noted in the exercise group but neither the exercise nor control group achieved increased orgasmic frequency.
In a more recent study, Lara et. al. studied 32 sexually active post-menopausal women, who had the ability to contract their pelvic floor muscles, tested the hypothesis that 3 months of physical exercises including pelvic floor muscle training with biweekly physical therapy visits and exercise performed at home three times a week, would enhance sexual function. Pelvic floor muscle strength was significantly improved post-test, but this study found no effect on sexual function.
Forty years after Dr. Kegel’s assertion about sexual arousal enhancing properties of pubococcygeus muscle exercises, Messe and Geer tested Kegel’s hypothesis in their psychophysiological study, in which they asked women to perform vaginal contractions while engaging in sexual fantasy. A second group was asked to engage in sexual fantasy without the contractions, and yet a third group was given the task of vaginal contractions but no sexual fantasy. The results indicated that performing vaginal contractions with sexual fantasy improved arousal and orgasmic ability. Initially, this group made better gains than vaginal contractions alone and fantasizing alone. However, with a second test session one week later, no further gains were noted in the ability of this group to improve sexual arousal or orgasm. Messe and Geer speculated that increased muscle tone may result in increased stimulation of stretch and pressure receptors during intercourse, leading to enhanced arousal and orgasmic potential.
The most interesting finding was reported by an older study done by Roughan, who reported no differences in the groups he studied. Roughan et. al. expected women with orgasm difficulties to improve after 12-week period of pelvic floor strengthening exercises, compared to a group that practiced relaxation and an attention control group. No difference was found between the orgasmic ability of the two groups.
The majority of women studied here had no reported pelvic floor dysfunction. Perhaps, contrary to popular opinion and against the advice of women’s magazines, women with healthy pelvic floors may not benefit from pelvic floor exercises any more than they would from relaxation training, or mindful attention to sexual stimuli.
So, what then, will increase our mojo in bed, you ask? Stay tuned for the next blogs…
Chambless D, Sultan FE, Stern TE, O’Neill C, Garrison S. Jackson A. Effect of pubococcygeal exercise on coital orgasm in women. J Consult Clin Psychol. 1984; 52:114-8
Laan E. Rellini AH. Can we treat anorgasmia in women? The challenge to experiencing pleasure: Sex Relation Ther. 2011:26:329-41
Messe MR, Geer JH. Voluntary vaginal musculature contractions as an enhancer of sexual arousal. Arch Sex Behav. 1985; 14:13-28
Padoa, Anna. Rosenbaum, Talli. 1st edition. 2016. The Overactive Pelvic Floor.
Roughan PA, Kunst L. Do pelvic floor exercises really improve orgasmic potential? J Sex Marital Ther. 1984;7:223-9
As practitioners, we understand the value of a yoga practice for multiple systems. Yoga improves cardiovascular function, pulmonary function, improves flexibility, builds strength, improves balance, and cultivates resiliency. Prenatal yoga is deemed safe and widely practiced. Beyond not laying prone after the first trimester, what are modifications for practicing yoga while pregnant? Is there any evidence to demonstrate if specific yoga postures are safe from both the maternal and fetal perspective?
 Polis et al set out to determine the safety of specific yoga postures using vital signs, pulse oximetry, tacometry, and fetal heart rate monitoring. The patients were diverse in age, race, BMI, gestational age, parity, and yoga experience. Exclusionary criteria included preeclampsia, placenta previa, bleeding in the 2nd or 3rd trimester, gestational diabetes, BMI greater than 35 and other medical conditions that presented contraindications.
Polis et al set out to determine the safety of specific yoga postures using vital signs, pulse oximetry, tacometry, and fetal heart rate monitoring. The patients were diverse in age, race, BMI, gestational age, parity, and yoga experience. Exclusionary criteria included preeclampsia, placenta previa, bleeding in the 2nd or 3rd trimester, gestational diabetes, BMI greater than 35 and other medical conditions that presented contraindications.
The maternal and fetal responses were tested in 26 yoga postures. The selected postures, much like most yoga classes, offered a variety of physical positions. The standing, seated, twists and balancing postures chosen were: Easy Pose, Seated Forward Bend, Cat Pose, Cow Pose, Mountain Pose, Warrior 1, Standing Forward Bend, Warrior 2, Chair Pose, Extended Side Angle Pose, Extended Triangle Pose, Warrior 3, Upward Salute, Tree Pose, Garland Pose, Eagle Pose, Downward Facing Dog, Child’s Pose, Half Moon Pose, Bound Angle Pose, Hero Pose, Camel Pose, Legs up the Wall Pose, Happy Baby Pose, Lord of the Fishes Pose and Corpse Pose.
Balancing postures were modified to decrease fall risk. Warrior 3, Tree Pose, Eagle Pose, and Half Moon Pose were performed at the wall or using a chair for support. The addition of a yoga block to bring the floor closer to the practitioner was used for Extended Side Angle Pose, Extended Triangle Pose, and Garland Pose.
Four poses that have previously been theorized to be contraindicated were studied in this group. These postures are Child’s Pose, Corpse Pose, Downward Facing Dog, and Happy Baby. No adverse reactions were discovered for this specific population during the intervention or in the 24 hour follow-up as reported by email.
Now that we have this data, what do we do with it?
We have the opportunity to educate our non-high-risk patients that the previously theorized contraindicated postures listed above were safe for the self-selected group in this study. Those who are in high-risk categories should understand that even though yoga is not a high impact activity, there should be clearance from the OB team to ensure expectant mothers are moving as safely as possible. With proper guidance, yoga is a safe form of exercise and stress reduction which can optimize physical and mental health during the prenatal period and prepare for birth.
Dustienne Miller is the author and instructor of Yoga for Pelvic Pain. Join her in Kansas City, MO on April 7, 2018 - April 8, 2018 to learn about treating interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia with a yoga approach.
Polis RL, Gussman D, Kuo YH. Yoga in Pregnancy. Obstet Gynecol 2015;126:1237–41
A 2016 study by Kaori et al examined the effect of self administered perineal stimulation for nocturia in elderly women. A prior study using rodents found a soft roller used decreased overactive bladder syndrome (OAB), but a hard roller did not produce the same results. Kaori et al performed a similar study for elderly women in a randomized, placebo controlled, double blind crossover. Participants were 79-89 years old women who applied simulation to perineal skin for 1 minute at bedtime, using either active (soft, sticky elastomer) roller or a placebo (hard polylestrene roller). Participants did a 3-day baseline, followed by 3-day stimulation, then 4 days rest, then other stimuli for 3 days. There were 24 participants, 22 completed the study: 9 with OAB, 13 without OAB. The placement of the roller was not on the skin of the perineal body, but rather on the general peri-anal area with the diagram from the study showing an area just medial to the gluteal crease—where one would find the ischial tuberosity-- and anterior and lateral to the anal sphincter.
 Across the subjects with OAB, change with the elastomer roller (soft and sticky feel) was more statistically significant than with the hard roller. Baseline micturition for the participants was 3.2+/- 1.2 times per night, measured as the number of urination between going to bed and arising. The group as a whole did not have a statistically significant difference, measured by at least one less time arising per night. However, in the OAB group, the difference was significant. The researchers theorized that the soft and sticky texture may induce more firing of somatic afferents nerve fibers.
Across the subjects with OAB, change with the elastomer roller (soft and sticky feel) was more statistically significant than with the hard roller. Baseline micturition for the participants was 3.2+/- 1.2 times per night, measured as the number of urination between going to bed and arising. The group as a whole did not have a statistically significant difference, measured by at least one less time arising per night. However, in the OAB group, the difference was significant. The researchers theorized that the soft and sticky texture may induce more firing of somatic afferents nerve fibers.
The most commonly prescribed treatment for overactive bladder is anticholinergic therapy, but the side effects, including cognitive changes and lack of significant difference from controls, as well as the drying effect of these drugs in a post-menopausal-low-estrogen-pelvis, bring up questions of whether this is the best option in the elderly.(6)
In anesthetized animals, electrical stimulation and noxious stimuli decrease frequency of bladder contractions when applied to the perineal area (3-5). Somatic, afferent nerve stimuli (those theorized to be active with the soft roller) are used to treat OAB by modalities such as acupuncture and transcutaneous electrical stimulation to the perineum (2). So, stimulation of somatic visceral afferent nerves in the perineal region seems to have an effect on the bladder. However, with manual therapies, it seems we can also affect the somatic or visceral afferents. Essentially, visceral afferents convey information to the central nervous system about local changes in chemical and mechanical environments of a number of organ systems(7). Doing manual therapy between the urethral and bladder fascia would also theoretically cause stimulation of the visceral afferents to the central nervous system about that organ (bladder).
In our pelvic floor intro class (Pelvic Floor Level 1) at Herman Wallace, we discuss the role of Bradley’s neurology loop 3 and the inverse relationship between pelvic floor contraction (lifting the perineal area) and the bladder. One suppression technique we discuss is the contraction of the pelvic floor to quiet or inhibit bladder activity in the bladder retraining program. Bladder retraining has evidence level A (strong) for improving urgency and frequency with overactive bladder.
Clinicians who are ready to raise their manual game may try using the skills of prior series courses and adding the sophistication of manual techniques in the abdomen and pelvis to increase afferent firing in patients with OAB, as well as freeing up any fascial restrictions that may be interfering with full bladder excursion.
In the newly written Capstone course, we combine the prior level of education from the pelvic series (bladder strategies) with manual techniques to address the endopelvic fascia at the bladder base, in the fascial articulations along the perineum, and along its attachments to the coccyx, as well as combining internal work with sacral techniques to facilitate S234 afferents for bladder control. We discuss studies, such as this one, to explore advanced concepts of bladder and urethral fascial mechanics and neural entrapment affecting the bladder. We move out of the pelvic muscle and into the fascial contents of the abdominopelvic region, to allow such firing of the somatic afferents. And the perineal stimulation? We have an entire lab for perineal tissue and its effect on pelvic function. Physical therapists can manually address the perineum, urethral and bladder fascia with Capstone techniques. With such intervention, we get more CNS communication.
So, what about the roller? Well, the soft roller created change in rodents in a couple of studies. (Sato 2010). In this human study, it helped with OAB. Certainly, manual therapies in the region of the endopelvic fascia and suprapubic region may be of help for also stimulating the visceral afferents. Also, it could be worth it to have a high fall risk elderly patient with OAB type nocturia follow up your treatments with one minute of soft washcloth stroking in the area of the perineum for one minute at bedtime to see if it helps decrease the number of voids on a night time bladder diary.
Nari Clemons, PT, PRPC is a Herman & Wallace faculty member who helped author the Pelvic Floor Series Capstone: Advanced Topics in Pelvic Rehab course. She is also the creator and instructor of Pelvic Nerve Manual Assessment and Treatment.
Main study: PLoS One. 2016 Mar 22;11(3):e0151726. doi: 10.1371/journal.pone.0151726. eCollection 2016.Effects of a Gentle, Self-Administered Stimulation of Perineal Skin for Nocturia in Elderly Women: A Randomized, Placebo-Controlled, Double-Blind Crossover Trial.Iimura K1,2, Watanabe N2, Masunaga K3, Miyazaki S1,2,4, Hotta H2, Kim H5, Hisajima T1,4, Takahashi H1,4, Kasuya Y3.
2. Exp Ther Med. 2013 Sep;6(3):773-780. Epub 2013 Jul 9., Acupuncture for the treatment of urinary incontinence: A review of randomized controlled trials.Paik SH1, Han SR, Kwon OJ, Ahn YM, Lee BC, Ahn SY.
3. Guo ZF. Transcutaneious electrical nerve stimulation in the treatment of patients with poststroke urinary incontinence. Clin Interv Aging. 2014; 851-6.
4. Sato A, The impact of somatosensory input on autonomic functions. Reve Physiol Biochem Pharmacol. 1997;130;1-328
5. Sato A. Mechanism of the reflex inhibition of micturition conractions of the urinary bladder elicited by acupuncture-like stimulation in anesthetized rats. Neurosci res. 1992 15:189-98
6). Effects of a Gentle, Self-Administered Stimulation of Perineal Skin for Nocturia in Elderly Women: A Randomized, Placebo-Controlled, Double-Blind Crossover Trial. Iimura K, Watanabe N, Masunaga K, Miyazaki S, Hotta H, Kim H, Hisajima T, Takahashi H, Kasuya Y. PLoS One. 2016 Mar 22;11(3):e0151726. doi: 10.1371/journal.pone.0151726. eCollection 2016.
7) John C. Longhurst, Liang-Wu Fu, in Primer on the Autonomic Nervous System (Third Edition), 2012